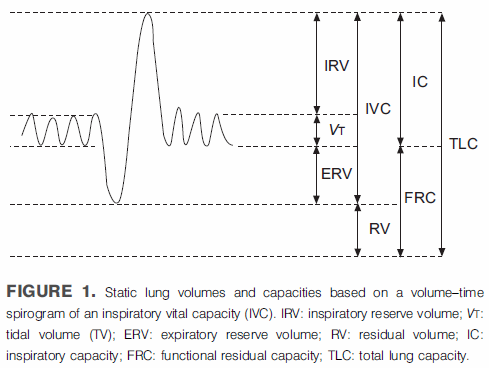
I have been searching through Pulmonary Function videos on YouTube in order to find ones I thought would be useful for technician education. So far what I’ve found have been intended either for medical students or for patients and not, in my opinion, particularly suitable for training technicians. Lately I’ve been looking at videos about lung volumes and have seen a half dozen presenters describe lung volume subdivisions using the same graph we’ve come to know and love with varying degrees of effectiveness and obfuscation.
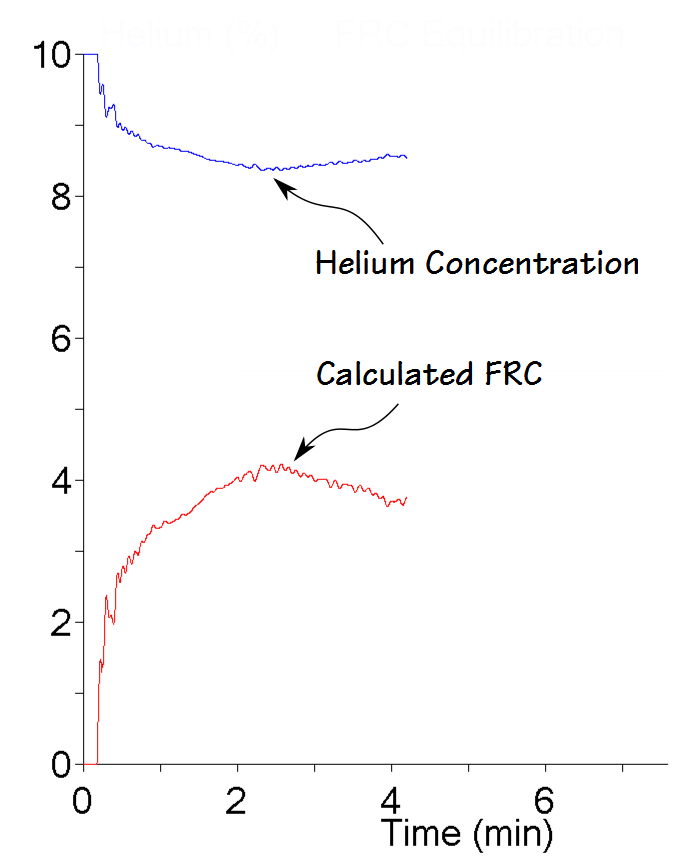
In a discussion of helium dilution lung volume measurements one of the presenters made an interesting statement and that was that “helium does not pass the alveolar-capillary barrier which means it stays inside the lungs during the test”. This is wrong on multiple levels. First, the alveolar-capillary membrane evolved for gas exchange and does not discriminate against individual gases so there is no barrier. Second, the reason that gases can be used as tracer gases or as probes of pulmonary circulation has entirely to do with gas solubility. Third, since it was a university-sponsored video with other egregious errors (for example did you know that lung volumes are measured in ml/kg?) what the heck are they teaching their medical students?
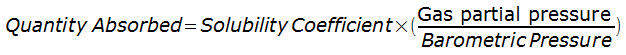
Gases can and will be absorbed by blood and tissue. The quantity of gas that can be absorbed is determined by the gas’s solubility and the Bunsen solubility coefficient is a measure of how much gas is absorbed (usually in milliliters of gas per milliliter of liquid) when the gas is at 1 atmosphere of pressure. When there is a multi-gas mixture, the quantity of gas absorbed for individual gas is calculated by: