The manager of a nearby PFT Lab made an interesting statement recently, and that was that DLCO measurements made with a sample balloon were superior to those made with a real-time gas analyzer. I think that he is biased to some extent by the fact that the manufacturer of his lab’s testing systems only supports the sample balloon approach to DLCO testing and so that is what he is used to. The same can be said of me however, because all of my lab’s equipment performs DLCO tests using real-time gas analysis and that is what I am used to.
I think that each approach has some benefits and some weaknesses but I’ll start first with a bit of background. When the single-breath DLCO test was standardized in more-or-less it’s current form in the mid-1950’s, the only gas analyzers available at that time were slow. They required relatively large samples of gas (>100 ml) and took over 10 seconds to settle to their final reading. The only way to perform the DLCO test was to capture a sample of alveolar gas and then analyze the entire sample.
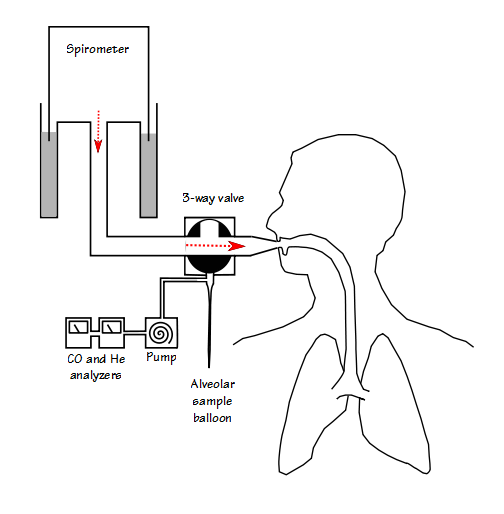
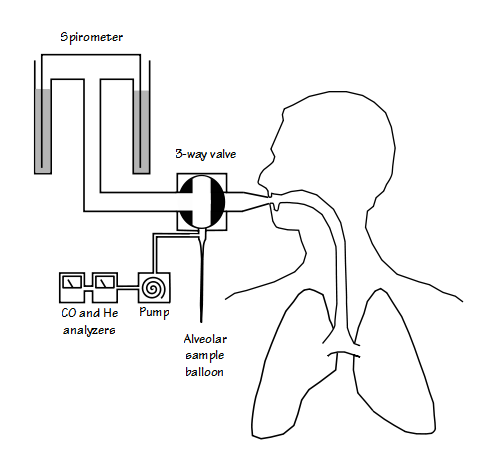
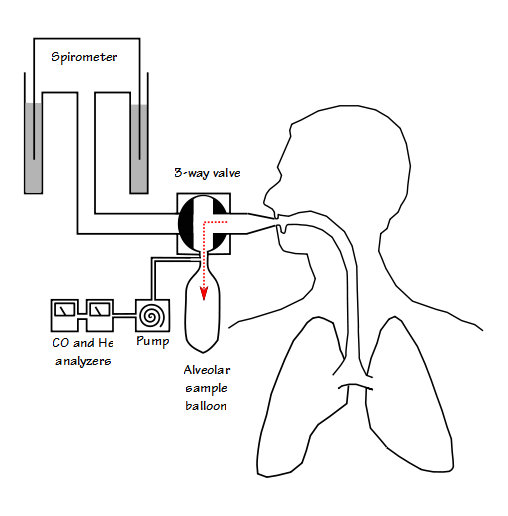
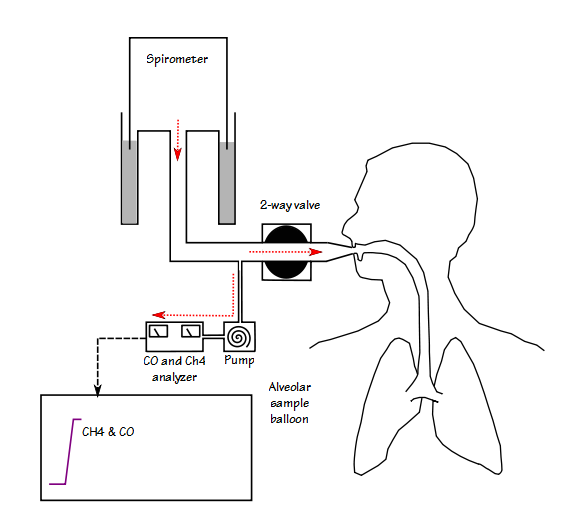
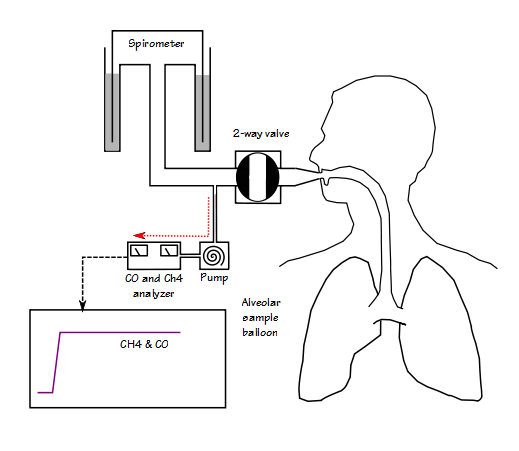
In a very simplified view, a sample balloon DLCO system works something like this:
Real-time sampling of exhaled DLCO gas was first attempted in the 1960’s using a mass spectrometer. Because carbon monoxide and nitrogen have essentially the same mass (~28), the CO gas component had to use an isotope of Oxygen, O18. This gas mixture was horrendously expensive (in the late 1970’s my lab bought a large cylinder of 0.1% CO18 in air for a research project and it cost $7000 at that time) which made this approach impractical for routine clinical use. In the early 1990’s a rapid-responding infrared analyzer capable of measuring CO and methane (CH4, a relatively insoluble gas that could take the place of helium) was developed and by the mid-1990’s several equipment manufacturers offered real-time DLCO measurements.
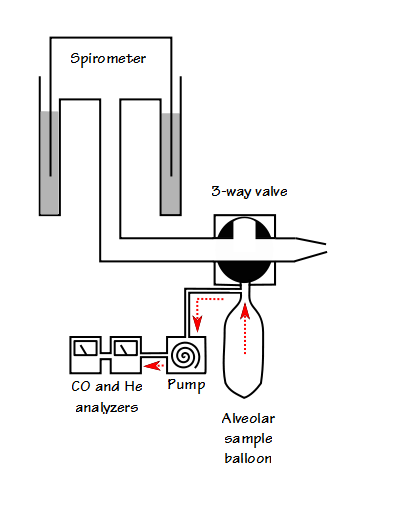
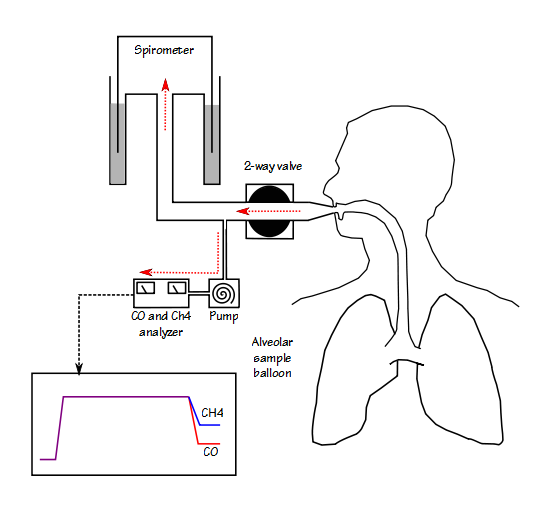
In a very simplified view, a real-time DLCO system works something like this:
For the majority of patients either system is capable of obtaining accurate DLCO test results. It is for the more marginal patients, those with very severe restrictive or obstructive lung disease, that the sample balloon system shows its limitations. The most significant disadvantage of the sample balloon system is that the washout volume must be set in advance. For patients with small vital capacities it can be difficult to get an alveolar sample that does not contain at least some deadspace gas while at the same time getting a sample volume that is large enough to analyze accurately. The ATS-ERS specifications for DLCO testing states that the washout volume should be reduced to 0.50 L (it’s normally 0.75 – 1.00 L) when the patient’s vital capacity is less then 2.00 liters. I am sure that most test systems will automatically default to the appropriate washout volume but that only applies if a vital capacity test has already been performed. In addition the ATS-ERS specifications also states that if the patient’s vital capacity is less than 1.00 L, then the washout volume can be reduced even further but they do not indicate how much further it could or should be reduced. All of this implies that a technician should be able to override the default washout volume settings but whenever they do it is going to be an educated guess at best and there is nothing in the results of the alveolar gas analysis that will indicate how successful the washout setting was.
Because a real time DLCO system allows a technician to inspect the exhaled gas waveforms, the washout and sample volume can be selected after the test has been performed. This, I believe, allows for more accurate testing on patients with marginal vital capacities. Having said that, all equipment manufacturers that I am familiar with display the exhaled DLCO gas waveforms as concentration versus time and I think this is a mistake. Because there is no indication of washout or sample volume when the results are displayed this way it is possible to mistake a point where the patient slowed or stopped their exhalation as the alveolar plateau or to select to a very small sample volume that may not be truly representative. I personally think that washout and sample volume are more important to DLCO test quality than breath-holding time and for this reason I think that the analyzer results should be displayed as concentration versus exhaled volume.
The fact that the gases in an alveolar balloon are usually well mixed is a possible advantage for that type of system. Real-time systems must depend on software to average results from the alveolar sample and this makes them dependent on whether or not a technician has selected the right alveolar sample and that the equipment manufacturer has developed the correct algorithm for this purpose.
Note: This is an aspect to present-day Pulmonary Function testing where I have a number of concerns. I understand that equipment manufacturers have invested significant resources in developing their software and have every reason to want to keep it proprietary. At the same time, the accuracy of the test results we report depend on this proprietary software and its hidden algorithms. Manufacturers can state that their equipment meets all ATS-ERS standards but we have almost no way to verify this and every time I have raised valid concerns about errors I have had a great deal of difficulty getting an answer. This is in part due to the fact that software has become so complex that finding the engineer or programmer responsible for the algorithm in question or even determining which algorithm is the one in question is difficult. I also know of situations where PFT software was developed by contract programmers who were let go when the project was completed and now there is no one left that knows what’s in the software. Although I believe that all manufacturers should make the critical algorithms in their software open to inspection, they are unlikely to do this on their own. I am not a fan of government regulation but like inspecting drugs and milk for purity this is an area where it may be necessary. Alternatively, the ATS-ERS or a manufacturers group could develop a set of open source algorithms for critical testing functions and allow anybody to adopt them. I am open to suggestions.
The fact that the alveolar sample is mixed inside a sample balloon can also be looked at as a potential disadvantage. A sample balloon will always contain a small amount of machine deadspace gas (probably on the order of 10-20 cc) from the test system’s valves (more if the sample balloon was not completely evacuated before the test). Although the amount deadspace gas is small this will affect the final concentration of the alveolar sample and the degree to which this affects the gas concentrations will depend on the actual sample volume which is usually unknown. Because a real time system continuously samples a patient’s exhaled air there is essentially no machine deadspace to contaminate an alveolar sample.
An advantage to sample balloon systems is that they are primarily mechanical in nature and the gas analyzers are relatively simple. This tends to make them less expensive and probably more physically robust than real-time systems. This is not to say they don’t have their share of problems since they are just as prone to leaks, sticking valves and pump failures as real time systems but if I had to place a test system in a remote location where service was difficult, then an alveolar balloon system may be a better choice.
Many factors go into choosing test systems including ease of use, accuracy, cost and durability, and even then some labs are “locked in” to manufacturers that may not offer this choice in the first place. For me it comes down to the fact that real time DLCO systems are more capable of getting accurate test results on marginal patients and that this reason alone makes them a better choice. There is no reason to believe, however, that either approach produces more accurate results for the majority of patients. It could be argued that the results of extremely marginal patients are questionable regardless of which approach is used to measure their DLCO but I think the number of confounding factors are greatly reduced with real time systems and regardless of the questions I have about the software driving them I believe they are inherently superior.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standisation of lung function testing. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 2005; 26: 720-735.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.