When I review the results from a CPET I am used to considering a maximum minute ventilation (Ve) greater than 85% of predicted as an indication of a pulmonary mechanical limitation. Recently a CPET report came across my desk with a maximum minute ventilation that was 142% of predicted. How is this possible and does it indicate a pulmonary mechanical limitation or not?
It is unusual to see a Ve that is greater than 100% of predicted. We derive our predicted max Ve from baseline spirometry and calculate it using FEV1 x 40. We have tried performing pre-exercise MVV tests in the past and using the maximum observed MVV as the predicted maximum Ve but our experience with this has been poor. Patients often have difficulty performing the MVV test correctly and realistically even if it is performed well the breathing maneuver used during an MVV test is not the same as what occurs during exercise. Since both Wasserman and the ATS/ACCP statement on cardiopulmonary exercise testing recommend the use of FEV1 x 35 or FEV1 x 40 as the predicted maximum minute ventilation we no longer use the MVV.
There are usually only two situations where a patient’s exercise Ve is greater than their predicted max Ve. First, when a patient is severely obstructed their FEV1 is quite low and FEV1 x 40 may underestimate what they are capable of since they are occasionally able to reach a Ve a couple of liters per minute higher than we expected. Second, if the FEV1 is underestimated due to poor test quality then the predicted max Ve will also be underestimated. In this case however, the baseline spirometry had good quality, was repeatable and the results did not show severe obstruction but instead looked more like mild restriction.
| Effort 1: | Effort 2: | Effort 3: | |
| FVC (L): | 2.51 | 2.52 | 2.60 |
| FEV1 (L): | 1.86 | 1.87 | 1.95 |
| FEV1/FVC %: | 74 | 74 | 75 |
| PEF: | 6.26 | 6.46 | 6.37 |
The patient’s TLC had been 70% of predicted when measured a month previously. Despite this and the somewhat restrictive looking spirometry, the diagnosis we had been given for the CPET was Asthma. One of the more common effects that exercise usually has on an individual with asthma is Exercise Induced Bronchoconstriction (EIB). This is one of the primary reasons that we routinely perform pre- and post-exercise spirometry as part of our CPETs. Most people usually have a small increase (3%-5%) in their FEV1 following exercise. When we see a significant decrease in FEV1 (greater than 12%) following exercise we usually consider EIB to be the cause. A small number of asthmatics however, do not bronchoconstrict with exercise, they bronchodilate, and that is what this patient did.
| Pre-Exercise: | %Predicted: | Predicted: | Post-Exercise: | %Predicted: | %Change: | |
| FVC (L): | 2.60 | 57% | 4.57 | 3.02 | 66% | +16% |
| FEV1 (L): | 1.95 | 54% | 3.59 | 2.30 | 64% | +18% |
| FEV1/FVC%: | 75 | 95% | 78 | 76 | 97% | +2% |
The patient was actually rather physically fit and other than their Ve had an above-average exercise test.
| AT | %Predicted: | Peak | %Predicted: | |
| VO2 (LPM): | 1.63 | 64% | 3.01 | 118% |
| VO2 (ml/kg): | 21.2 | 61% | 39.2 | 112% |
| VCO2 (LPM): | 1.44 | 3.27 | ||
| RER: | 0.88 | 1.09 | ||
| SpO2: | 98% | 97% | ||
| PETCO2: | 37.4 | 34.1 | ||
| Ve/VCO2: | 30 | 34 | ||
| Ve (LPM): | 43.0 | 55% | 110.3 | 142% |
| Vt (L): | 1.64 | 2.57 | ||
| RR: | 26 | 43 | ||
| HR: | 123 | 71% | 171 | 99% |
| O2/Pulse: | 13.3 | 90% | 17.6 | 119% |
[In addition, the Ve-VCO2 slope from rest to AT was 27.5 and from rest to peak exercise was 30.3 both of which are normal, and the chronotropic index was 0.81 which is low normal.]
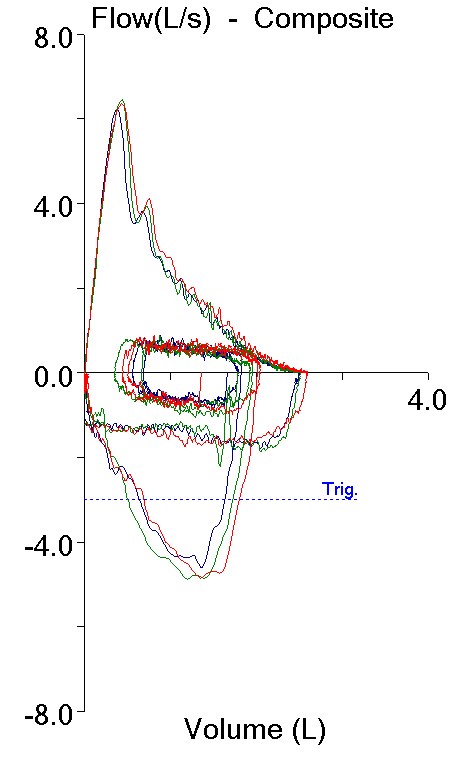
One final point is that we measure Inspiratory Capacity (IC) during a CPET in order to track a patient’s End-Expiratory Lung Volume (EELV). EELV is a surrogate for FRC and we use it to see if a patient is hyperinflating during exercise. This is a common limiting factor for patients with COPD but we routinely measure it on all of our patients (if you don’t look for it you won’t find it!). In this case, not only did this patient’s EELV decrease during exercise by 0.80 L but the maximum IC that was measured during the test was 3.30 L, which is approximately 10% greater than their post-exercise FVC and 27% greater than their pre-exercise FVC.
My take on this patient’s CPET results is that there was a markedly elevated bronchodilation response during exercise. In fact, because we perform post-exercise spirometry at least 10 or 15 minutes following exercise I strongly suspect that this patient’s post-exercise spirometry is significantly underestimating the degree to which they bronchodilated.
So was there a pulmonary mechanical limitation? Since we can’t know for sure how much the patient bronchodilated that question can’t be answered with any certainty. Even using the post-exercise FEV1 x 40, the Ve was 120% of predicted. Usually when we think of an exercise limitation, whether it is pulmonary mechanical, pulmonary vascular or cardiovascular, we are thinking in terms of something that limits or prevents a patient from achieving a normal exercise capacity. When a patient reaches a threshold for one limitation or another but still has a normal maximum oxygen consumption we usually phrase it as the patient “achieved” the limit rather than saying it was an actual limitation. I know that’s just semantics, but how else should it be described?
One final note is that the patient’s main complaint and the reason they weren’t able to go any further was leg fatigue, not shortness of breath. This fact, along with all the others, leads me to suspect that a pulmonary mechanical limit did not in fact occur.
And the low TLC? Some investigators have hypothesized that airway constriction and inflammation occurs heterogeneously in some individuals with asthma. This means that gas trapping occurs patchily all across the lung. During exhalation, these parts of the lung remain inflated and can cause further airway constriction and gas trapping in nearby parts of the lung that are not otherwise involved. This may be the reason that some asthmatics (as many as 10%?) can have a symmetrically decreased FEV1 and FVC with a normal FEV1/FVC ratio during an exacerbation. This patient’s lung volume measurements were performed using helium dilution and it is possible that heterogeneous gas trapping caused their TLC to be underestimated. Having said that there is no reason a patient can’t have both restrictive and obstructive defects simultaneously but if that was the case then this patient’s maximum VO2 of 118% of predicted is even more remarkable.
Is this asthma? In many ways this patient’s clinical course has not been typical and somewhat of a puzzle to their pulmonary physician; hence the CPET. I am not a clinician and my view may be too simplistic, but reactive airways are reactive airways even if the way they react is to bronchodilate rather than bronchoconstrict. A search of the literature indicates that bronchodilation during exercise is not all that unusual, although the degree that it appears to have occurred in this case is exceptionally large. There is a lot of research being performed on the genetics and biochemical pathways of asthma and I suspect that we will eventually find out that what we call asthma is actually just the way that a wide variety of underlying syndromes present themselves. Until that time I think that this just needs to be considered an unusual asthma variant.
Using FEV1 to predict an individual’s maximum minute ventilation does not take into consideration inspiratory flow rates. This is why FEV1 x 40 can underestimate Ve in individuals with severe airway obstruction. FEV1 can also increase during and post-exercise due to bronchodilation. When significant bronchodilation occurs, I have reported CPET results with two predicted Ve’s, one based on the pre-exercise FEV1 and one based on the post-exercise FEV1. Doing this has moved some patients from having an apparent pulmonary mechanical limit to being WNL. In this case, the patient achieved a maximum minute ventilation that was well above either predicted value. Even so I think that this helps make it clear that performing pre- and post-exercise spirometry is important not only to assess EIB but also to detect bronchodilation.
Using FEV1 x 40 to estimate an individual’s maximum minute ventilation is not perfect but it is probably better than any other approach we have at this time. When a patient’s maximum minute ventilation during a CPET exceeds what is predicted for them this can be a sign of poor baseline spirometry (or MVV) test quality or the ability of a compromised patient to slightly exceed expectations. In this case it appears to be a sign of a somewhat unusual asthmatic response to exercise.
References:
ATS/ACCP Statement on Cardiopulmonary exercise testing. Am J Resp Crit Care Med 2003; 167: 211-277.
Gelb AF, Tashkin DP, Epstein JD, Gong H, Zamel N. Exercise-induced bronchodilation in asthma. Chest 1985; 87: 196-201.
Hyatt RE, Cowl CT, Bjoraker JA, Scanlon PD. Conditions associated with an abnormal nonspecific pattern of pulmonary function tests. Chest 2009; 135: 419-424.
Wasserman K, Hansen JE, Sue DY, Stringer WW, Whipp BJ. Principles of exercise testing and interpretation, Fourth Edition, Published by Lippincott, Williams and Wilkins, 2005.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

Hello. I’m doing CPET. Tell me please how do you rate Vt (l)? For this indicator, the program does not calculate the rate. At what level of workload do you spend flow-volume loops? it depends on the level of VO2 or the onset of respiratory thresholds?
Andrey –
The first think I look for in Vt is how much of a change was there from rest to exercise? I expect to see at least a doubling. If Vt does not increase significantly, then what is the cause? Airway obstruction or restriction or odd baseline breathing pattern (high Vt, low RR) since this may affect how the ventilatory results are interpreted. If your software does not report respiratory rate (??!!) then you can calculate it by dividing the minute volume by the tidal volume.
We perform an inspiratory capacity maneuver and get flow-volume loops at baseline then every two minutes during testing. You can’t do them too often because it can bias the minute volume and the overall ventilatory response. Although some researchers have indicated that comparing the tidal volume to the maximum flow-volume loop envelope can tell you about expiratory flow limitation I haven’t really found this helpful, in particular because the tidal volume for many subjects with airway obstruction will occur outside the maximum flow-volume loop envelope. I’m more concerned about inspiratory volume and changes in the End-Expiratory Lung Volume (EELV). I also look at the inspiratory loop to see if there is any flow limitation (flattening) for all our subjects.
Regards, Richard
Thanks for the answer Richard. Respiratory rate – translation error. I do not know much English. The software does not calculate the correct values in%. Does not show the norm Vt. How sensitive is the IC (IC = inspiratory capacity) for dynamic hyperinflation of the lungs?
Andrey –
There are no normal values for tidal volume. At rest it’s nominally somewhere around 0.50 L with a minute volume of less than 12.0 LPM but that depends a lot on patient height and weight. Many subjects however, are anxious prior to testing and hyperventilate to one extent or another so you have to take the baseline values with a grain of salt. During exercise with normal subjects increases in tidal volume primarily come out of the inspiratory capacity but at higher levels of ventilation EELV decreases and IC increases. Interestingly, although it takes a bit of extra energy to dip into the ERV, this energy is mostly recovered during inhalation and so the energy cost of decreasing the EELV and increasing the IC is very low. Lung diseases, both obstructive and restrictive, can prevent a subject from decreasing their EELV, although for different reasons. IC is the only reasonable way to track EELV during exercise but getting subjects to perform the IC maneuver correctly during exercise can be difficult and this can be exacerbated by poor cuing from the technical staff. It also becomes more difficult to get an accurate IC at higher levels of exercise simply because the subject’s ventilatory drive can be very high and they don’t want to change the cadence of their breathing. When I look for changes in EELV that would indicate dynamic hyperinflation I look for a steady increase in EELV over time and don’t like to use a single measurement. An abrupt change in EELV, either + or -, usually indicates a measurement error.
Regards, Richard
Thanks for the answer Richard. In our practice we use a veloergometer. For the choice of protocol and load, we calculate the load according to the formula taking into account the growth in weight and age. the duration of testing is not always equal to 8-12 minutes. Sometimes less, but more often than 12 minutes. You could not share your formula for calculating the load and choosing the right protocol? I will check it with pleasure and write to you !!! Thank you!
Andrey –
I’d like to say that we have an official approach towards setting ergometer workload during CPETs but the reality is that we make an educated guess as to what we think the patient will be able to handle. The patients that we see for CPETs usually have a variety of known medical problems and limitations. Our CPETs are most often performed in order to determine what set of limitations is greatest (pulmonary vs cardiac) or as part of a pre-op assessment (max VO2) in order to guide treatment and rehab. Only a small number of patients are being seen because the cause of their dyspnea is unclear (the most interesting cases as far as I’m concerned). We see very few patients that would be considered to be physically fit and individuals who would be considered to be athletes only rarely. For these reasons, the predicted VO2 or workload is usually a fair bit more than what our patients can reach. Our goal is an exercise test that lasts between 5 minutes and 10 minutes and so we select the workload ramp protocol from our experience after chatting with the patient about their ability to exercise. We have workload protocols of 10, 15, 20, 25 and 30 watts/minute. The majority of our patients get the 15 watt/minute protocol. The second largest group gets the 10 watts/minute protocol. We save the 20, 25 and 30 watt/min protocols for our fit patients and athletes. We make mistakes, of course. Some patients last less time than we expect, some last more, but most of the time we seem to do okay.
Regards, Richard
Thanks for the answer Richard. In your articles, the term anaerobic threshold sounds. In the laboratory, do you determine the level of lactate in the blood? The Working Group on CPET (Westhoff M., 2013) introduced new concepts for threshold values. How do you look at it?
Andrey –
We do not use the lactate threshold because we do not use any indwelling catheters and do not collect any blood samples during exercise. Our test system uses the V-slope method to determine anaerobic threshold but I often override this. I prefer to use the nadir of the PetO2 and VeVO2 because they seem to be clearer and easier to find. I verify this as best I can with the surrounding gas exchange and ventilatory data.
The Working Group’s recommendations have not been translated to English so I have not read them. The abstract indicates that they believe there are two anaerobic thresholds and two ventilatory thresholds. Given the amount of noise in CPET data I’d be a bit skeptical about this but I’d be interested in reading it when it becomes more widely available to see what they have to say.
Regards, Richard
Richard, thanks for the answer !!! Your experience in conducting CPET is invaluable. I expect from you another cognitive and fascinating article about CPET.
Hello, Richard. I plan to spend CPET to a patient with severe respiratory limitations. I want to choose the right protocol for the load. Can you give a link to the literature on this topic? In your work you use ramp protocols 5, 8, 9 watts / minute? Is your laboratory involved in the selection of CPET-based rehabilitation programs?
Andrey –
The lowest ergometer ramp setting we use in my lab is 10 watts/minute. When a patient is so debilitated that we are contemplating a lower workload (5 watts/min?) then it’s just as likely that they will end the test due to it’s length and not to the workload. I won’t turn any patients away just because they are debilitated but to me the point of a CPET is to be diagnostic, i.e. determine what the cause of an individual’s exercise limitation, and if their ability to exercise is that limited then the CPET isn’t likely to tell you anything you don’t already know.
We do CPETs for some patients that are starting pulmonary rehab but this is primarily so the physical therapists know what’s safe for the patient and secondarily, what their primary exercise limitations (ventilatory limit, desaturation, blood pressure etc.) so they know what to work on.
Regards, Richard
Our program is also limited to the protocol for 10 watts/minute. But it allows you to create any protocol yourself. There is research. “Benzo R. P. et al. Optimal protocol selection for cardiopulmonary exercise testing in severe COPD //Chest. – 2007. – Т. 132. – №. 5. – С. 1500-1505.” It is limited to the number of patients with protocols. But it is limited by the number of patients. P.S.: The protocol was used 10 watts/minute testing lasted 8 minutes.
Hello Richard. Did you use treadmill in your work? How to choose the right speed and angle? could you share your experience?
Andrey –
We’ve used a bicycle ergometer for the last 15 years. Before that we had a treadmill and used a modified Bruce protocol not because we thought there was some particular advantage with it but because that was what the doctors were familiar with. I didn’t disagree because it also meant that most tests were more than 5 but less then 10 minutes in length. I think exercise tests longer than 10 minutes run into a fatigue factor simply from the length of the test and not necessarily because you’ve reached their true VO2 limit. You have to remember that we’re not a sports medicine clinic but are dealing with primarily debilitated or sedentary patients.
I think it’s easier to get a better quality ECG and blood pressures on a bicycle ergometer and maybe a higher VO2 with a bit less overall safety on a treadmill.
Regards, Richard
It is better to use an individually selected protocol. The treadmill is not as safe as a bicycle ergometer, but by adjusting the speed and angle, I think that you can get a good result.
Andrey –
I’ve had difficulty with trying to select treadmill protocols for specific patients. I’ve often found patients able to perform significantly better or worse than expected. That’s one reason I found the Bruce and Modified Bruce protocols useful since they managed to get to a high workload rather quickly and yet still had decent low workload levels. I’m not sure adjusting results on the fly is a good idea as it’s easy to overshoot and undershoot the changes.
Regards, Richard