I was recently contacted by the manager of a lab that was having problems with their N2 washout lung volumes. Specifically, their N2 washout lung volumes (FRC in particular) were coming out low and everyone being tested on the system looked like they had restriction. The system has been checked by the manufacturer’s service techs several times and they’d replaced the tubing, the O2 tank and a number of parts. Service first asked them to wait between tests and then not to bother. Most lately they’ve been asked to calibrate the system before each test. Despite all this, their system continues to under-estimate lung volumes.
We’ve all had seemingly intractable problems with our test systems at one time or another. Sometimes they’re problems that can only be fixed by replacing major components, such as a gas analyzer or a motherboard. Sometimes they turn out to be something simple that nobody noticed despite looking straight at it numerous times. Experience and good technical support helps, but for every test system there has to be at least a couple of problems that are either uncommon, difficult to diagnose or are happening for the first time. When this happens it’s best to go back to basics and try to see what it is that’s most likely to explain the symptoms.
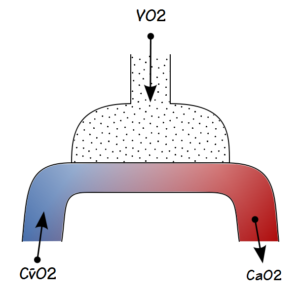
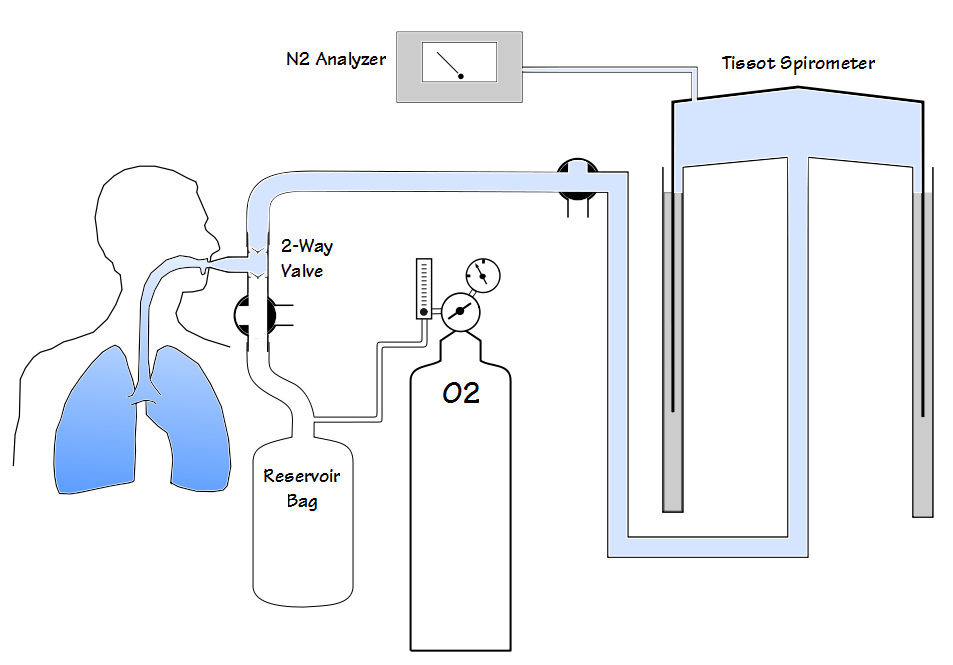
N2 washout lung volume measurements measure the amount of nitrogen residing in the lung and use this to estimate the volume of the entire lung. Closed circuit lung volume measurements using nitrogen were first attempted in 1932 by Christie. Christie’s approach used a known volume of oxygen to dilute the nitrogen in the lung but accuracy was limited at least in part because the amount of oxygen in the closed circuit was constantly changing due to the subject’s oxygen uptake. In 1940 Darling et al demonstrated an open circuit technique that is the basis for current N2 washout tests. In this approach the nitrogen in a subject’s lung was washed out with 100% O2 and their exhaled air was collected in a Tissot spirometer. After a certain amount of time (nominally 7 minutes) the exhaled volume and the N2 concentration in the Tissot spirometer was measured. The amount of nitrogen that had been exhaled is then calculated using simple math and the subject’s FRC is estimated from that.
Continue reading →