I’ve had a number of reports across my desk in the last couple of weeks with both elevated and reduced FRC’s that were associated with a more-or-less normal TLC. I reviewed the raw data from all of these tests (I review the raw data from all lung volume tests) and in only a few instances did I make any corrections to the report. This made me think however, about what, if anything, is an abnormal FRC trying to tell us?
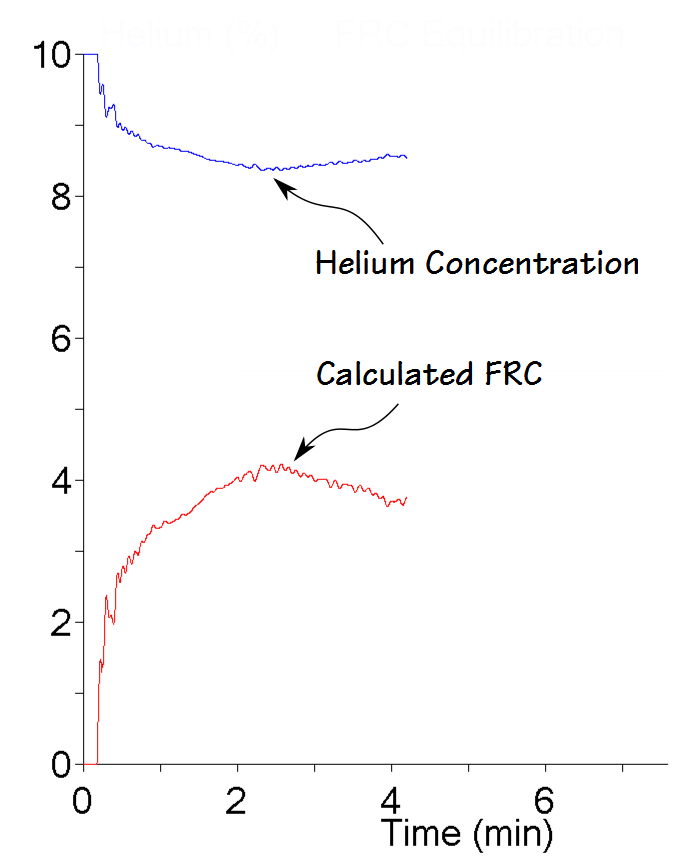
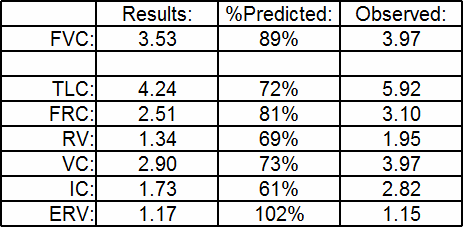
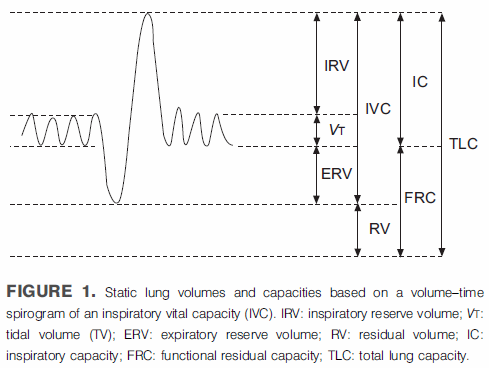
The answers to that question range from “a whole bunch” to “not much” to “darned if I know”. When you measure lung volumes TLC is really the only clinically important result. RV can be useful at times but although the other lung volume subdivisions may play a role in the measurement process they have only a limited diagnostic value. All lung volume measurements start with FRC, however, and if you don’t know you have an accurate FRC how do you know that TLC is accurate?
FRC is a balance point of opposing forces in the lung and thorax. Lung tissue wants to collapse, the rib cage wants to spring open and the diaphragm wants to do whatever muscle tone, gravity and the abdomen allows it to do. All of these forces are to one extent or another dynamic and can change over time. These changes can occur both slowly and rapidly, and are the primary reason why isolated changes in FRC don’t tend to have a lot of clinical significance. For all lung volume measurements however, one primary assumption is that FRC does not change during the test and this isn’t necessarily true.