Recently a report came across my desk from a patient being seen in the Tracheomalacia Clinic. The clinic is jointly operated by Cardio-Thoracic Surgery and Interventional Pulmonology and among other things they stent airways. The patient had been stented several months ago and this was a follow-up visit. Given this I expected to see an improvement in spirometry, which had happened (not a given, BTW, some people’s airways do not tolerate stenting), but what I didn’t expect to see was a significant improvement in lung volumes and DLCO.
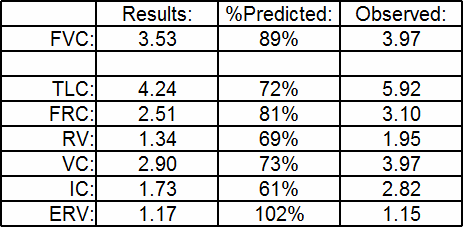
When I took a close look at the results however, it wasn’t clear to me that there really had been a change. Here’s the results from several months ago:
| Observed: | %Predicted: | Predicted: | |
| FVC: | 1.19 | 50% | 2.38 |
| FEV1: | 0.64 | 35% | 1.79 |
| FEV1/FVC: | 53 | 71% | 76 |
| TLC: | 3.21 | 76% | 4.22 |
| FRC: | 2.34 | 96% | 2.43 |
| RV: | 2.11 | 113% | 1.85 |
| RV/TLC: | 66 | 150% | 44 |
| SVC: | 1.15 | 48% | 2.37 |
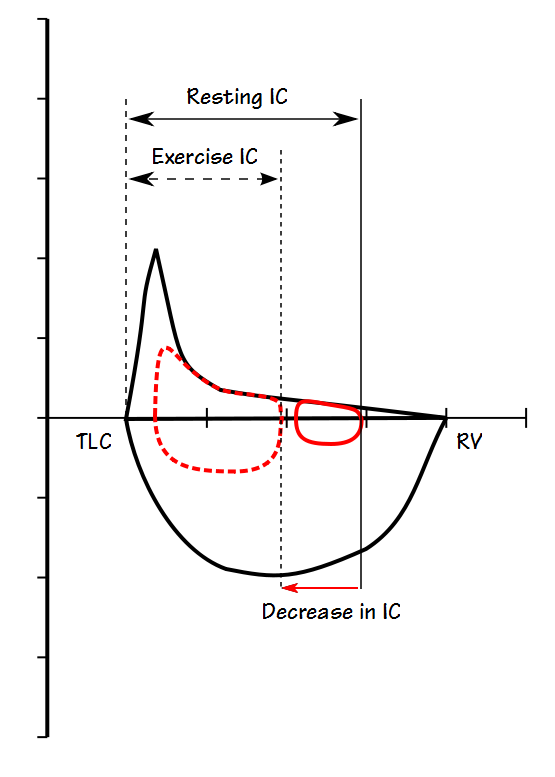
| IC: | 0.87 | 48% | 1.80 |
| ERV: | 0.25 | 41% | 0.58 |
| DLCO: | 6.59 | 38% | 16.18 |
| VA: | 1.78 | 43% | 4.12 |
| IVC: | 1.04 |
[more] Continue reading