The issue of PFT staff licensure or certification has recently been a topic of discussion on the LinkedIn Pulmonary Function Studies group and the Diagnostics section of the AARConnect discussion board. The overwhelming majority of those posting comments have been in favor of some form of licensure or certification. CPFT (Certified Pulmonary Function Technician) and RPFT (Registered Pulmonary Function Technician) certification is discussed most often but not surprisingly on the AARConnect board most posters feel that RRT (Registered Respiratory Therapist) certification should be required as well. Continue reading
Category Archives: Test quality
DLCO Dilemma
For the last several months I’ve noticed what appears to be a greater than normal number of patient test results where the VA volume from the DLCO test was greater than the TLC. This is not impossible of course, but it usually tends to be more on the rare side and when I’ve seen this in the past and inspected the results closely there were usually either problems with the lung volume test or the difference was only a few percent and within the error bar for both tests. We’ve been seeing VA’s that were larger than TLC more frequently lately but when I look at the results closely most of the time I have been unable to see anything wrong with either the lung volume or the DLCO test. At the same time, we have a number of patients that are frequent fliers and have seen what looks to be bigger differences in DLCO from visit to visit than usual as well as a number of patients that have had larger DLCO results than we would have expected.
The problem is that these apparent problems are really just suspicions with very little real evidence. I’ve been paying very close attention to lung volumes since our hardware and software upgrade last summer so my paranoia level is on the high side and I may well be overreacting. Late last week however, I found myself on the horns of a dilemma. The test results for a patient with a helium dilution TLC that was 68% of predicted but at the same time with a VA that was 93% of predicted and a DLCO that was 129% of predicted came across my desk.
Equipment is not detecting glottal closure and cough
In my last blog on personal spirometers I mentioned that one of the university projects has developed software that assesses spirometry results for ATS-ERS standard including cough, glottal closure and early termination of exhalation. The specific project that claimed this also claimed to have attained a 70% detection rate using waveforms from the NHANESIII study. This should be taken as a challenge by the pulmonary function equipment manufacturers to improve their existing software.
The test systems I am familiar with are pretty much limited to being able to determine back-extrapolation and whether end-expiratory flow rates meet ATS-ERS end-of-test criteria. So far they have not attempted to assess spirometry efforts for the cough or glottal closure that are also part of the ATS-ERS criteria for test quality. Here is a good example of glottal closure:
DLCO, by the numbers
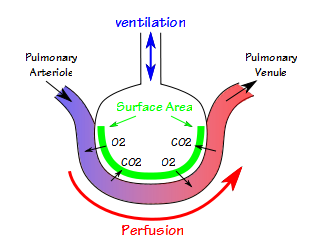
I was recently contacted by a physician looking for an illustration or diagram to help make gas exchange and DLCO more understandable. We’ve all seen the diagram of the alveoli with a capillary stretched around it and with oxygen and carbon dioxide exchanging across the membrane. I think I first saw it in Comroe’s ‘The Lung” published in the 1960’s, but it may well be older than that. It’s hard to improve on this and dozens of versions have been made of it.
He said something that got me thinking “for instance in a preoperative setting … all we know is a number on a seedy print out and all we use is a DLco % to tell us what to do!”. When I review reports I can access all of the raw data from all of a patient’s efforts so there’s a lot I can see about test quality that doesn’t show up on the final report. So what is a reduced DLCO test trying to tell you when all you have are numbers to look at?
VA versus TLC, what this can tell you about test quality
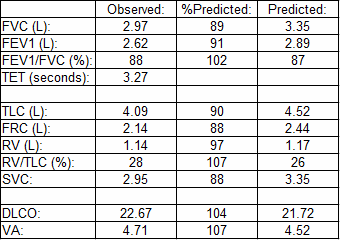
I’ve had a bug lately about lung volumes and I guess that today is no different. A report with some odd lung volume results came across my desk and I’ve spent some time trying to figure out what the numbers are telling me about test quality.
What concerned me was the 15% discrepancy between the VA from the DLCO and the TLC measured by plethysmography. VA is measured from the insoluble component of the DLCO gas mixture (methane in this case) and is almost always less than TLC. VA is a single-breath measurement and for VA and TLC to be close this usually means the patient must have very good gas mixing inside their lungs. Even when the quality of the DLCO and lung volume tests are good however, VA is almost always less than TLC. So why was VA so much larger than TLC in this case?
N2 washout drift throws another curve.
Just when we thought it was safe to go back in the water, we’ve run into another N2 washout-related problem. Although it probably affects the TLC and RV calculations in a minor way, it was actually noticed in relation to spirometry.
When spirometry is reviewed in my lab the FVC is compared to the SVC, if one has been performed. If the SVC is greater than FVC, then the FEV1/VC ratio is recalculated using the SVC. This is in line with the ATS recommendations on interpreting spirometry and does occasionally throw up a patient with airway obstruction that otherwise would not have been detected.
I have been reviewing the raw data from all of the lung volume tests lately. My lab has a mix of equipment and performs lung volumes with helium dilution, nitrogen washout and by plethysmograph. I’ve mentioned previously that we went through a major upgrade in equipment and software over the summer and this extra scrutiny on lung volumes is in part because of the problems we’ve had with the nitrogen washout test.
Busted for speeding during an N2 washout
Nitrogen washout lung volumes are still relatively new to my PFT Lab. The number of problems we’ve encountered has decreased substantially but we are still learning some of the idiosyncrasies of the system. Recently while trying to understand a test with odd results we were reminded by the manufacturer that during the washout period a patient’s inspiratory and expiratory flow rates should not exceed 1.5 liters/second. The reason this “speed limit” is necessary highlights some of the limitations of modern open-circuit lung volume measurements.
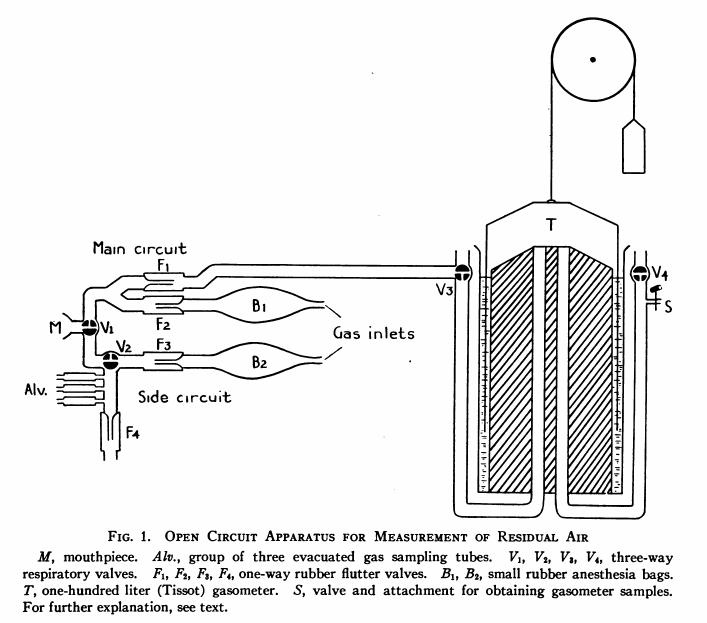
The basic concept behind nitrogen washout is relatively simple. The air we breathe contains 78% nitrogen which is a relatively inert, insoluble gas. If you have a patient breathe 100% oxygen and then collect their exhaled air you can calculate the volume of exhaled nitrogen by multiplying the concentration in the exhaled air by the total volume of air that was collected. Once you know the volume of nitrogen you can then calculate the lung volume.
Initially this was a laborious and cumbersome process. The patient’s exhaled breathing circuit and a Tissot Gasometer (a very large spirometer with a volume between 125 and 300 liters) are first flushed with oxygen several times to remove any nitrogen. Next, while breathing room air the patient exhales to RV and an end-expiratory gas sample is taken and used to estimate the patient’s alveolar nitrogen concentration. The patient is then switched to 100% oxygen and breathes for seven minutes. At the end of the washout period the nitrogen concentration of the exhaled gas in the gasometer is analyzed and the volume recorded.
Plethysmography and “trapped air” demystified
Recently I was reading the blog of someone who teaches Pulmonary Function testing and they stated:
“…in emphysema and air trapping, the VTG (thoracic gas volume) will be higher than a FRC (functional residual capacity) measured by Helium dilution and Nitrogen washout. This is because VTG is the volume of gas contained in the thorax, whether in communication with the airways or trapped in the thorax.”
This unfortunately is not correct, but it is a common misconception and since there was a time when I believed it myself I find it difficult to fault the author too much. I think it’s time to return to the basics of plethysmographic lung volumes however, and show why this is not true.
N2 washout switch-in error
I have been taking a close look at the raw data from all lung volume tests lately in large part because N2 washouts are still relatively new to my PFT Lab and we’re continuing to learn from our mistakes. When I saw this N2 washout test I knew that there was something wrong with it. The patient had performed three N2 washout tests and the TLC, FRC and RV for this one test were significantly larger than for the other tests. The most common problem we’ve been having with N2 washouts has been with patient leaks during the washout period which almost always show up as an upwards drift in the tidal baseline. This test did not show any drift however, and it took me a little while before I could see what was wrong with it.
The N2 washout maneuver has the patient start by breathing tidally for a short period of time in order to determine where end-exhalation (FRC) is located. The patient then performs a slow vital capacity maneuver by steadily inhaling maximally to TLC and then exhaling maximally to RV. The technician then switches the patient into the washout breathing circuit at maximal exhalation and the patient resumes breathing tidally for the remainder of the test.
Poor quality test results. When do you accept them?
The ATS/ERS have published standards for most Pulmonary Function tests. These standards include the criteria that are used for assessing test quality. What these standards don’t address however, is how poor a test’s quality can be yet still be acceptable for reporting.
We’ve all had patients that aren’t able to perform tests correctly. There can be many reasons why this happens. Lack of comprehension due to cultural or language barriers. Dementia. Extreme shortness of breath. Fatigue. Neuromuscular disease. Whatever the reason, you’ve done the tests with a patient and gotten the best you think you can get, how bad do they have to be before you don’t report them? Continue reading