Just when we thought it was safe to go back in the water, we’ve run into another N2 washout-related problem. Although it probably affects the TLC and RV calculations in a minor way, it was actually noticed in relation to spirometry.
When spirometry is reviewed in my lab the FVC is compared to the SVC, if one has been performed. If the SVC is greater than FVC, then the FEV1/VC ratio is recalculated using the SVC. This is in line with the ATS recommendations on interpreting spirometry and does occasionally throw up a patient with airway obstruction that otherwise would not have been detected.
I have been reviewing the raw data from all of the lung volume tests lately. My lab has a mix of equipment and performs lung volumes with helium dilution, nitrogen washout and by plethysmograph. I’ve mentioned previously that we went through a major upgrade in equipment and software over the summer and this extra scrutiny on lung volumes is in part because of the problems we’ve had with the nitrogen washout test.
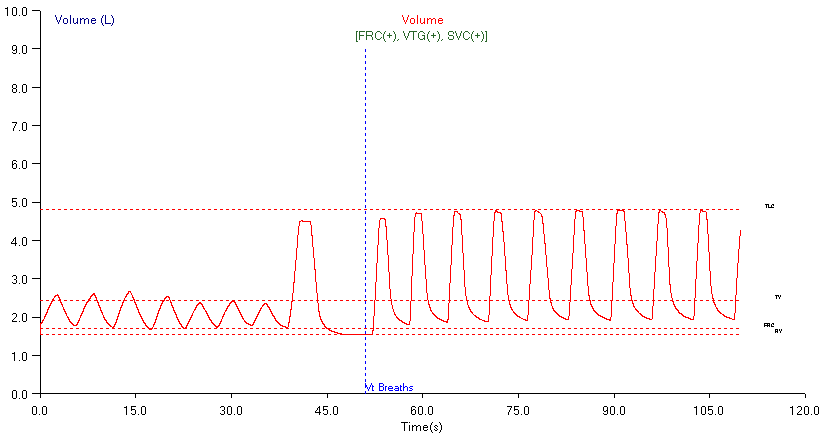
Today a report came across my desk that at first glance met the criteria for recalculating the FEV1/VC ratio with the SVC. The spirometry was within normal limits, but the FEV1/FVC ratio was towards the lower end of the normal range and there was some mild coving on the flow-volume loop. The SVC was about 0.30 L greater and when the FVC was replaced with the SVC, it was definitely below the normal range. One of the patient’s diagnoses was asthma so the overall report was consistent with mild airway obstruction and there were no warning bells going off. But since the lung volumes were performed by N2 washout I went ahead a looked at the raw data.
Once again the first thing I saw was drift during the washout period. This has been a chronic problem with the N2 washout test that I attribute to patient leaks. I think the leaks are a result of two factors. First, the equipment that performs the N2 washout will only allow us to use what I consider to be a small mouthpiece. I have always been an advocate of using the largest possible mouthpiece a patient can tolerate because it cuts down on leaks and at the moment we don’t have that option. Second, the instructions for the test states that the patient should “take slow deep breaths” during the washout period but what I see often looks more like fast deep breaths. I think that the technicians may be encouraging the patients to breathe faster and deeper than is optimal during washout and that anybody is more likely to leak when breathing this way.
The amount of drift was actually relatively small and although the TLC and RV were probably overestimated, the actual error is probably small and I would be hard pressed to believe it would alter the interpretation of the lung volumes being normal. However, when I eyeballed the drift it was apparent that the SVC was being overestimated by about 0.30 L and that instead of being larger than the FVC, the SVC was actually the same as the FVC. The final read on the report was that the spirometry was within normal limits.
So, in this case drift during the N2 washout didn’t significantly affect TLC and RV, but would have significantly affected the way spirometry had been interpreted. Go figure. I guess I’ll be continuing to review all the raw lung volume test data (no matter what the technique) for the forseeable future.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.