Nitrogen washout lung volumes are still relatively new to my PFT Lab. The number of problems we’ve encountered has decreased substantially but we are still learning some of the idiosyncrasies of the system. Recently while trying to understand a test with odd results we were reminded by the manufacturer that during the washout period a patient’s inspiratory and expiratory flow rates should not exceed 1.5 liters/second. The reason this “speed limit” is necessary highlights some of the limitations of modern open-circuit lung volume measurements.
The basic concept behind nitrogen washout is relatively simple. The air we breathe contains 78% nitrogen which is a relatively inert, insoluble gas. If you have a patient breathe 100% oxygen and then collect their exhaled air you can calculate the volume of exhaled nitrogen by multiplying the concentration in the exhaled air by the total volume of air that was collected. Once you know the volume of nitrogen you can then calculate the lung volume.
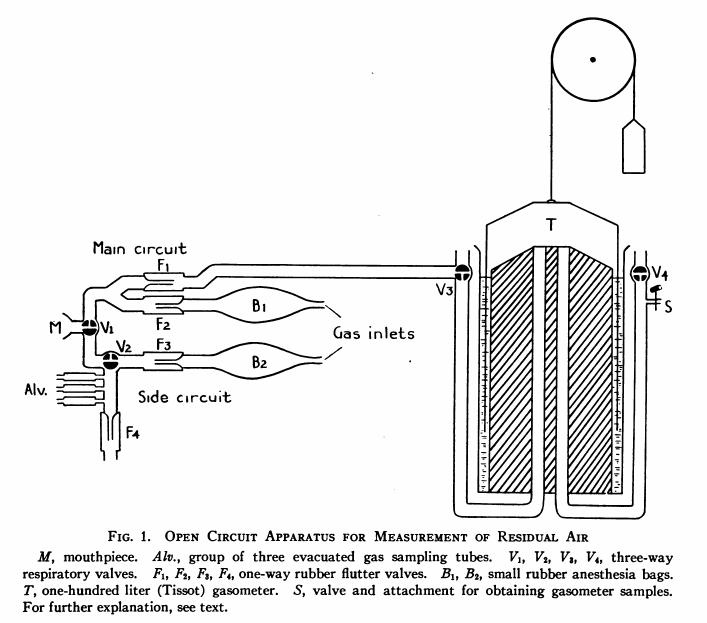
Initially this was a laborious and cumbersome process. The patient’s exhaled breathing circuit and a Tissot Gasometer (a very large spirometer with a volume between 125 and 300 liters) are first flushed with oxygen several times to remove any nitrogen. Next, while breathing room air the patient exhales to RV and an end-expiratory gas sample is taken and used to estimate the patient’s alveolar nitrogen concentration. The patient is then switched to 100% oxygen and breathes for seven minutes. At the end of the washout period the nitrogen concentration of the exhaled gas in the gasometer is analyzed and the volume recorded.
At some point it was realized that instead of being physically collected exhaled air could be measured with a flow sensor and a high-speed nitrogen analyzer and the exhaled nitrogen volume calculated from the integrated wave forms. Later it was also realized that what wasn’t nitrogen in the exhaled air was mostly oxygen and that the nitrogen concentration could be estimated from the oxygen concentration instead. Thus the modern open-circuit nitrogen washout lung volume technique was born.
The reason there is a limitation in a patient’s inspiratory and expiratory flow rates during the washout period has mostly to do with the speed of the oxygen analyzer and the sampling system. All gas analyzers have a limited ability to accurately react to rapid changes in gas concentrations which is due both to design issues in the electronic circuitry and to the physical sample volume needed by an analyzer. The current recommendations are for a 95% response to 10% change in nitrogen (or oxygen) in less than 60 milliseconds, which sounds quite fast but the transition from inspiration to expiration, particularly early in the washout period, can show much larger changes in nitrogen concentrations on a small time scale so this specification is only just adequate.
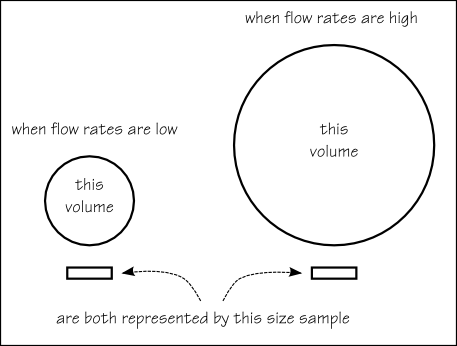
More importantly, gas samples are usually transported to the analyzer from the breathing manifold by narrow tubing. Because gas is drawn through the tubing by a pump at a constant rate this means that there is a smaller amount of gas sample per unit of inhaled or exhaled air when flow rates are high than when flow rates are low. This means that when inspiratory or expiratory flow rates are high a change in gas concentration may not be “seen” by the analyzer because the sample is too small. In addition the tubing that transports the gas sample from the breathing circuit to the oxygen analyzer also causes rapid changes in gas concentrations to be “smeared” (due to flow shear effects near the wall of the tubing) and this “smearing” will be proportionally greater when inspiratory or expiratory flow rates are high.
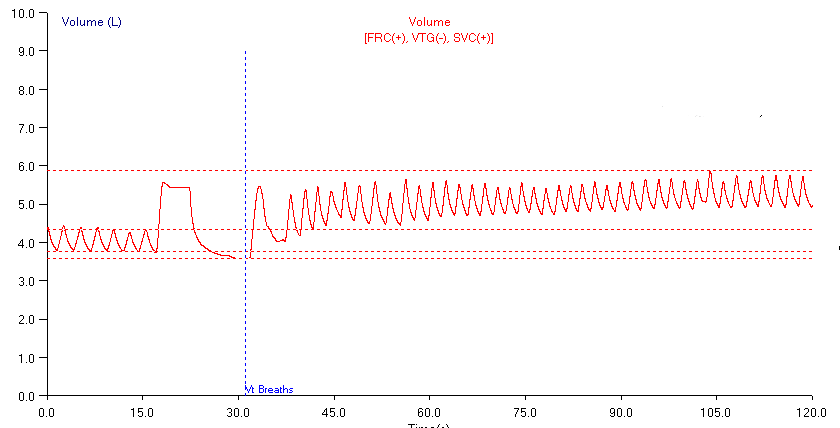
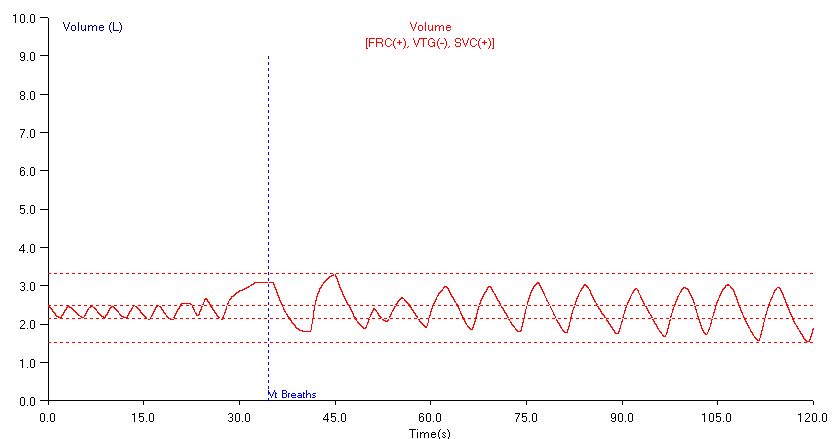
The inspiratory and expiratory flow signals have to be integrated to convert flow to volume. High flow rates aren’t as much a concerning factor for this but it is a much more difficult task than is generally appreciated given that the gas concentrations, humidity and temperature of inspiratory and expiratory air are so different. The various equipment manufacturers appear to have solved this problem quite well with various proprietary software algorithms and flow-sensor construction techniques but the long term stability of the integrated volume is always a concern. Strictly speaking because of differences in oxygen consumption, CO2 production and humidity there are always small differences in the amount of air that is inhaled versus the amount that is exhaled and this means that the stability of FRC shown during prolonged tidal breathing is to some extent an artificial construction.
Although some drift during the washout period is probably normal, too much drift can effect the measured TLC and not just because it probably indicates a leak. Most nitrogen washout systems have the patient perform a SVC maneuver and exhale to RV before being switched to washout mode. This actually solves several problems simultaneously. First it allows the end-exhalation air to be sampled and the starting alveolar nitrogen concentration estimated. Second, by exhaling to RV the amount of nitrogen that has to be washed out and therefore the time needed to wash it out is significantly reduced. Finally, since it is RV (or the lung volume at which the patient is switched to washout mode) that is measured, the SVC maneuver allows FRC and TLC to be calculated.
So when drift during the washout period is detected is it normal or is it due to a leak? When drift is large and exceeds the SVC envelope it will cause the calculated TLC and/or RV to be miscalculated and it’s obvious the test can be rejected. When drift is small however, it is a lot less clear whether it signals a leak or not. About the only way we can be sure one way or the other is to always perform a minimum of two lung volumes tests and to compare results.
These problems with inspiratory and expiratory flow rates, analyzer speed and integrator drift would not have been as issue with early nitrogen washout systems but the modern systems are much faster, simpler and certainly much less cumbersome, so it is a good tradeoff.
Overall, I’d have to say that we’re satisfied with our new test systems. When good quality tests are compared we see little or no difference between lung volumes performed by helium dilution and those performed by nitrogen washout. There has been a learning curve and the problems for each technique are different and it has been learning these differences that made the first couple of months somewhat rocky.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS TASK FORCE: STANDARDISATION OF LUNG FUNCTION TESTING. Standardisation of the measurement of lung volumes. Eur Respir J 2005; 26: 511-522.
Darling RC, Cournand A, Richards DW. Studies on the intrapulmonary mixture of gases. III. An open-circuit method for measuring residual air. J Clin Invest 1940; 19: 609-618.
Newth CJL, Enright P, Johnson RL. Multiple-breath nitrogen washout techniques: including measurements with patients on ventilators. Eur Resp J 1997; 10: 2174-2185.
Tierney DF, Nadel JA. Concurrent measurements of Functional Residual Capacity by three methods. J. Appl. Physiol. 1962; 17: 871-873

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

Initial exhaled N2 concentration depends to some degree on the size of the breath taken. There is lack of clarity as to what the threshold should be for validity. If initial exhaled N2 concentration is less than 50%, would we consider this valid? What should a threshold be?
Thanks
William –
The “initial” exhaled N2 reading should be taken before the patient is switched to 100% O2 and should not be the first exhalation after that happens. The N2 washout test as it is currently performed has a number of flaws which include a standardized ending at 2% N2; the fact that it is O2 being measured and not N2; and the variable contribution of N2 body stores to exhaled N2.
– Richard