Recently I have been reviewing a lot of early pulmonary function research. I’m not feeling nostalgic but I think that re-visiting some of the older methods and technology may be interesting. Almost all Pulmonary Function laboratories presently use the single-breath technique to measure diffusing capacity. There are a number of reasons why this is case but I suspect that many technicians and physicians aren’t aware that there are several alternative methods for measuring diffusing capacity and that there was a time when at least one of these, the steady-state DLCO, was routinely used in clinical labs.Diffusing capacity, regardless of technique, is determined by the rate of CO uptake, divided by the driving (alveolar) pressure:
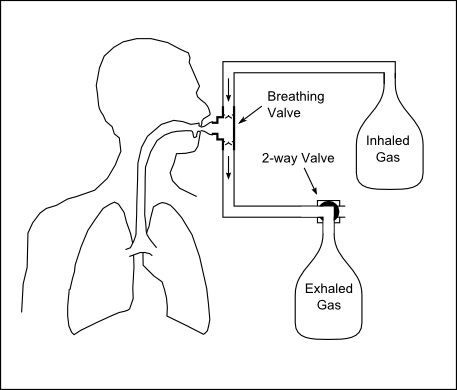
A steady-state DLCO test takes this simple equation and tries to run with it. It is relatively easy to measure CO uptake and a steady-state test system can be as simple as a breathing valve and large sample bags containing the inspiratory and expiratory gas mixtures.
The problem, and perhaps the most significant weakness of all steady-state DLCO measurements is the need to estimate the alveolar concentration of carbon monoxide. For each method of estimating alveolar CO there are limitations to either the accuracy of the measurement or the circumstances under which it can be performed. As importantly, the differences in the way each technique estimates PACO can lead to significant differences in calculated DLCO.
Depending on how carefully you count them there have been at least eight different approaches taken at one time or another towards estimating PACO, but two were used most frequently;
Filley et al, measured Vd/Vt by taking an arterial blood gas during the DLCO test and measuring the mixed expired CO2. Once Vd/Vt ratio was known it was possible to estimate PACO from:
The Filley approach was used (and modified) by many researchers and for some it is considered the “gold standard” of steady-state DLCO. The primary drawback for this technique is that small errors in the analysis of PaCO2 can have a large effect on the calculated Vd/Vt. In the range of normal values for PaCO2 and PECO2 a 1 mm Hg error in PaCO2 alone can cause an error of 8% in Vd/Vt. It’s also been suggested that the dead space/tidal volume ratio for CO2 does not necessarily match that for CO and that this could cause an error of up to 33% in calculated DLCO.
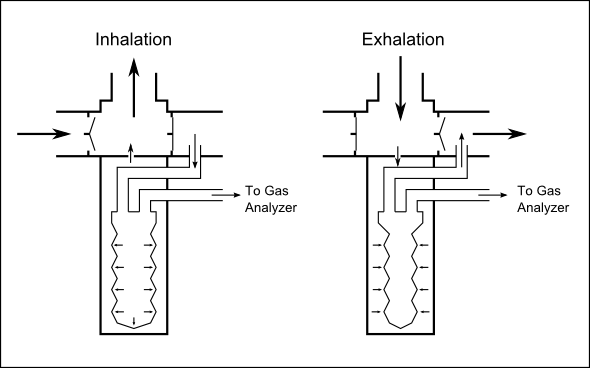
The other major approach, first published by Bates et al, was to assume that end-tidal CO was the same thing as PACO. A variety of end-tidal samplers were developed, most notably the ingeniously simple Rahn-Otis end-tidal sampling valve which was used in at least one clinical testing system (Collins Modular Lung Analyzer).
[This sampling valve uses the pressures generated during breathing to obtain end-tidal gas samples. During inhalation, the negative pressure in the breathing valve causes a small, thin-walled sample ballon to inflate with gas that is immediately downstream of a one-way valve on the exhalation limb of a breathing circuit. During exhalation, positive pressure causes the sample ballon to slightly deflate, preventing any exhaled gas from the beginning of the exhalation from entering. A sample pump set to a low flow rate continuously evacuates the balloon and sends the sample to the CO gas analyzer.]
Although this approach gets around the need for measuring or estimating Vd/Vt the primary limitation is that end-tidal gas concentrations are not necessarily an accurate reflection of alveolar gas concentrations and this is particularly so during exercise or hyperventilation. It is open to question just how “alveolar” the samples really are because end-tidal sampler valves act to average out the gas sample and the amount of gas averaged and which part of the exhalation it comes from will depend on tubing size, sampling rate, respiratory rate, tidal volume and is generally not predictable.
The steady-state DLCO techniques are a reflection of the available technology of the time they were developed. They played a significant role in the early understanding of ventilation and perfusion during exercise, membrane diffusing capacity and the diffusing capacity in lung disease. Technology and the understanding of diffusing capacity has moved onwards in the last half-century and the single-breath DLCO technique has become the primary clinical measurement technique. Steady-state DLCO measurement systems have not been commercially available for at least several decades and there are a number of reasons for this.
A steady-State test is significantly longer and more time-consuming than a Single-Breath test. Steady-state tests are at least three minutes long (not including set-up time) because it is necessary for the DLCOSS gas mixture to be breathed long enough for a true steady-state condition to exist.
Steady-state diffusing capacity measurement techniques suffer from a lack of standardization because there is no consensus on the best way to determine alveolar CO. CO, like O2 and CO2 varies constantly in the alveoli during the breathing cycle and the selection of a specific alveolar CO concentration to represent an average value depends on the assumptions being used to select it.
Steady-state DLCO measurements are highly influenced by minute ventilation and results can be markedly skewed by hyperventilation. When tidal volume is low the error bar is greater for either due to dead space gas contamination of end-tidal samplers or because minor errors in calculating Vd/Vt are magnified. When tidal volumes are large there is an increase in the surface area of the lung and the average absolute volume at which measurements are made becomes a factor.
Clinical interpretation of results can be difficult. Steady-state measurements are obtained near FRC. Because the lung has a lower surface area and possibly a thicker membrane at FRC this means these results are always lower than measurements obtained at TLC by single-breath measurements. Because tidal breathing does not uniformly ventilate the lung, measurements made at FRC can not be linearly or otherwise systematically related to measurements made at TLC in patients with lung disease.
Finally, even though the concentration of carbon monoxide in the steady-state gas mixture is nominally one-third of that used in the single-breath DLCO mixture (usually 0.10% with a range of 0.04% to 0.15%), the greater length of a Steady-State test means that the amount of carbon monoxide absorbed by the patient tends to be much higher than it does for a Single-Breath test. COHB has been estimated to increase as much as 2.4 percent during the course of a single test. This raises the issue of patient safety given the COHb burden placed on a patient from even a single steady-state test, let alone from repeat testing. Although noted in the literature, this fact was not widely appreciated and I personally shudder to think of the number of times during the 1970’s that I performed three steady-state DLCO tests on frail and sick patients because that was my medical director’s standard protocol.
I’d have to say the era of steady-state DLCO testing has passed and will not come again. It has been several decades since steady-state DLCO tests were performed clinically, and it’s been a least a decade since I last saw a research paper involving steady-state DLCO. Although theoretically still capable of playing a role in research, there are other DLCO techniques that are easier to perform, easier to interpret and less prone to error. Probably the only value that steady-state DLCO still has is in teaching the concepts and history of DLCO testing.
References:
Anderson TW, Shephard RJ. A theoretical study of some errors in the measurement of pulmonary diffusing capacity. Respiration 1969; 26:102-115
Apthorp GH, Marshall R. Pulmonary diffusing capacity: a comparison of breath-holding and steady-state methods of using carbon monoxide. J Clin Invest 1961; 40:1775-1784
Bates DV, Boucot NG, Dormer AE. The pulmonary diffusing capacity in normal subjects. J Physiol 1955; 129:237-252
Bates DV, Pearce JF. The pulmonary diffusing capacity: a comparison of the methods of measurement and a study of the effect of body position. J Physiol 1956: 132:33-238
Bates DV, Knott JMS, Christie RV. Respiratory function in emphysema in relation to progress. Quart J Med 1956; 25:137
Bates DV. The measurement of the pulmonary diffusing capacity in the presence of lung disease. J Clin Invest 1958; 37:591-604
Bates DV, Varvis CJ, Donevan RE, Christie RV. Variations in the Pulmonary Capillary Blood Volume and Membrane Diffusion Component in Health and Disease. J Clin Invest 1960; 39:1401-1412
Beck KC, Hyatt RE, Staats BA, Enright PL, Rodarte JR. Carbon monoxide diffusing capacity of the lungs determined by single-breath and steady-state exercise methods. Mayo Clin Proc 1989; 64:51-59
Borland C, Mist B, Zammit M, Vuylsteke A. Steady-state measurement of NO and CO diffusing capacity on moderate exercise in men. J Appl Physiol 2001; 90:538-544
Bouhuys A, Georg J, Jonsson R, Lundin G, Lindell SE. The influence of histamine inhalation on the pulmonary diffusing capacity in man. J Physiol 1960; 152:176-181
Filley GF, MacIntosh DJ, Wright GW. Carbon monoxide uptake and pulmonary diffusing capacity in normal subjects at rest and during exercise. J Clin Invest 1954; 33:530-539
Forster RE, Cohn JE, Briscoe WA, Blakemore WS, Riley RL. A modification of the Krogh carbon monoxide breath-holding technique for estimating the diffusing capacity of the lung: A comparison with three other methods. J Clin Invest 1955; 34:1417-1426
Forster RE, Roughton FJW, Cander L, Briscoe WA, Kreuzer F. Apparent pulmonary diffusing capacity for CO at varying alveolar O2 tensions. J Appl Physiol 1957; 11:277-289
Kinker JR, Haffor AS, Stephan M, Clanton TL. Kinetics of CO uptake and diffusing capacity in transition from rest to steady-state exercise. J Appl Physiol 1992; 72:1764-1772
Leathart GL. Steady-state diffusing capacity determined by a simplified method. Thorax 1962; 17:302-307
MacNamera J, Prime FJ, Sinclair JD. An assessment of the steady-state carbon monoxide method of estimating pulmonary diffusing capacity. Thorax 1959; 14:166-175
McCredie RM. The diffusing characteristics and pressure-volume relationships of the pulmonary capillary bed in Mitral valve disease. J Clin Invest 1964; 43:2279-2289
Sybert A, Ayash R, Chatham M, Gurtner GH. CO concentration-dependent changes in pulmonary diffusing capacity in humans. J Appl Physiol 1982; 53:505-509
Turino GM, Brandfonbrener M, Fishman AP. The effect of changes in ventilation and pulmonary blood flow on the diffusing capacity of the lung. J Clin Invest 1959; 38:1186-120

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.