I was recently contacted by a physician looking for an illustration or diagram to help make gas exchange and DLCO more understandable. We’ve all seen the diagram of the alveoli with a capillary stretched around it and with oxygen and carbon dioxide exchanging across the membrane. I think I first saw it in Comroe’s ‘The Lung” published in the 1960’s, but it may well be older than that. It’s hard to improve on this and dozens of versions have been made of it.
He said something that got me thinking “for instance in a preoperative setting … all we know is a number on a seedy print out and all we use is a DLco % to tell us what to do!”. When I review reports I can access all of the raw data from all of a patient’s efforts so there’s a lot I can see about test quality that doesn’t show up on the final report. So what is a reduced DLCO test trying to tell you when all you have are numbers to look at?
The numbers can actually tell you quite a bit but before looking for a cause for a low DLCO you need to start by getting a sense of the test’s quality. To do this for DLCO the VA and theInspired Volume should also be reported.
Trying to determine DLCO test quality without other pulmonary function test results will be difficult because the results from spirometry and lung volume tests can be used both to assess DLCO quality and to guide the interpretation. Inspired Volume, for example, should be at least 90% of the FVC. When Inspiratory Volume is less than this the test gas mixture will probably not be as well distributed through the lung as it should be. When the Inspired Volume is markedly low compared to FVC then DLCO will likely be underestimated as much from a low VA as from poor gas distribution.
VA is a single-breath TLC measurement. Because it is a single-breath measurement it is almost always less than TLC measured by helium dilution, nitrogen washout or plethysmography. As long as VA is within 10% of the patient’s measured TLC then it is likely that the DLCO test gas was well distributed. If VA is significantly lower than TLC this is likely due either to a suboptimal inspired volume or to poor gas mixing from airway obstruction. There is a correlation between airway obstruction and the difference between VA and TLC so a low VA is to be expected if it is accompanied by significant airway obstruction and will be acceptable if it has an adequate Inspired Volume. If not you will need to assume that the DLCO is likely underestimated.
Correcting for hemoglobin is recommended but not required. The lack of hemoglobin correction only becomes an issue when the DLCO is slightly below the normal range because anemia may be the cause of the reduction, not a gas exchange defect.
If there is reason to believe a DLCO test is underestimated it is probably not possible to estimate by how much. Having said that unless a DLCO test is grossly suboptimal (and should have not been reported in the first place) it is unlikely that it is underestimated by more than about 25%. My experience is that DLCO is a fairly robust test and that patients can mis-perform it in many different ways and the results still come out reasonably correct. Like anemia, underestimation is an issue mostly when you are trying to determine if the results are within normal limits or not.
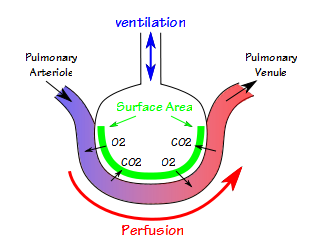
DLCO is essentially a measure of the lung’s functional surface area and will be reduced when lung perfusion, volume or ventilation are reduced. If all you have are the DLCO results then VA can tell you something about a patient’s lung volume and gas mixing, but only in a negative sense. If VA is within normal limits for the patient’s TLC then you can probably rule out significant restrictive and obstructive diseases, which then suggests that reduced perfusion is a primary cause. Unfortunately, VA (and DL/VA) can be reduced in both restrictive and obstructive disease, so this is where spirometry and lung volume measurements become important.
DLCO is often reduced in restrictive diseases. The degree to which it is reduced relative to the decrease in TLC can be used to differentiate between interstitial diseases and chest wall/neuromuscular diseases. This is the about the only place where DL/VA may be of some use (DL/VA is not DLCO normalized for lung volume, it is KCO!). The basic rule of thumb is that DL/VA will be normal or reduced in interstitial diseases and elevated in chest wall and neuromuscular diseases. To use DL/VA however, you need to know that VA is reduced because TLC is reduced and furthermore that VA is essentially the same as the measured TLC.
A reduced DLCO in the presence of significant airway obstruction will, of course, suggest COPD. A reduced DLCO without airway obstruction or restriction will, of course, suggest a perfusion limitation such pulmonary emboli or hepato-pulmonary syndrome.
DLCO can be used to assess a patient for lung resection, lobectomies and pneumonectomies. A simple approach is to estimate how much lung tissue will be removed as a fraction of the total lung volume and then estimate that DLCO will be reduced by the same amount. This is true to an extent, but a more accurate assessment will use a V/Q scan and take the perfusion and ventilation of the target lung volume into consideration as well. A post-pneumonectomy patient will have a reduced DLCO but DL/VA (okay, so there is another use for DL/VA) will be normal as long as the remaining lung is normal.
DLCO, VA and Inspired Volume can say a lot about lung function. DLCO is a critical component in the differential diagnosis of obstructive and restrictive lung diseases but to use it you first need to assess test quality with Inspired Volume and VA and only then can you use VA to help interpret the results.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.