When it comes to spirometry, it’s really all about FEV1. FVC and the FEV1/FVC ratio are also important of course, but because FVC is more likely to be underestimated than FEV1 they are less reliable.
Changes in FEV1 are critical in monitoring airway disease. The recent ATS guidelines on Occupational Spirometry indicate that a 15% decrease (adjusted for changes in age) is significant and cause for concern. For diagnosing airways disease however, it is important to know what a normal FEV1 is.
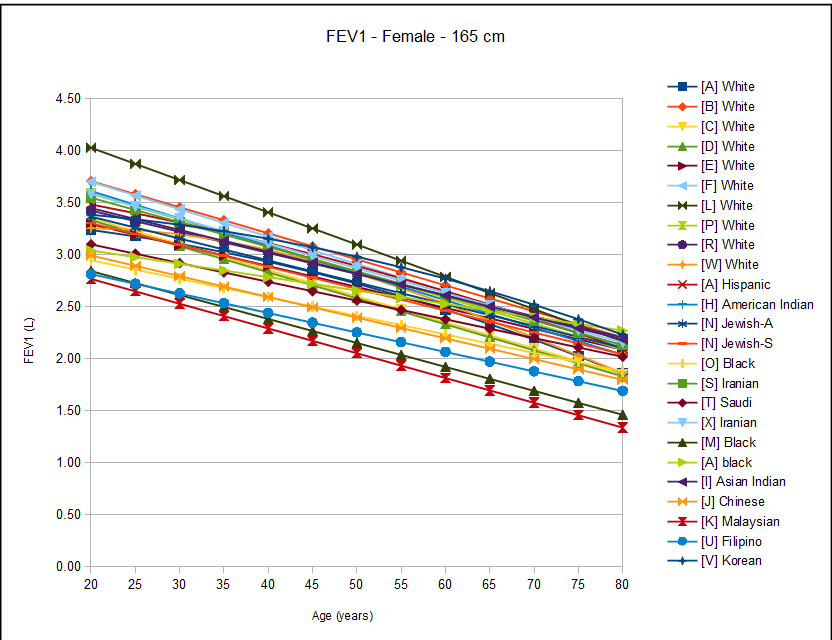
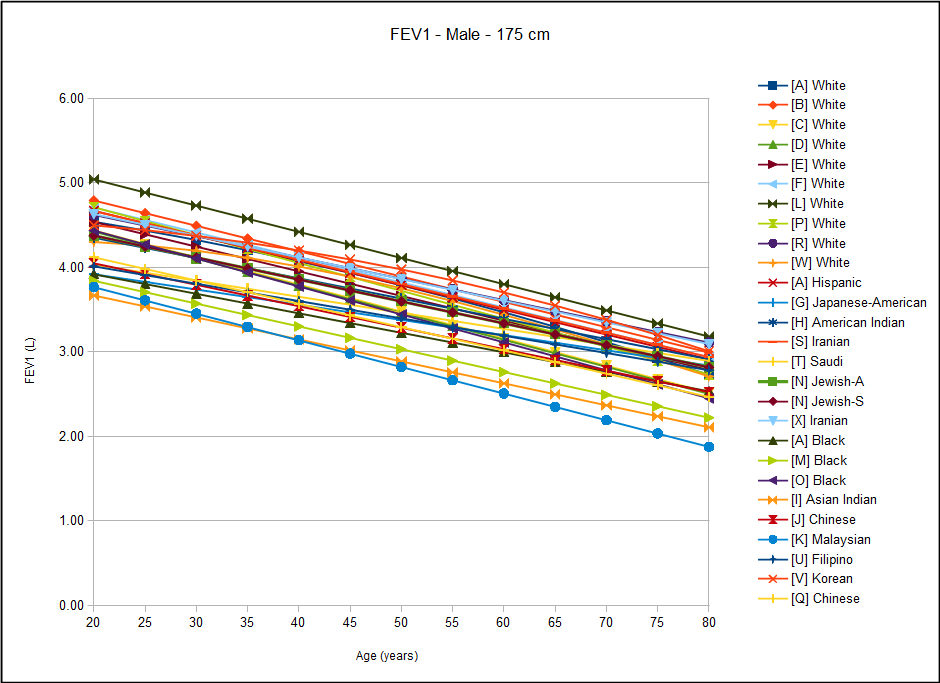
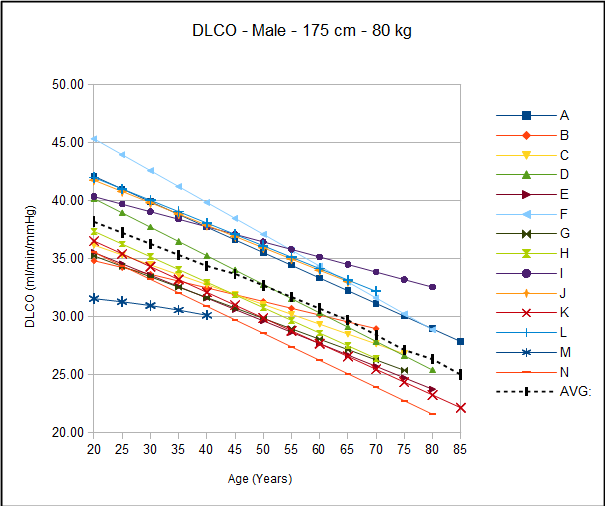
I have been able to find twenty-four different reference equations for FEV1. That’s good in one sense but that quantity also makes it that much more difficult to determine which reference equations should be used. When I graph results it often becomes more apparent what the equations are trying to tell us but in this case I came away a bit more confused instead.