A month or two ago in the AARC Diagnostics forum several members noted that their labs had acquired Impulse Oscillometry systems a number of years ago but that their physicians had since stopped ordering oscillometry tests, mostly because nobody understood what it was measuring and didn’t know how to interpret the results. There are a number of reasons why this is probably not an uncommon scenario and why, despite being first described in 1956, oscillometry is not used more widely.
But first, what is oscillometry, and what’s the best way to understand it?
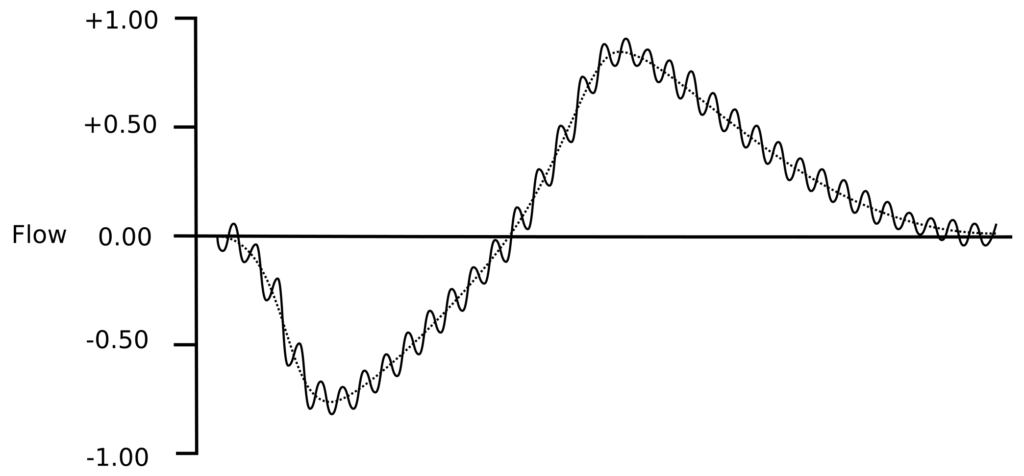
Oscillometry refers to a closely related group of techniques for measuring respiratory impedance by superimposing small pressure waves on top of normal tidal breathing.
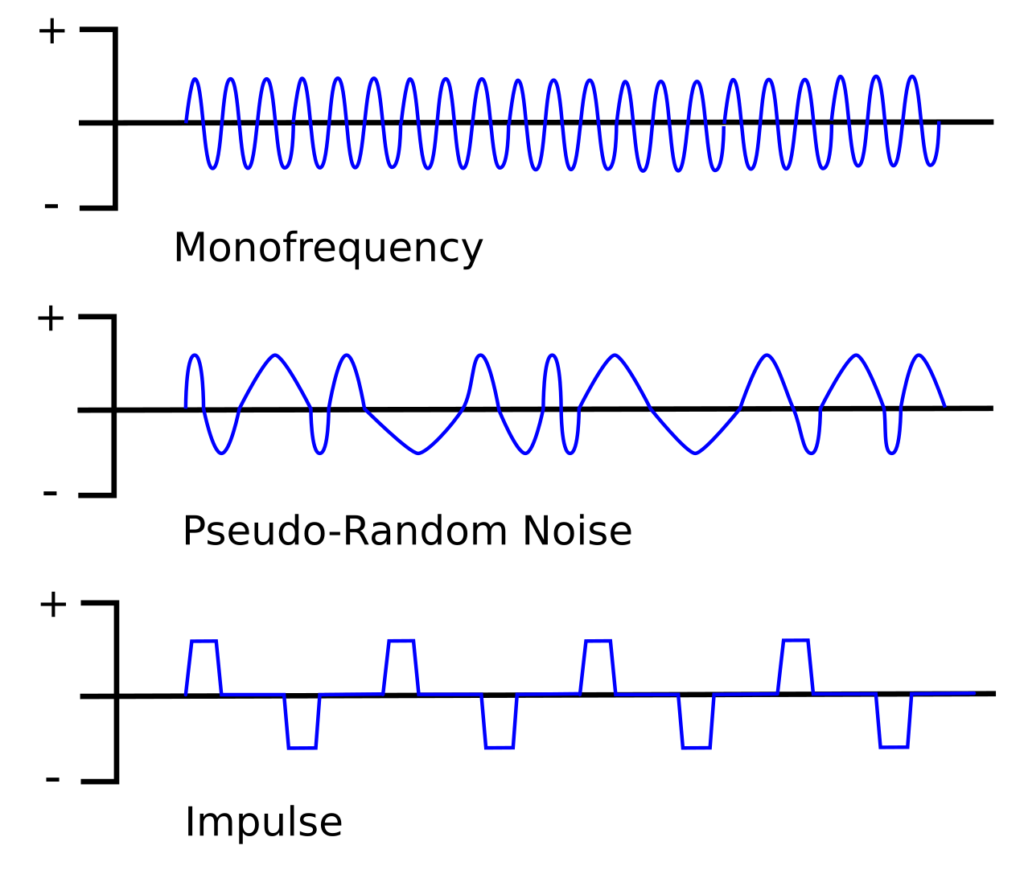
There are three main approaches: the Forced Oscillation Technique (FOT), which is sometimes used a blanket term for all oscillometry techniques but more often refers to a single frequency technique, Impulse Oscillometry (IOS) and Pseudo-Random Noise (PRN). Most commercial oscillometry systems use either PRN or IOS because each approach uses multiple oscillation frequencies more or less simultaneously which allows testing to performed relatively quickly. The mono-frequency technique is used mostly in research because although it is slow to scan all frequencies, it is able to resolve rapid changes occurring at a single frequency.
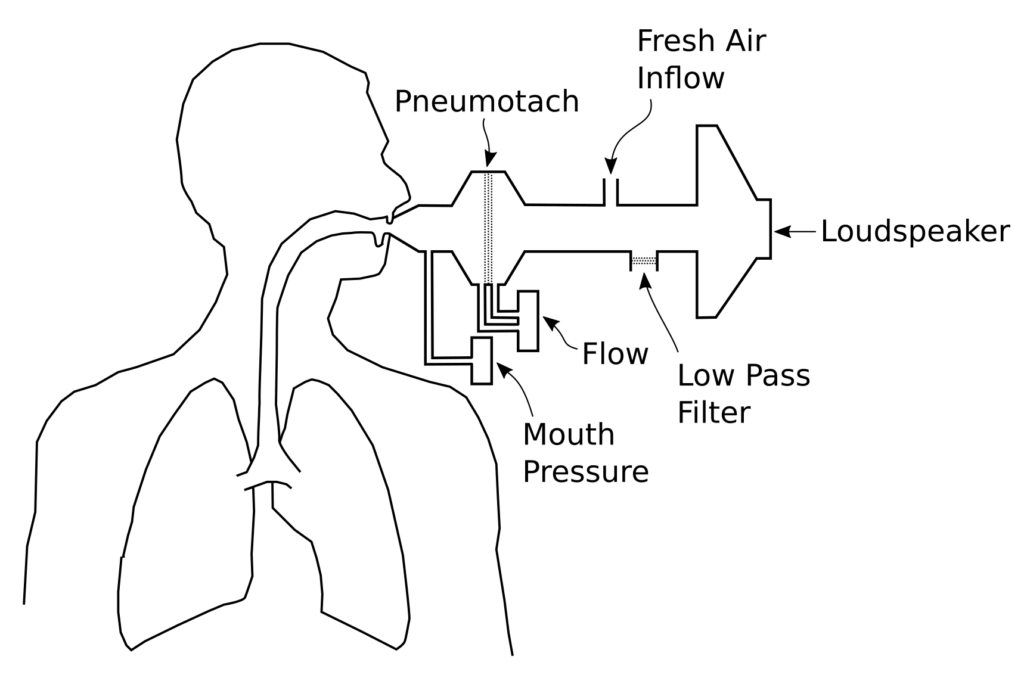
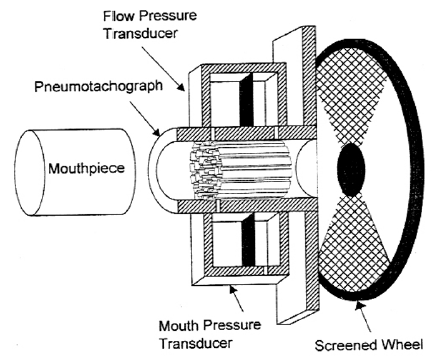
All techniques share a similar equipment configuration:
The oscillatory pressure is usually generated by a loudspeaker, although the actual waveform and the frequency it produces differ for each technique. The peak pressures are usually on the order of +/- 1 to 5 cm H2O (+/- 0.1 to 0.5 kPa). Because patients have to breathe during testing, the system provides a steady flow of fresh air in one manner or another but this has to include a low pass filter of some kind so that the pressure waveform is not significantly diverted or blunted. The key measurements are flow and the pressure at the mouth.
Continue reading