I’ve had some concerns for a while now about how the CO and CH4 concentrations are being calculated from the DLCO analyzer calibration zero offsets and gains on our test systems. For this reason I’ve been looking carefully at all of the raw data from our DLCO tests and today I came across an oddball test result. There are several reason why this is probably not the best example for this particular problem that I could come up with but it illustrates an important point and it’s in front of me so I’ll go with it.
In order to use the output from a gas analyzer you need to know the zero offset and the gain of the signal. Presumably the analyzer remains stable enough between the time it was calibrated and the time it is used for the zero offset and gain to be meaningful. When looking at the calibration data I’ve noticed that some of our test systems show relatively large changes in zero offset from day to day. These changes are still within the operating limits of the analyzer so no red flags have gone up over this. The test systems and analyzers are turned off over night so in order to see if the analyzers go through these kind of changes during a normal day I once did a series of calibrations each separated by five or ten minutes on one of the more suspect testing systems. What I saw was that although there were small changes from calibration to calibration, I didn’t see anywhere near the changes I’ve seen from day to day which at least implied that the analyzer remained reasonably stable during a given day.
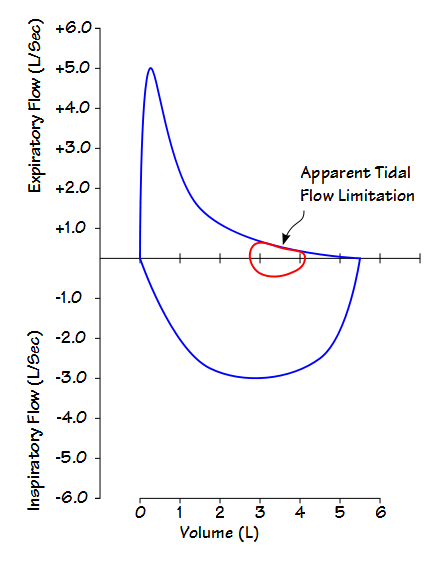
Today a patient’s report came across my desk and as usual I took a look at the raw test results. What I saw was that two out of three of the DLCO tests had been performed with the correct inspired volume but that the one with a much lower inspired volume had a much larger VA and DLCO when compared to the other results. This got me scratching my head since the patient has severe COPD and that usually means that a lower inspired volume leads to a lower DLCO and VA. When I noticed the analyzer signals during the breath-hold period that’s when I could see right away why the results had been overestimated.