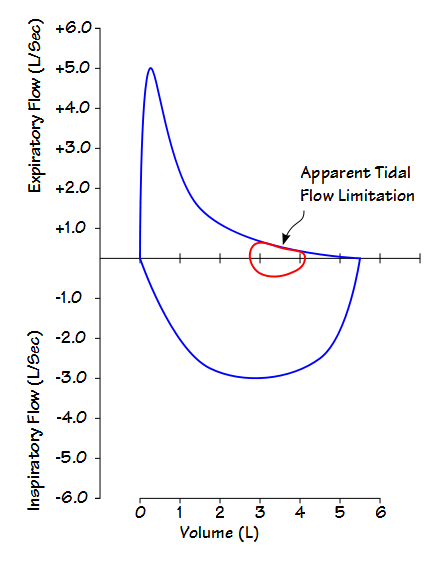
Expiratory flow limitation exists when increasing expiratory effort fails to increase the expiratory flow rate. This can been seen when a patient exhales along the same flow-volume curve during quiet, tidal breathing as they do during a forced expiratory effort. Tidal expiratory flow limitation (EFLt) is a key concept in understanding dyspnea, hyperinflation and orthopnea in patients with COPD and in assessing the functional severity of COPD.
The notion that EFLt could be detected through flow-volume loops was proposed in the 1960’s but subsequent research has shown this approach to be unreliable for a variety of moderately esoteric reasons which include the differences in static lung recoil and airway resistance that occur following a deep inhalation, differences in time-dependent lung emptying and the viscoelastic forces in the lung. When tidal flow limitation as seen on flow-volume loops is compared to other techniques it is apparent that flow-volume loops overestimate the presence of EFLt by approximately one-third.
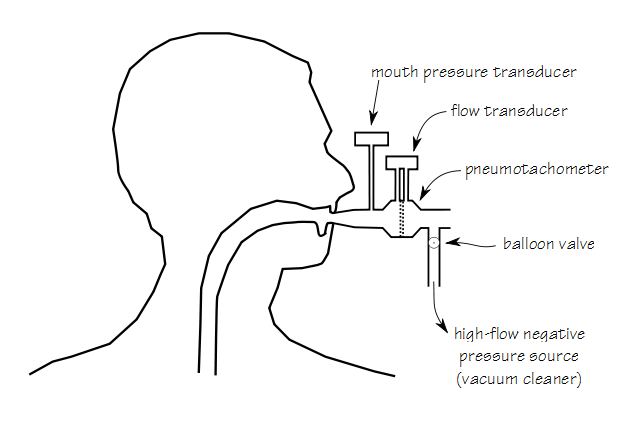
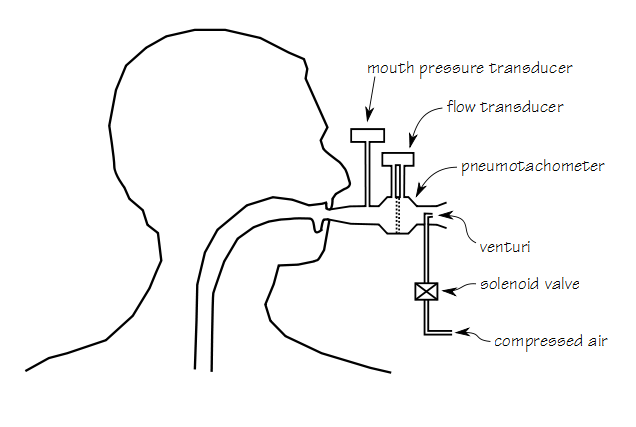
A particularly simple technique to detect EFLt, called Negative Expiratory Pressure (NEP) was developed in the mid-1990’s. In this technique a negative pressure of approximately -5 cm H2O is applied to a patient’s airway during a resting tidal exhalation. The negative pressure increases the gradient between the patient’s alveoli and their airway opening and will increase expiratory flow when there is no expiratory flow limitation. If the patient’s expiratory flow rate does not increase when negative pressure is applied then EFLt is present. A particular advantage of this technique is that it the patient breathes tidally throughout the test and does not need to perform any maximal expiratory efforts.
The apparatus for performing the NEP test is relatively simple. The patient breathes through a pneumotachograph while airway pressure is measured from a side tap between the patient mouthpiece and the pneumotach. In one version of the apparatus, on the far side of the pneumotach is a balloon-valve controlled source of negative pressure, typically a vacuum cleaner. Alternately, a venturi is supplied with solenoid valve-controlled compressed air.
To perform the test a patient breathes normally through the pneumotach. At the beginning of an exhalation the negative pressure is applied. At the end of exhalation the negative pressure is removed. This should be repeated several times until at least several quality tidal maneuvers have been performed and recorded. The maneuver should be performed with the patient sitting upright and while they are supine. It can also be performed during exercise on a treadmill or ergometer.
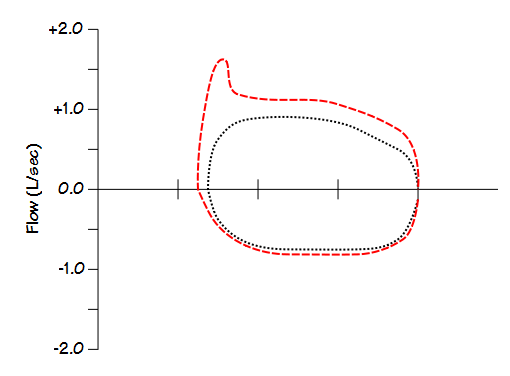
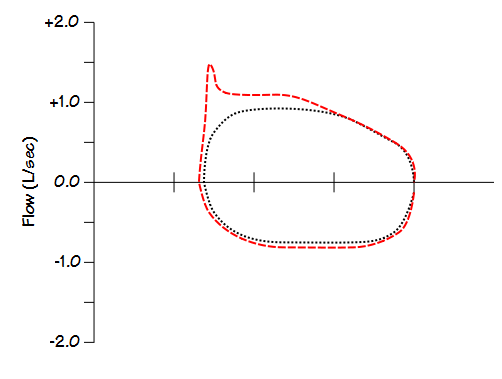
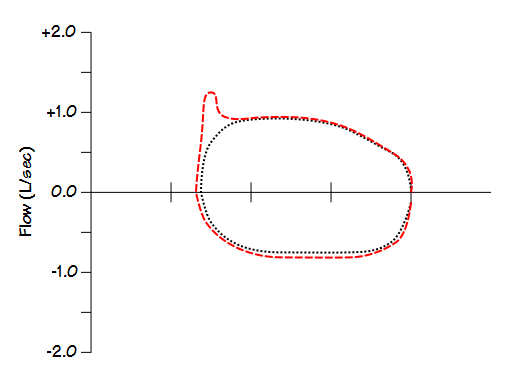
The control tidal loop and negative pressure loop are overlaid and the portion of the flow-volume loop where there was no appreciable increase in expiratory flow is considered as flow limted. This will always be less than 100% of the entire exhalation because during the beginning of exhalation flow is still increasing and it cannot be considered to be limited at that time. Additionally when the negative pressure is applied there is usually a “spike” which is considered to be the partial collapse of the extrathoracic airways and mouth.
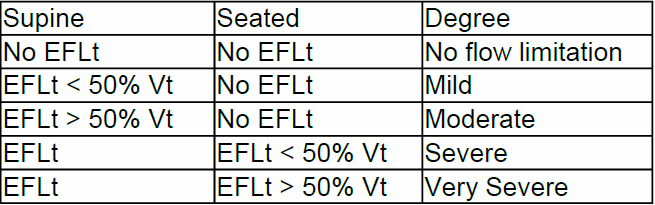
The Functional Residual Capacity (FRC) in patients with mild to moderate COPD is smaller in the supine position than when upright. For this reason EFLt is usually present in the supine position earlier in the disease process than it is in the upright position. Many COPD patients also suffer from orthopnea for the same reason.
The severity of EFLt can be categorized using the following scale:
There is a disparity in the symptoms of chronic dyspnea in patients with similar levels of COPD as assessed by spirometry in that patients with similar FEV1’s often have quite different levels of dyspnea. This dyspnea however, has been shown to correlate with the presence or absence of EFLt at rest much better than it does with FEV1. The presence of EFLt also correlates highly with dynamic hyperinflation. Expiratory flow limitation is an issue not just in COPD, but in chronic asthma, cystic fibrosis, obesity, heart failure and the elderly as well.
NEP is a relatively simple technique that is able to provide diagnostic and staging information regarding dynamic hyperinflation, dyspnea and orthopnea that is at least as valuable as FEV1. It was first described in the mid-1990’s and yet has not been adopted by clinical PFT Labs. I can’t speak for the rest of the world but in the United States there are probably at least two reason why this is the case.
First, there is no CPT procedure code for the NEP test. Without a CPT code for NEP testing insurers will not pay for the test. The test therefore can’t be billed and there is no revenue available from it. This is not the first time that CPT coding has put limitations on Pulmonary Function testing (you need look no further than CPT 94620 which applies to both pre- and post-exercise spirometry and to 6-minute walk tests and has caused a multitude of 6MWT billing rejections) and probably won’t be the last. The CPT coding system tends to be conservative and if the NEP test has been submitted for inclusion in the CPT coding system so far it has not happened.
Second, there are no commercially available NEP testing systems. The only existing NEP testing systems have been built by researchers. Although the NEP testing system is technically simple, building, calibrating and maintaining it is probably above the skill level of most pulmonary function labs.
Finally there may also be some hesitation regarding the interpretation of results. A NEP test produces graphical results that to a large extent must be interpreted by eye. How much difference or similarity should be allowed to exist between the NEP loop and the control tidal flow-volume loop before EFLt is considered to present has not been well defined. Additionally, one technical issue in the measurement is that most investigators align the control loop and NEP loop based on the position of the patient’s end-inhalation. This may or may not be valid but the loops cannot be aligned at end-exhalation because the application of NEP always causes tidal volume to increase.
I think that NEP testing is a valuable technique and that any Pulmonary Function lab that has the resources and technical ability should consider performing it clinically. Perhaps when enough labs adopt this test then CPT codes and commercial test systems will become available.
References:
Calverley PMA, Koulouris NG. Flow limitation and dynamic hyperinflation: key concepts in modern respiratory physiology. Eur Respir J 2005; 25: 186-199.
de Bisschop C, Marty ML, Tessier JF, Berberger-Gateau P, Dartigues JF, Guenard H. Expiratory flow limitation and obstruction in the elderly. Eur Resp J 2005; 26: 594-601
Duguet A, Tantucci C, Lozinguez O, Isnard R, Thomas D, Zelter M, Derenne JP, Milic-Emili J, Similowski T. Expiratory flow limitation as a determinant of orthopnea in acute left heart failure. J Amer Coll Card 2000; 35: 690-700.
Eltayara L, Becklake MR, Volta A, Milic-Emili J. Relationship between chronis dyspnea and expiratory flow limitation in patients with chronic obstructive pulmonary disease. Am J Resp Crit Care Med 1996; 154 1726-1734.
Eltayara L, Ghezzo H, Milic-Emili J. Orthopnea and tidal expiratory flow limitation in patients with stable COPD. Chest 2001; 119: 99-104.
Koulouris NG, Valta P, Laoie A, Corbeil C, Chasse M, Braidy J, Milic-Emili J. A simple methoud to detect expiratory flow limitation during spontaneous breathing. Eur Respir J 1995; 8: 306-313.
Koulouris NG, Dimopoulou I, Valta P, Finkelstein R, Cosio MG, Milic-Emili J. Detection of expiratory flow limitation during exercise in COPD patients. J Appl Physiol 1997; 82: 723-731.
Koulouris NG, Hardavella. Physiological techniques for detecting expiratory flow limitation during tidal breathing. Eur Respir Rev 2011; 20: 121, 147-155.
Pellegrino R, Brusasco V. Lung hyperinflation and flow limitation in chronic airway obstruction. Eur Respir J 1997; 10: 543-549.
Tantucci C. Expiratory flow limitation definition, mechanisms, methods, and significance. Pulmonary Medicine 2013; Article ID 749860.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

Mr. Johnston,
Please consider reviewing this again, especially as it pertains to cardiopulmonary exercise testing.
Do you use it during exercise testing?
Thank you
Dr. Sullivan –
No, I don’t use NEP for either spirometric or exercise testing. I’m not involved in any research at the moment and I think that for routine clinical CPETs monitoring the EELV is adequate for determining whether expiratory flow limitation is affecting exercise capacity. There are only about a half dozen or so articles combining NEP and exercise so I’ll have to review them when I have some time (too many other projects in my queue at the moment) and see if there’s anything worth adding to what I’ve already written.
Regards, Richard