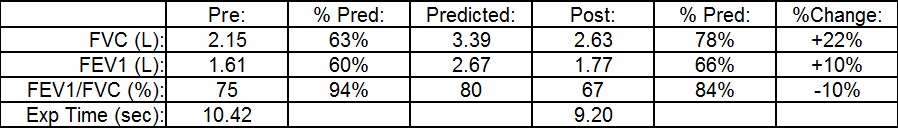
The current ATS/ERS guidelines require that an individual have a post-bronchodilator increase in FEV1 or FVC of at least 12% and 200 ml in order for it to be considered a significant response. Numerous studies have shown however, that many patients that don’t meet these criteria, particularly those with COPD, do have a clinically significant improvement with bronchodilators.
The September 2014 issue of Chest had a point-counterpoint set of editorials on this standard and on assessing the response to bronchodilator in general. Both sides had a number of interesting things to say but to a large extent one side was talking apples (physiology) and the other side oranges (statistics). I actually think that both sides feel there are significant problems with the ATS/ERS standards, they just differ in what they think is wrong and in the best way to fix it.
One statistical argument was that the ATS/ERS guideline is a one-size-fits-all solution that is designed more to detect asthmatic-type responses than the more subtle changes that can occur in individuals with COPD that although small, are clinically relevant. I am inclined to agree with this but as much as I and others think that the current ATS/ERS standard likely needs revision the difficulty with this is that spirometry is a “noisy” measurement with a lot of variability.
Spirometry variability and the limits to its accuracy comes from issues to familiar to all of us:
- the patient’s ability to understand and perform spirometry
- the technician’s ability to encourage and guide a patient through a spirometer maneuver
- the spirometer’s ability to measure exhaled flow and volume accurately
“Noise” is one of the reasons why it can be difficult to determine statistically and clinically significant changes. It’s also why the threshold for significant post-bronchodilator change is set as high as it is and may also be the reason why it shouldn’t be lowered.
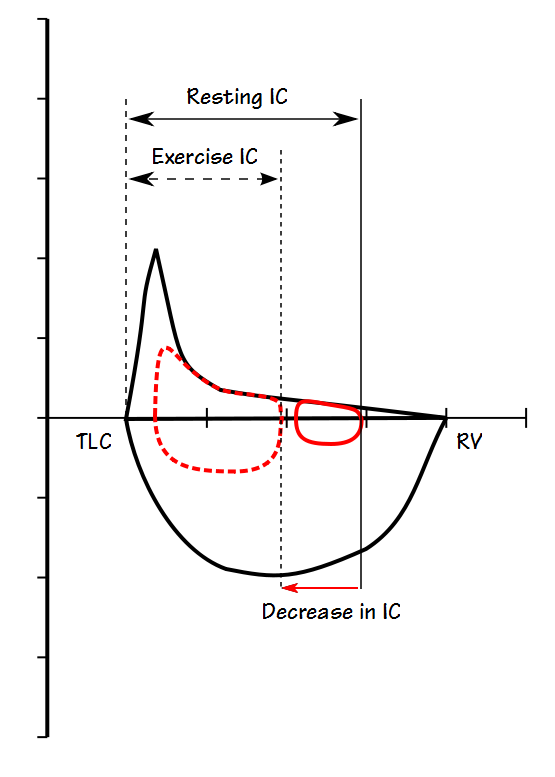
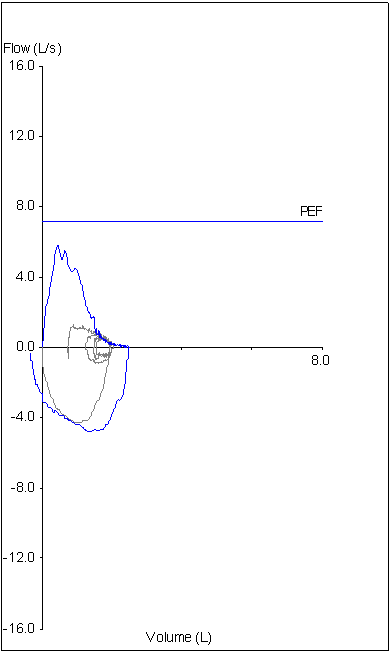
Even though there may be reasons why the ATS/ERS guidelines for post-bronchodilator improvements in FEV1 and FVC shouldn’t be revised at the very least they need to become more inclusive and consider more factors. There is too much emphasis placed on the changes in FEV1 and FVC as the sole indication for a response to bronchodilator particularly since there are other ways in which a response can be measured.
Continue reading →