Patients with COPD often have a ventilatory limitation as their primary limitation to exercise. A ventilatory limitation to exercise has traditionally been assessed by the breathing index or the breathing reserve:
breathing index = Peak Ve / Predicted MVV
breathing reserve = 1 – (Peak Ve / Predicted MVV)
which are basically two different ways of saying the same thing. In either case a breathing index greater than 85% or breathing reserve less than 15% is an indication that a patient has reached a ventilatory limit to exercise. There is some disagreement as to whether the predicted MVV should come from a MBC test performed by the patient or from the patient’s FEV1 x 40. I have tried both approaches and my experience has been that FEV1 x 40 is the best indicator for a patient’s predicted MVV. This is also Wasserman’s (my go-to source for exercise testing) recommendation so this is what we use.
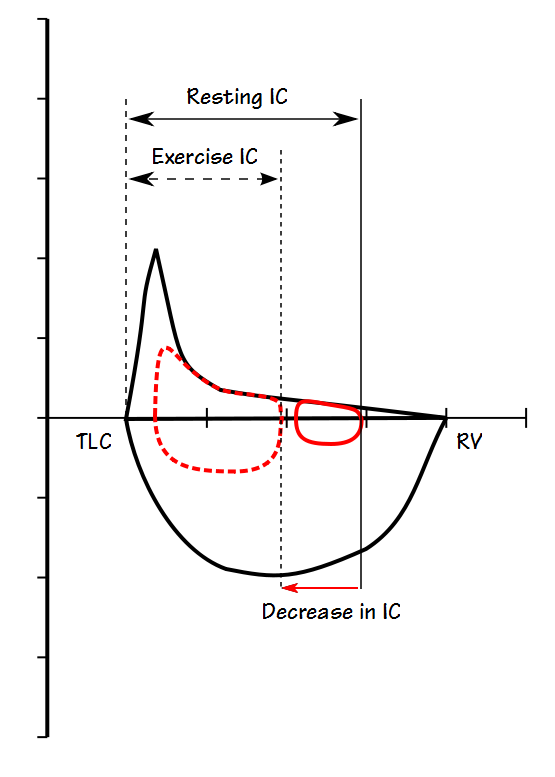
Individuals with COPD are occasionally hyperinflated at rest (i.e. elevated FRC and RV) and more commonly they dynamically hyperinflate during exercise. Research has shown that those individuals with are flow-limited during tidal breathing at rest almost always hyperinflate with exercise. Patients who are not flow-limited at rest but still have a low FEV1 and FEV1/FVC ratio may also hyperinflate. Because hyperinflation limits a patient’s tidal volume response to exercise it may cause an individual to have a limitation to exercise that occurs at a minute volume below the 85% threshold.
Since TLC probably remains constant during the course of an exercise test, the measurement of Inspiratory Capacity (IC) during exercise is a way of tracking changes in FRC (or more accurately the End-Expiratory Lung Volume, EELV). We routinely measure IC during cardiopulmonary exercise tests in order to determine whether hyperinflation is occurring and there are a variety of way to look at IC and its effect on ventilation:
- Change in IC (L)
- Percent change in IC (baseline – measured/baseline)
- Vt/IC
- IC/TLC
- EILV/TLC
Because we do not measure TLC as part of a CPET and only rarely does a patient have a TLC measurement that was performed recently, we do not use any comparisons that depend on TLC. We also feel that the percent change in IC is overly sensitive to the baseline IC and for this reason we look at just the change in IC (L) and the Vt/IC ratio.
When we perform a CPET we try to obtain at least two acceptable IC measurements at baseline and then at approximately two minute intervals during exercise. Unfortunately our test system’s software does not report the IC results immediately, only in the CPET reports, which makes it difficult to assess the quality and repeatability of these trial efforts. The best we can do is “eyeball” the graphs during the IC maneuver and correct the patient only if there are obvious problems.
At the present time there are no accepted normal values for changes in IC during exercise. Based on the results we’ve seen in several studies we’ve decided that a decrease in IC of 0.25 L or greater is a significant change and an indication that hyperinflation is probably occurring. We use the Vt/IC ratio to help determine whether hyperinflation, when it occurs, may be causing a ventilatory limitation. Specifically, a normal maximum Vt/IC ratio is usually 0.75 or less. The work of breathing rapidly increases at Vt/IC ratios greater than 0.85 so for this reason, we’ve use a Vt/IC ratio of 0.85 or above as an indication the patient has reached his maximum useable tidal volume.
When a patient hyperinflates this usually occurs more or less steadily throughout the exercise and this is the pattern we look for. For this reason, we tend to discount a significant change in a single IC measurement, particularly if it is the last measurement obtained during exercise and none of the previous IC measurements had shown any particular change.
Recently a CPET report came across my desk that showed a steady decrease in IC throughout exercise, with a final IC measurement that was 0.55 L less than baseline.
So why didn’t I believe that the patient was really hyperinflating?
First and most importantly, the patient’s baseline spirometry was normal. The FVC was 106% of predicted and the FEV1 was 107% of predicted and there was no significant change in either of these values following exercise. You can’t measure expiratory flow limitation with spirometry, but results like this make obstructive gas trapping exceedingly unlikely.
The CPET system’s software measures the IC automatically but because errors are not all that uncommon I usually re-measure and verify the IC volumes. When I reviewed this patient’s IC maneuvers I found was that the reported IC values were accurate but a look at the other ventilatory results showed why at the same time they probably weren’t “accurate” at all.
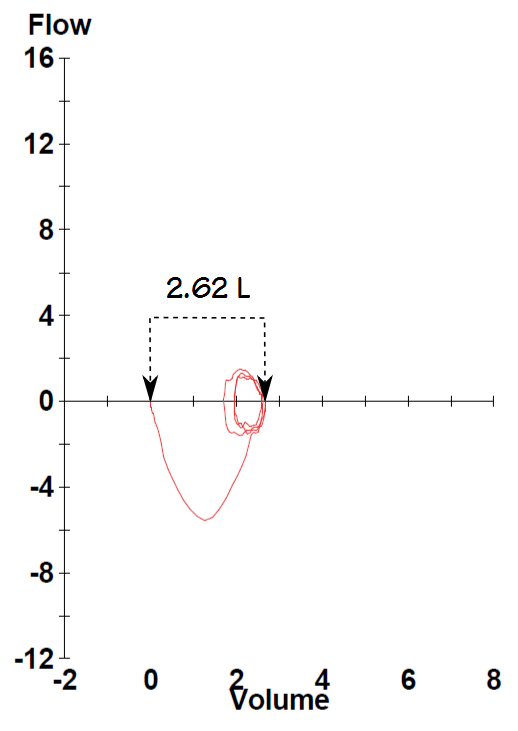
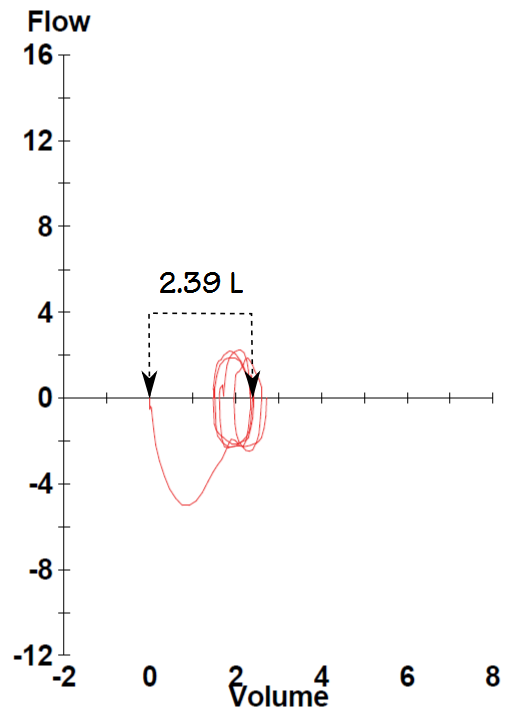
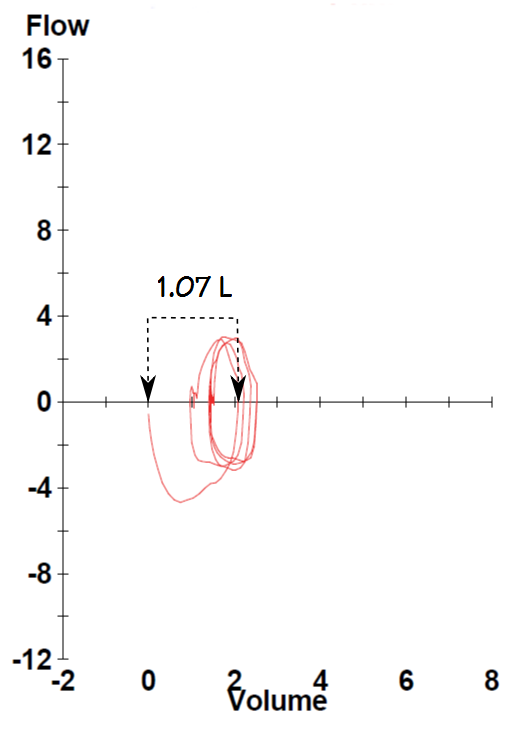
During a normal ventilatory response to exercise tidal volume usually increases first and usually by at least two to three times the baseline tidal volume. Respiratory rate usually increases second and only after tidal volume has more or less plateaued. In this case the patient’s tidal volume only increased slightly from their baseline value and most of the increase in minute ventilation was from an increase in respiratory rate. At peak exercise their respiratory rate was 56 and their tidal volume was only about 50% greater than it was at baseline. This is a markedly inefficient ventilatory response to exercise.
This pattern of a low tidal volume and high respiratory rate is a hallmark of restrictive lung disease but when this occurs the Vt/IC ratio is usually quite high (0.85 or above) and the maximum minute ventilation is usually above 85% of predicted. This patient’s Vt/IC ratio was 0.46 however, and therefore had the ability to significantly increase their tidal volume but for some reason wasn’t doing so. The patient’s maximum minute ventilation was also 63% of predicted. Despite the low tidal volume and high respiratory rate their overall minute ventilation was normal. So why was their IC decreasing?
It is possible that because of the high respiratory rate the patient was “stacking” breaths and actually breathing at a higher lung volume. In a sense this is hyperinflation, but if this was the case there was no apparent physiological reason for it to be occurring.
What I think is far more likely however, is that because of the high respiratory rate the patient was unable to perform an adequate IC maneuver. I’ve noticed that towards the end of a CPET, when patients get to very high respiratory rates, the final IC measurement is often significantly lower than all the others and is often the only IC measurement that showed any decrease. We almost always ignore the final IC measurement when this occurs. In this case however, the patient was at a high respiratory rate throughout testing and the IC measurements were taken at respiratory rates of 39, 47 and 53 breaths per minute.
We see this inefficient ventilatory response (low tidal volume, high respiratory rate) several times a year and it usually occurs for no apparent reason that we can see. It could be anxiety (but many patients are anxious and don’t breathe this way). It could be that the CPET is so “unnatural” that some patients feel they have to adopt an “unnatural” ventilatory pattern in order to cope with it. It could be that these patients have an elevated CO2 drive and can’t complete a normal exhalation before urgently needing to inhale again. It also could be a “learned response” in that they were either taught or decided on their own that this was the best way to increase their breathing during exercise. Regardless of the reason, this type of ventilatory response may well be why these patients are short of breath in the first place.
IC maneuvers cannot be repeated too frequently since they can skew a patient’s ventilatory pattern and their EELV. Because the IC manuever can only be performed a few times the quality of each IC measurement depends a lot on patient cooperation and effort. Patients should be given the opportunity to practice the maneuver at least a couple of times before starting the CPET and care should be taken when cuing the patient to perform the IC maneuver during exercise.
There should be at least some selectivity about deciding whether IC maneuvers should be performed in the first place. We get patients with COPD for pre-op exercise testing fairly often. For these patients the CPET is not really a diagnostic test per se but part of a surgical risk assessment and their max VO2 and Ve-VCO2 slope are what’s important, not dynamic hyperinflation.
It could be argued that there is no need to perform IC maneuvers in patients with normal spirometry who, for this reason, are unlikely to hyperinflate. The problem with this is that spirometry alone cannot determine whether or not expiratory flow-limitation is present. Even when flow-limitation and hyperinflation is not present IC maneuvers can provide additional information about an individual’s ventilatory response to exercise. For these reasons, unless there is an overwhelming reason not to we routinely perform IC maneuvers on all of our CPET patients.
Decreases in IC during exercise can indicate dynamic hyperinflation and this can be an important factor in a patient’s exercise limitation. Decreases in IC can also occur however, because of suboptimal IC maneuver quality or peculiar breathing patterns, so some care must be taken when assessing IC measurements. In this particular case the final report included the notation that the patient appeared to hyperinflate during exercise but that their low Vt/IC ratio showed that this was not a limitation.
References:
ATS/ACCP Statement on Cardiopulmonary Exercise Testing. Am J Resp Crit Care Med 2003; 167(1): 211-277
Calverley PMA. Dynamic hyperinflation. Is it worth measuring? Proc Am Thor Soc 2006; 3: 239-244.
Ferguson GT. Why does the lung hyperinflate? Proc Am Thor Soc 2006; 3: 176-179.
Fujimoto K, Yoshiike F, Yasua M, Kitaguchi Y, Urushihata K, Kubo K, Honda T. Effects of bronchodilators on dynamic hyperinflation in patients with COPD. Respirology 2007; 12: 93-99.
O’Donnell DE, Lam M, Webb KA. Measurement of symptoms, lung hyperinflation and endurance during exercise in chronic obstructive pulmonary disease. Am J Resp Crit Care Med 1998; 158(5): 1557-1565.
O’Donnell DE, Revill SM, Webb KA. Dynamic hyperinflation and exercise intolerance in chronic obstructive pulmonary disease. Am J Resp Crit Care Med 2001; 164(5): 770-777.
Pellegrino R, Brusasco V, Rodarte JR, Babb TG. Expiratory flow limitation and regulation of end-expiratory lung volume during exercise. J Appl Physiol 1993; 74(5): 2552-2558.
Wasserman K, et al. Principles of exercise testing and interpretation. Published by Lippincott, Williams & Wilkins, 2005.
Yan S, Kaminski D, Sliwinski P. Reliability of inspiratory capacity for estimating end-expiratory lung volume chanes during exercise in patients with chronic obstructive pulmonary disease. Am J Resp Crit Care Med 1997; 156(1): 55-59.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.