Although the technology used to perform the single-breath DLCO test has improved since it was first developed in the 1950’s the essential concepts and equations have not changed significantly. Probably the most important advance has been the introduction of rapid response real-time gas analyzers in the 1990’s. Prior to that time the patient’s washout and sample volumes had to be preset which always involved a certain amount of guesswork when a patient was significantly obstructed or restricted. With a real-time gas analyzer it is possible inspect the exhaled gas tracings after the test has been performed in order to determine when washout has occurred and then select the appropriate location for the sample volume. This has improved the single-breath DLCO test quality but at the same time it has also exposed some of its limitations.
The single-breath DLCO test attempts to simplify what is actually a very complex process. One of the key assumptions of the single-breath DLCO calculations is that the inspired gas mixture is evenly distributed throughout the lung. This is not really true even for patients with normal lungs and in general, inspired gas follows the last in-first out rule. In patients with lung disease this inhomogeneous filling and emptying can be magnified and a maldistribution of ventilation is often most evident in patients with COPD.
A second key assumption is that a small sample of exhaled air taken near the beginning of exhalation (the alveolar sample) can accurately represent the entire lung. The reason that it is necessary to rely on a small sample rather than the entire exhaled volume has to do mostly with time. The length of time that the inspired gas sample resides in the patient’s lung (breath-holding time, BHT) needs to be determined fairly precisely. Since an entire exhalation is presumed to take on the order of 6 seconds (or longer, of course) then at what point do you stop measuring time? Beginning? Middle? End? By using a small sample of exhaled air near the beginning of exhalation when flow rates are relatively high and a gas sample can be acquired in a short period of time it is possible to be more precise. Even so there have been different approaches to measuring the end of the BHT. The current ATS-ERS standard recommends the Jones-Meade approach which uses the middle of the alveolar sampling period as the end of BHT, whereas both the Ogilvie and ESP approach used the beginning of the alveolar sampling period. The selection of BHT technique has been shown to produce measurable and systematic differences in calculated DLCO but regardless of this a small sample reduces the error bar.
The insoluble component of the DLCO test gas mixture (which is most often methane in systems with real-time gas analyzers) is used to calculate VA and this is where the problems of ventilation inhomogeneity and a small exhaled gas sample converge.
The exhaled gas waveforms from a patient without lung disease typically has a flat methane tracing which indicates that the inhaled gas mixture was well mixed within their lungs. This is confirmed by the fact that their VA is usually almost the same as their TLC.
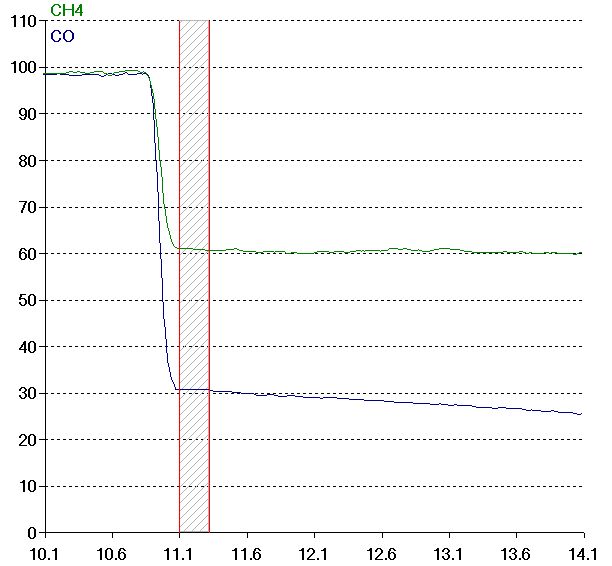
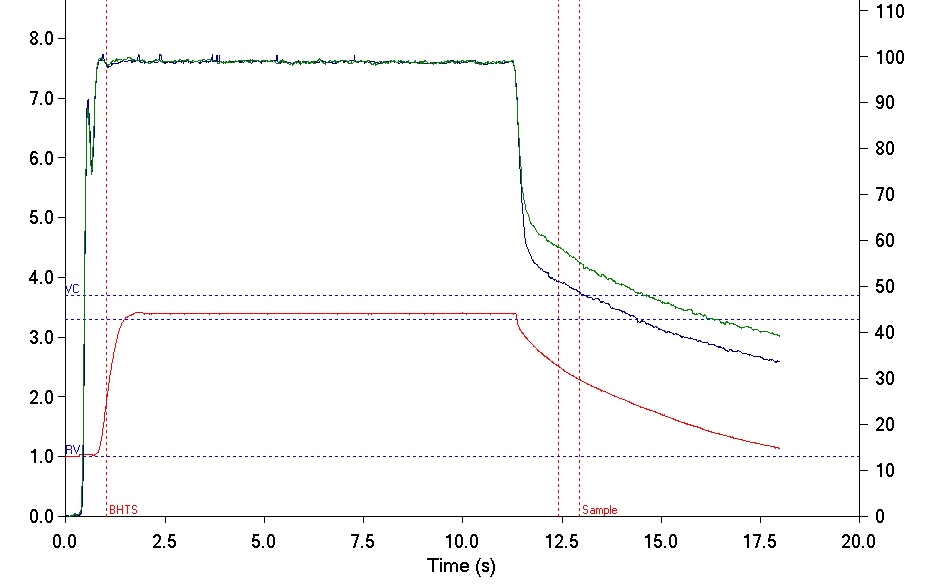
In contrast the exhaled gas waveforms from a patient with COPD often has a methane tracing that decreases throughout exhalation and a VA that is noticeably lower than their TLC. This shows that the inhaled gas mixture was unevenly distributed in their lungs.
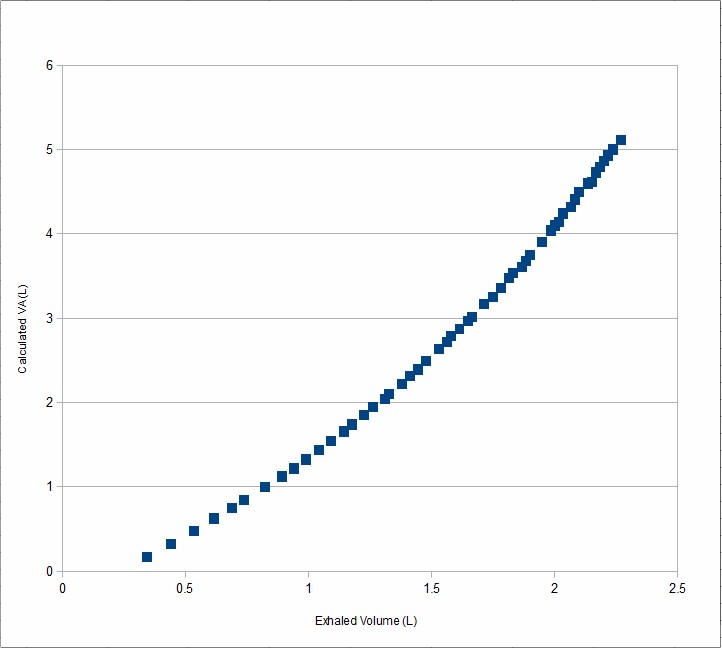
Since the methane concentration varies throughout exhalation it is apparent that VA will be quite different depending on where the methane is measured. The following graph uses data taken from the above exhaled gas and volume tracings to show how the calculated VA varies during exhalation.
The ATS-ERS statement on DLCO testing allows for a certain amount of variability in both washout and sample volumes. For a vital capacity greater than 2.0 liters, washout can be from 0.75 to 1.00 liter and the sample can be from 0.50 liter to 1.00 liter. In patients with normal lungs variations in washout and sample volume within ATS-ERS guidelines are unlikely to make any significant difference in calculated DLCO.
In patients with COPD however, VA is usually significantly less than TLC and there tends to be a direct correlation between the degree of airway obstruction and the difference in VA and TLC. {see Single Breath TLC Measurements} This raises the question as to just how how much the low DLCO seen in patients with COPD is due to the actual lung disease and how much is due to a low VA. The answer, somewhat surprisingly, is that the variation in DLCO is much smaller than the change in VA over a wide range of washout volumes. This means that a DLCO using the ATS-ERS guidelines is (probably) both reasonably correct and reasonably appropriate to the degree of lung disease.
This is not to say there is no difference. DLCO measured using an alveolar sample from late in the exhalation of a COPD patient tends to be higher than when measured from an alveolar sample from early in the exhalation. This increase is largely attributable to the larger VA measured from that part of the exhalation. Patients with normal lungs however, show the opposite pattern. DLCO decreases when using an alveolar sample from late in exhalation and this is probably due to the fact that it comes in part from a period when lung volume and the corresponding surface area are lower.
The difference between VA and TLC can provide an index into ventilation inhomogeneity but it is unclear how reproducible this measurement is and how sensitive it is to overall DLCO test quality and in particular, inspired volume. In patients with normal lungs, assuming that inhalation during the DLCO maneuver is to TLC, VA is relatively insensitive to inspired volume. In patients with COPD I suspect that the measured VA is going to be dependent on how close a patient is able to get to RV before inhaling to TLC. But just as importantly as all this, it’s unclear what a VA/TLC index is actually measuring and what its clinical relevance is.
Prediletto et al suggest the use of an index, Delta VA/Ve, that is the change in the percentage of VA per liter of exhaled gas. They note that higher values of this index indicate increasing maldistribution of ventilation. This may be an improvement over the VA/TLC ratio but it is not clear to me that Delta VA/Ve relationship is linear over the range of exhaled volume.
Since VA is sensitive to washout volume in patients with COPD, this means that DLCO/VA (KCO) is going to be similarly sensitive. Although DLCO/VA has its place in assessing gas exchange (mostly in restrictive lung disease) I think that its use in patients with COPD is suspect. {see DL/VA is really K in disguise.}
Before rapid-responding, real-time gas analyzers came into widespread use in clinical DLCO testing the dependence of VA on washout volume in patients with ventilation inhomogeneities was known by researchers but little could be done about it during routine measurements. Now we can routinely see its effects but it is not clear that what should be done about it. Several different approaches have been proposed to improve the accuracy of DLCO measurements in general and COPD in particular but there is no consensus at this time. I suspect that a future answer, if any, will depend on integrating DLCO and VA over the entire exhalation.
In my lab the general recommendation to technicians is that whenever it is difficult to determine where the alveolar plateau begins (i.e., when the methane line gently slopes downwards and there is no distinct alveolar plateau) to default to a 1.00 liter washout and 0.50 liter sample volume in order to standardize results as much as possible. This is not a perfect answer but it at least acknowledges the problem and attempts to contain it.
References:
Beck KC, Offord KP, Scanlon PD. Comparison of Four Methods for Calculating Diffusing Capacity by the Single Breath Method. Chest 1994; 105:594-600
Brusasco V, Crapo R, Viegi G editors. ATS/ERS Task Force: Standardization of Lung Function Testing. Standardization of the single-breath determination of carbon monoxide uptake in the lung. Eur Resp J 2005; 26:720-735
Dressel H, Filser L, Fishcher R, de la Motte D, Steinhaeusser W, Huber RM, Nowak D, Jorres RA. Lung diffusing capacity for nitric oxide and carbon monoxide: Dependence on breath-hold time. Chest 2008; 133:1149-1154
Ferris BG, ed. Epidemiology Standardization Project. Am Rev Resp Dis 1978; 118:6(Part 2;1-120)
Graham BL, Mink JT, Cotton DJ. Overestimation of the Single-Breath Carbon Monoxide Diffusing Capacity in Patients with Air-Flow Obstruction. Am Rev Resp Dis 1984; 129:403-408
Graham BL, Mink JT, Cotton DJ. Effect of breath-hold time on DLCO(SB) in patients with airway obstruction. J Appl Physiol 1985; 58:1319-1325
Jones RS, Meade FA. Pulmonary Diffusing Capacity: an improved single-breath method. Lancet 1:94-95
Leech JA, Martz L, Liben A, Becklake M. Diffusing Capacity for Carbon Monoxide: The Effects of Different Derivations of Breathold Time and Alveolar Volume and of Carbon Monoxide Back Pressure on Calculated Results. Am Rev Resp Dis 1985; 132:1127-1129
Ogilvie CM, Forster RE, Blakemore WS, Morton JW. A Standardized Breath Holding Technique For The Clinical Measurement Of The Diffusing Capacity Of The Lung For Carbon Monoxide. J Clin Invest 1957; 36:1-17
Prediletto R, Fornai E, Catapano G, Carli C. Assessment of the alveolar volume when sampling exhaled gas at different expired volumes in the single breath diffusion test. BMC Pulmonary Medicine 2007; 7:18

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.