Re-breathing DLCO may not be well known because this technique has not been used in routine clinical testing. It has instead been primarily used to research diffusing capacity during exercise because it is able to do this without the need to interrupt or significantly alter a subject’s breathing pattern.
Re-breathing DLCO is probably best thought of as a hybrid between the single-breath DLCO and steady-state DLCO techniques. The gas mixture and calculations are from the single-breath world but the breathing pattern is more from the steady-state side of the family.
In order to perform a re-breathing DLCO test, a rubber bag is filled with a standard single-breath DLCO gas mixture (usually 0.3% CO, 10% He, 21% O2, balance N2). The volume of the bag is adjusted to the subject so that it empties at end-inhalation with every breath. At the end of an exhalation the subject is switched into the bag who then hyperventilates at a rate of approximately 30 breaths per minute.
During the first several breaths, carbon monoxide and helium undergo dilution and equilibration with the patient’s FRC. An initial carbon monoxide reading is taken at this time and used as a baseline. The test usually continues for another 30 seconds or so after the baseline measurements are taken and the subject is then switched out of the breathing circuit. DLCO is then calculated by:
where:
Pb = barometric pressure
T = length of the re-breathing period, in minutes
FACO1 = fractional CO at beginning of re-breathing period (after initial equilibration between lungs and bag)
FACO2 = fractional CO at end of re-breathing period
Lung and bag volume is calculated by:
where:
Vbag = initial volume of gas in bag (ml STPD)
FIHe = fractional He in bag before re-breathing started
FAHe = fractional He in bag at end of re-breathing period
There are several re-breathing DLCO techniques which vary primarily by bag and tidal volume size, gas mixture, and breathing circuit details. Most researchers have developed a testing circuit that continuously samples the gas mixture. In part this is because determining the baseline is relatively straightforward. After the first couple of breaths, when the mixing of gas in the bag and in the subject’s lungs has been completed, the CO concentrationdeclines linearly when plotted using a semi-log scale. The beginning of this linear period is then used as the baseline.
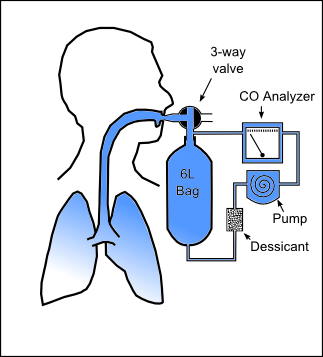
In a version of this developed by Lewis et al, a pump was used to continuously circulate gas from the re-breathing bag through a carbon monoxide analyzer during the test.
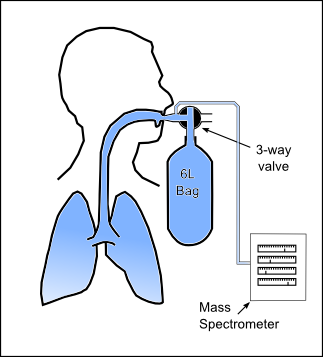
Another version developed by Sackner et al, used a mass spectrometer to continuously sample the re-breathing gas mixture. Although a mass spectrometer has several advantages, in particular a small sampling rate (approximately 15 ml/min), carbon monoxide and nitrogen have essentially the same mass. For this reason, carbon monoxide using a stable isotope of oxygen, oxygen-18, must be used.
In this system a 6 liter bag was filled with 3.5 liters of test gas. The gas mixture used was 10% helium, 0.3% C18O, 0.5% acetylene, 21% oxygen, balance nitrogen and they were able to measure DLCO, tissue volume, pulmonary capillary blood flow (Qc), membrane diffusing capacity (DMCO) and pulmonary capillary blood volume (Vc) at rest and during exercise.
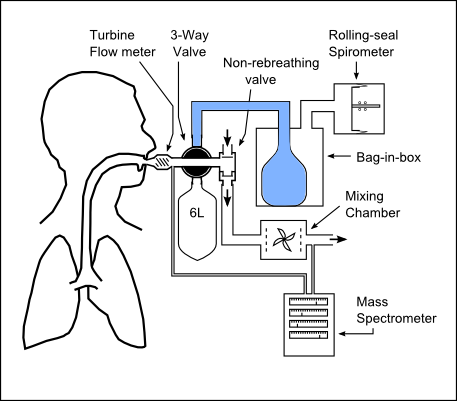
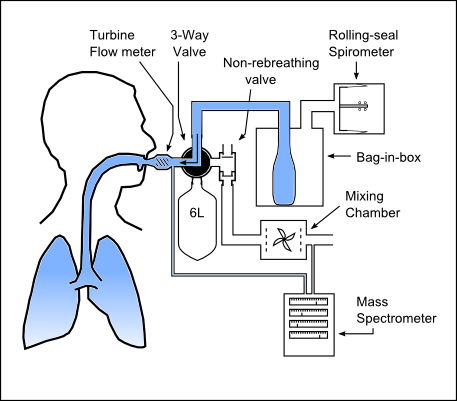
Hsia et al developed a complicated but still quite elegant system capable of measuring re-breathing DLCO, tissue volume, pulmonary capillary blood flow, DMCO and pulmonary capillary blood volume at rest and during exercise. This system is also capable of measuring the normal cardiopulmonary exercise values such as tidal volume, minute volume, respiratory, oxygen consumption and CO2 production.
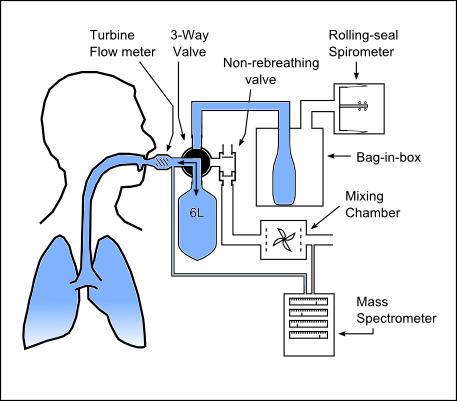
The basic exercise testing components consists of a turbine flow meter, non-re-breathing valve, mixing chamber and mass spectrometer. Added to this is a pneumatically actuated 3-way valve, a 6 liter bag, a bag-in-box and a volume displacement spirometer. The system is prepared by evacuating the 6 liter bag and filling the bag-in-box with the test gas mixture. Test gas mixtures typically used were 9% helium, 0.3% C18O, 6% acetylene and either 30% O2 in N2 or 90% O2.
At the end of a normal exhalation, the pneumatically-actuated 3-way valve switches the patient to the bag-in-box system and they inhale to TLC. The pneumatically actuated valve then switches the patient to the 6 liter bag and the patient re-breathes for a period of 15 or 16 seconds.
An advantage of this system is that the re-breathing bag volume is not pre-filled but instead determined by the subject’s inhalation from the bag-in-box system. This system has since been updated to use an infrared analyzer rather than a mass spectrometer making the C18O test mixture unnecessary.
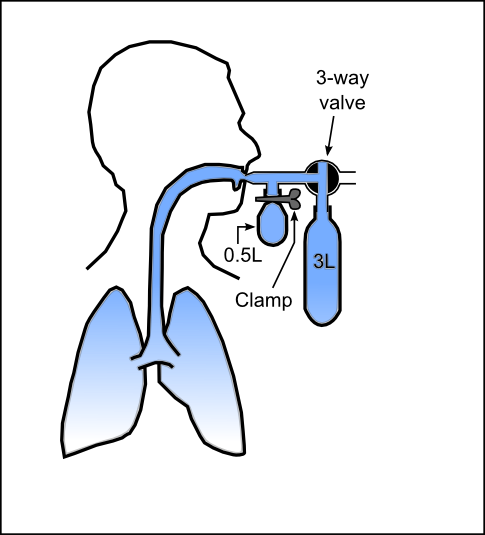
A low-tech approach was developed by Marshall. The breathing circuit for this technique uses two rubber bags instead of one. In addition to a 3 liter rubber bag is used for re-breathing, the circuit contains a smaller 500 cc bag that is used for obtaining the initial equilibrated gas sample from the beginning of the re-breathing period.
To prepare for the test, the 3 liter bag is filled with 2 liters of the diffusing gas mixture and the 500 ml sample bag is evacuated and clamped so that it cannot refill. To perform the test, at the end of exhalation, the patient is switched into the re-breathing circuit. The patient then hyperventilates. After approximately 10 seconds into the re-breathing period the clamp to the 500 cc sample bag is opened. Once the sample bag is filled, it is again clamped closed. The patient continues to hyperventilate and 20 seconds later is switched out of the breathing circuit. After the test has ended the bags are analyzed for CO and helium.
Re-breathing DLCO results are lower than single-breath DLCO measurements in the same patients. This appears to be mainly due to the fact that re-breathing measurements are made at lower lung volumes than single-breath measurements and at least one researcher has shown that the results agree when made at the same lung volume.
Although the hyperventilation that occurs during the re-breathing maneuver is not a natural breathing pattern proponents have pointed out that re-breathing DLCO is relatively independent of minute ventilation and that respiratory rates between 15 and 60 do not affect calculated DLCO.
A major assumption of the re-breathing technique is that the gases in the lung and in the re-breathing bag equilibrate during the maneuver and that the CO concentration in the re-breathing bag is therefore an accurate indication of mean alveolar PCO. This assumption is probably not valid when significant obstructive disease or other maldistribution of ventilation is present, but the same criticism can also be applied to all DLCO techniques.
A criticism of the re-breathing DLCO technique is that lung volume changes constantly during testing. This means that the test gas mixture is in contact with the maximum alveolar-capillary surface area only during part of the breathing cycle and may be an additional reason why re-breathing DLCO results are lower than single-breath DLCO results. A related issue is that the re-breathing DLCO calculation may be overly simplistic due to the fact that a basic assumption in the formula is that lung volume is constant and at end-inhalation.
The re-breathing technique will probably never be used clinically because the results are related to the lung volume at which the test is performed and this limits the ability to interpret results. Its primary value lies in being able to measure DLCO during exercise or any other situation where the patient’s breathing pattern should not be interrupted. Although it has limited applications, it’s still an interesting technique that pulmonary technologists should be aware of.
References:
Barazanji KW, Ramanathan M, Johnson RL, Hsia CCW. A modified re-breathing technique using an infrared gas analyzer. J Appl Physiol 1996; 80:1258-1262
Chance WW, Rhee C, Yilmaz C, Dane DM, PrunedaML, Raskin P, Hsia CCW. Diminished Alveolar Microvascular reserves in Type 2 Diabetes reflect systemic Microangiopathy. Diabetes Care 2008; 31:1596-1601
Clark EH, Jones HA, Hughes JMB. Bedside re-breathing technique for measuring carbon monoxide uptake by the lung. Lancet 1978; 1:791-793
Dujic Z, Eterovic D, Denoble P, Krstacic G, Tocilj J. Lung diffusing capacity in a hyperbaric environment: assessment by a re-breathing technique. Br J Indust Med 1992; 49:254-259
Felton C, Rose GL, Cassidy SS, Johnson RL. Comparison of Lung Diffusing Capacity during re-breathing and During Slow Exhalation. Resp Physiol 1981; 43:13-22
Hijazi OM, Ramanathan M, Estrera AS, Peshock RM, Hsia CCW. Fixed maximal stroke index in patients after pneumonectomy. Am J Respir Crit Care Med 1998; 157:1623-1629
Hsia CCW, Ramanathan M, Estrera AS. Recruitment of Diffusing Capacity in Patients after Pneumonectomy. Am Rev Resp Dis 1992; 145:811-816
Hsia CCW, McBrayer DG, Ramanathan M. Reference Values of Pulmonary Diffusing Capacity during Exercise by a re-breathing Technique. Am J Respir Crit Care Med 1995; 152:658-665
Lewis BM, Lin TH, Noe FE, Hayford-Welsing EJ. The measurement of pulmonary diffusing capacity for carbon monoxide by a re-breathing method. J Clin Invest 1959; 38:2073-2086
Marshall R. A re-breathing Method for Measuring Carbon Monoxide Diffusing Capacity: A Supplement to the Single-breath Method. Am Rev Resp Dis 1977; 115:587-589
Rose GL, Cassidy SS, Johnson RL. Diffusing capacity at different lung volumes during breath holding and re-breathing. J Appl Physiol 1979; 47:32-37
Russell NJ, Bagg LR, Dobrzynski J, Hughes DTD. Clinical assessment of a re-breathing method for measuring pulmonary gas exchange. Thorax 1983; 38:212-215
Sackner MA, Greeneltech D, Heiman MS, Epstein S, Atkins N. Diffusing Capacity, Membrane Diffusing Capacity, Capillary Blood Volume, Pulmonary Tissue Volume and Cardiac Output Measured by a re-breathing Technique. Am Rev Resp Dis 1975; 111:157-163
Weingarten JA, Milite F, Lederer DJ, Cohen SJ, Mooney AM, Basner RC. Comparison of single-breath and rebreathe diffusing capacity in Emphysema. Am J Respir Crit Care 2009; 179:A1485
Yilmaz C, Chance WW, Johnson RL, Hsia CCW. Simulation system for a re-breathing technique to measure multiple cardiopulmonary function parameters. Chest 2009; 135:1309-1314

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.