There are a number of simple observations that can be made during a cardio-pulmonary exercise test (CPET) that can point you immediately in a specific diagnostic direction. Recently I was reminded of this while reviewing the CPET results on patient with a complicated medical history whose test had been requested as part of a pre-operative assessment.
Most patients that are candidates for cardio-thoracic surgery do not need to have a CPET and that’s because it is usually straightforward to determine who is high risk and who is low risk from other routine tests. When risk is hard to determine or equivocal, the cardio-thoracic surgeons will order a CPET. They are primarily interested in the VO2 max and Ve-VCO2 slope since there are a number of widely accepted pre-op assessment algorithms that use these values. Even if the CPET results indicate the patient is high risk, the test details can help determine whether there is anything that can be done to improve the patient’s odds.
The patient whose report I was reviewing had moderately severe airway obstruction (FEV1 57% of predicted), mild restriction (TLC 77% of predicted) and a moderate gas exchange defect (DLCO 51% of predicted). This would normally pre-dispose me to look for a pulmonary vascular or pulmonary mechanical exercise limitation but there was a single test value that told me the limitation was going to be cardiovascular instead. That test value was the SaO2 at peak exercise which was 99%.
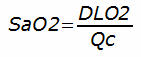
The reason that SaO2 can differentiate between pulmonary and cardiac limitations can be expressed in an equation:
This isn’t a “real” equation, however, and exists only to highlight the relationship between oxygen transfer and cardiac output. Specifically, what it is saying is that as long as the lung’s ability to transfer oxygen is greater than the blood flow rate through the lung, then SaO2 will be normal.
In this particular CPET, despite what the apparent low resting DLCO is saying about gas transfer, cardiac output has to be even lower. It did turn out that the patient had chronotropic incompetence (likely due in part to the beta-blocker medication Metoprolol). The patient also had a mildly reduced O2 pulse.
O2 pulse can be a good indicator of stroke volume. A low O2 pulse is a relatively common occurrence in COPD. Part of this is because individuals with COPD are usually deconditioned. Part can also be because COPD patients often desaturate and when this occurs O2 pulse decreases because of the lower O2 content in arterial blood. In this case, however, there was no desaturation so the low O2 pulse most likely indicates a low stroke volume. The combination of chronotropic incompetence and a low O2 pulse is a pretty strong indication of a low cardiac output in this individual.
I was still bothered by the fact that there was no desaturation during exercise even though the patient’s DLCO was 51% of predicted. After looking the report over carefully I reminded myself that a DLCO measured at rest does not predict a DLCO measured during exercise.
It has long been noted that DLCO increases during exercise. There are several reasons for this. First, an increased cardiac output increases pulmonary capillary blood volume so there is more blood at any one moment that is available for gas transfer. Second, the increased blood flow also means that within the same period more blood is available for gas transfer. Third, and possibly most important, is that ventilation/perfusion mismatching is often a primary reason for reduced DLCO measurements and when cardiac output increases during exercise, under-perfused regions of the lung can see increased blood flow and overall gas transfer can increase dramatically. For any or all of these reasons it is possible that the patient’s resting DLCO was underestimating their true capacity for gas exchange.
Regardless of whether the patient’s “real” DLCO was underestimated, the fact is that their cardiac output was even lower and despite their significant pulmonary disease their primary limitation to exercise was cardiovascular.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.