Spirometry is the most commonly performed (and mis-performed) pulmonary function test around the world. The apparent simplicity of spirometry is misleading since there are numerous subtleties that have a significant effect on the results.
I suspect that when the FVC is thought about it is most often considered to be an index towards the total capacity of the lung. That’s certainly true in it’s own way, but the FVC is actually a critically important factor when determining airway obstruction. I’ve had a number of reports across my desk lately where the patient had a reasonably large change in FVC when compared to their last visit but little change in FEV1, and this has made a difference in how the results are interpreted. For example:
| Visit 1: | Observed: | %Predicted: | Predicted: |
| FVC: | 4.27 | 87% | 4.91 |
| FEV1: | 3.36 | 84% | 3.99 |
| FEV1/FVC: | 79 | 96% | 82 |
| Visit 2: | Observed: | %Predicted: | Predicted: |
| FVC: | 4.67 | 95% | 4.91 |
| FEV1: | 3.38 | 85% | 3.99 |
| FEV1/FVC: | 72 | 88% | 82 |
Although the change in FVC is not significant by my lab’s standards (+0.40 L, +9%) and the FEV1 has hardly changed at all, the FEV1/FVC ratio has gone from being within normal limits to being under the LLN and therefore showing mild airway obstruction.
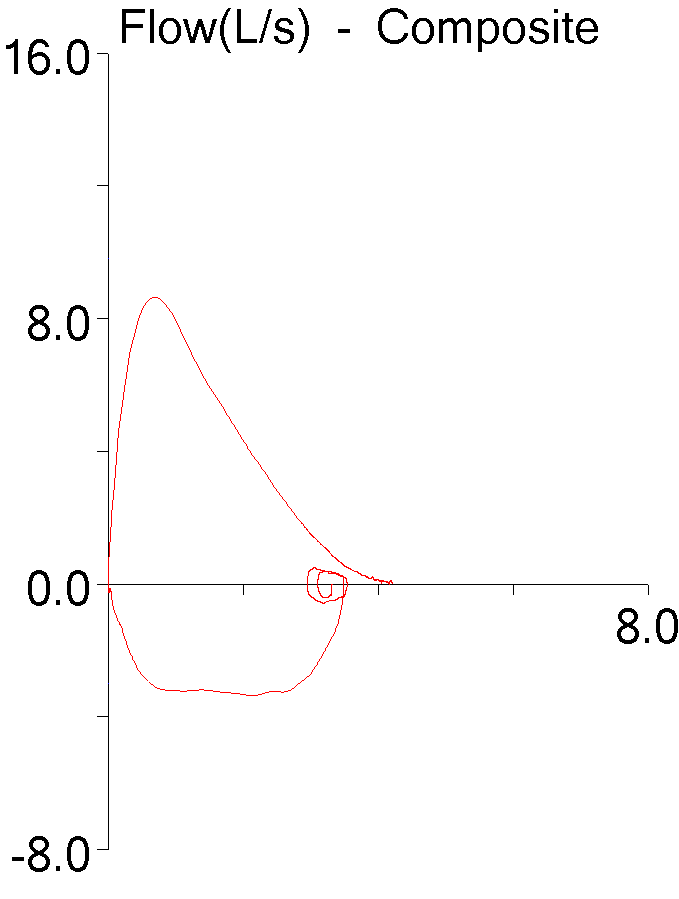
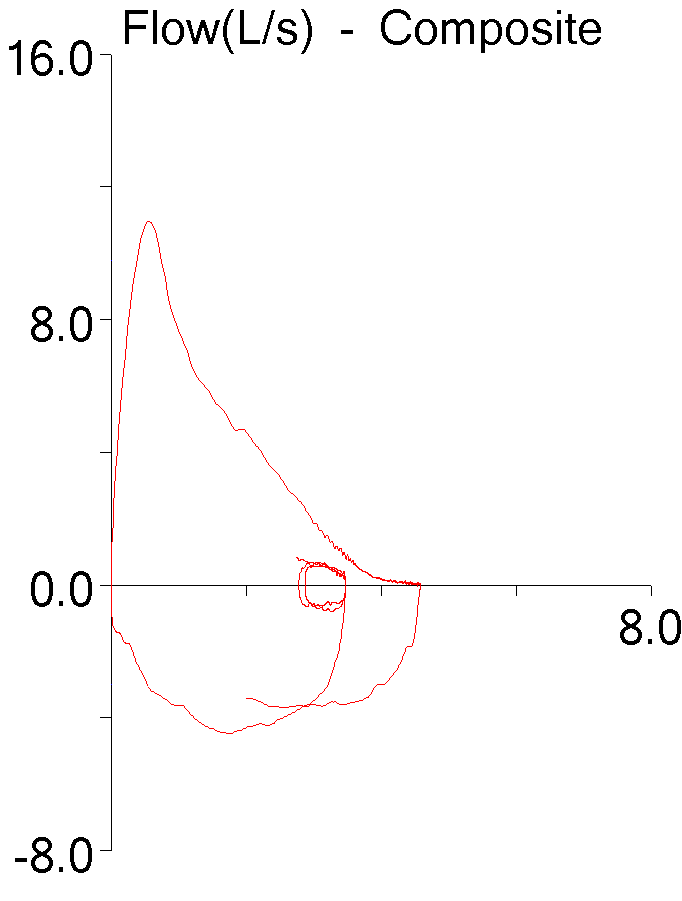
If just the flow-volume loops from each set of results was considered, there is no reason to suspect that either effort was inadequate.
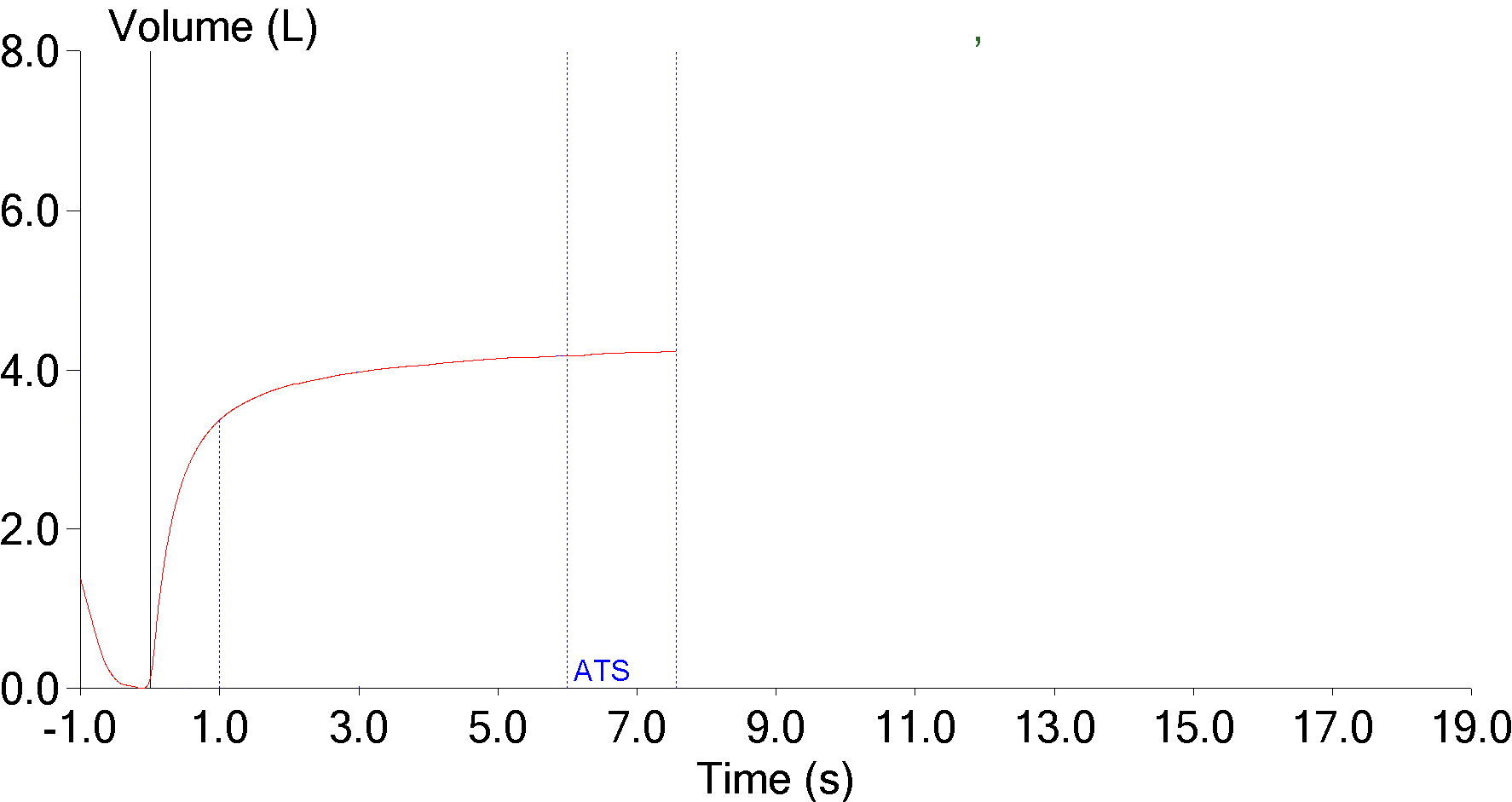
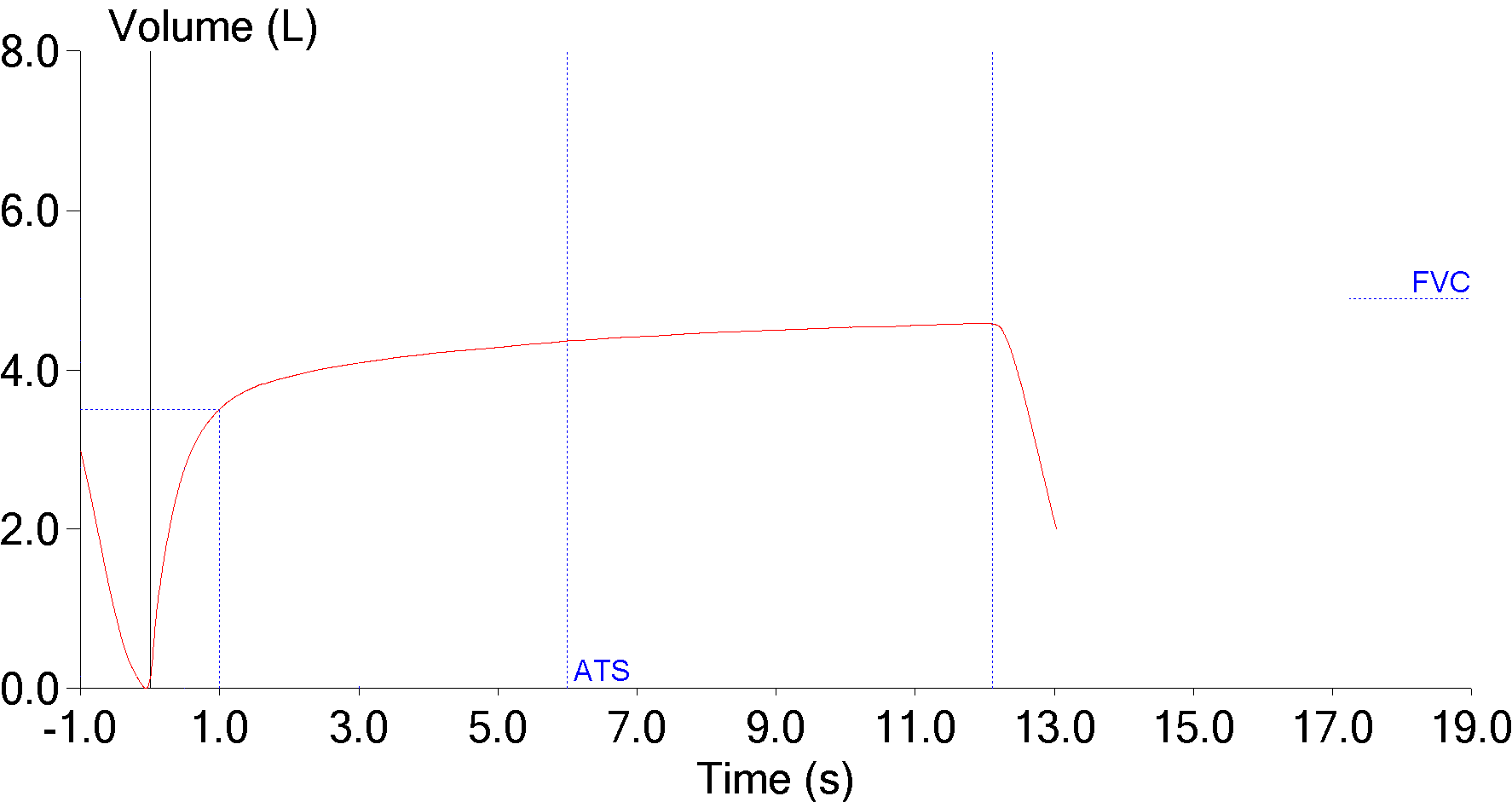
The real difference is in how long the patient exhaled.
The ATS/ERS standard on spirometry testing has a number of things to say about how long the forced vital capacity effort should last.
“It is important for subjects to be verbally encouraged to continue to exhale the air at the end of the manoeuvre to obtain optimal effort…”
Having said that, one of the end-of-test criteria is:
“The volume–time curve shows no change in volume (0.025 L) for ≥1 s(econds), and the subject has tried to exhale for ≥3 s(econds) in children aged <10 yrs and for ≥6 s(econds) in subjects aged >10 yrs.”
It also says that:
“For patients with airways obstruction or older subjects, exhalation times of >6 s(econds) are frequently needed.”
But this is tempered with:
“Although subjects should be encouraged to achieve their maximal effort, they should be allowed to terminate the manoeuvre on their own at any time, especially if they are experiencing discomfort.”
I’ve visited a number of pulmonary function labs and clinics where spirometry was being performed and have seen a wide range in attitudes towards obtaining an “optimal” FVC. What I’ve most often seen is that an “optimal” FVC effort is one of those things where an experienced technician can make all the difference in the world. It takes practice to know how to “read” a patient in order to encourage their maximal effort and to know when to stop pushing them. In addition it takes a certain lack of self-consciousness (I forget which book I read this in but the instructions for technicians performing spirometry included something like “you should be embarrassed by level of clamor you make”). Most importantly though, it also takes a certain level of ruthlessness.
Even more importantly however, what I’ve seen among all levels of individuals that perform and review spirometry is a frequent lack of appreciation for the effect that FVC has on the FEV1/FVC ratio. Everyone understands FEV1 (and yes, many of the physicians and researchers I’ve known and respected have rightly said it’s all about the FEV1) but the first step towards determining the presence of airway obstruction is the FEV1/FVC ratio and there the FVC is just as important as the FEV1.
Taken individually both spirometry efforts met all of the ATS/ERS criteria for adequacy and this is one of the problems with the FVC. The order in which these kind of changes in FVC occur are always different and I’m often left wondering what the reason was. Does a decrease (or increase) in FVC actually reflect a change in the patient’s condition? Or was it more of a change in their mood? Or a change in which technician performed the test?
Currently my lab’s criteria for assessing changes in spirometry trends involve only the FEV1 and FVC individually, and not the FEV1/FVC ratio. I’m not sure this is correct but my thoughts on this keep changing depending on circumstances. Changes in the FEV1/FVC ratio are probably significant when the FVC efforts are comparable, such as when the expiratory time is essentially the same, but maybe not so much when the expiratory times are different. But for many COPD the differences in a patient’s expiratory time (and FVC) are often a better reflection of how well they are doing than the changes in their FEV1. And for many patients with pulmonary fibrosis, the expiratory time (even when it’s suboptimal) doesn’t affect FVC all that much. For a test as apparently simple as spirometry there is probably no simple answer to this problem.
FVC frequently matters as much as the FEV1 when it comes to assessing the presence of airway obstruction. Obtaining an “optimal” FVC remains as much an art as a science, however, and for this reason I suspect that mild airway obstruction is under-diagnosed. There is a lot of leeway in the ATS/ERS criteria for assessing the adequacy of the FVC but other than mandating an exhalation time longer than 6 seconds (10 seconds? 12 seconds? 15 seconds) which is not needed in the majority of patients, it’s unclear to me how they can be improved, particularly since this is an area where the experience of the participants (both patient and technician) often make the most difference.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of lung function testing. Standardisation of spirometry. Eur Respir J 2005; 26: 319-338.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License