I always like it when a patient does something during a test that makes me have to think about the basics of the test and what effect an error will have on the results. I was reviewing a report that had come across my desk and the technician performing the test had put “poor DLCO test reproducibility, fair quality in selected test” in the notes so of course I had to pull up the raw test data and take a look for myself.
The patient had performed three DLCO tests, two of which were completely unusable and one that was sort of okay but not really. Interestingly, the test system software thought it met the criteria for acceptability.
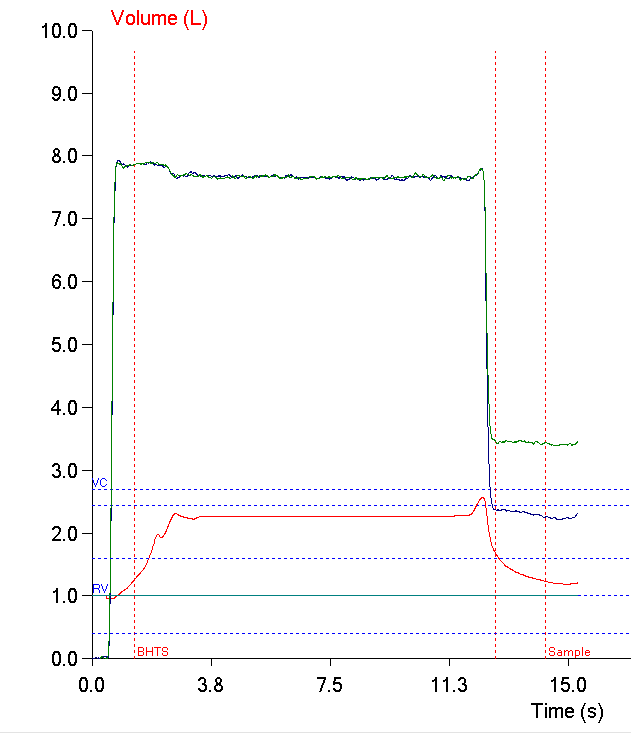
The ATS/ERS statement on DLCO testing says that the inspired volume needs to be at least 85% of the patient’s largest known vital capacity. Even though the patient’s inspired volume during most of the test was well below this threshold they made a further inspiratory effort just before exhaling and exceeded the threshold when they did. For this reason the software thought the effort was acceptable. This points out limitations in our testing system software, its hardware, and in the ATS/ERS statement as well.
When you read the ATS/ERS statement on DLCO testing it is clearly assumed that a patient will hold their breath at their maximum inspired volume throughout the test but I have been unable to find anything in the statement that actually says this. There is a great deal of discussion on the minimum parameters for the inspiratory maneuver, the breath-holding period and the expiration and we all “know” that the patient should do nothing but hold their breath until it comes time to exhale but this isn’t explicitly stated. This isn’t something that really needs to be spelled out for those of us who have spent any time performing DLCO tests but there are programmers and engineers who have no real familiarity with pulmonary function testing that rely on the ATS/ERS statements when they are designing software and hardware. If it isn’t in the statement, it doesn’t get put into the software (and sometimes even when it is in the statement it still doesn’t get put there).
Even so, everybody “knows” that a patient is supposed to reach their maximum lung volume at the beginning of the DLCO test and then hold it at that level during the remaining part of the test but it probably never occurred to anybody to test this assumption. I have to be honest and say I would have assumed that all patients did this or if they didn’t it was because they leaked air out instead. In this case it seems the programmers did not design the software to make sure that the maximum inspired volume was held throughout the breath-holding period but instead to only see if it occurred at any time during the breath-holding period, even if that was only for a fraction of a second.
Strictly speaking, the test system hardware should also help insure the patient holds their breath at the same volume through the test. Our test systems have a valve controlled by the technician that can be locked after a patient has inhaled at the beginning of the DLCO test. In our older volume-based test systems this locking valve prevents the patient from both inhaling and exhaling. Our newest systems however, use a demand valve to provide the DLCO gas mixture to the patient and the inlet for this is located on the patient side of the locking valve. A patient can’t exhale into the demand valve, so the locking valve still prevents the patient from exhaling, but it certainly doesn’t prevent them from inhaling from the demand valve.
This also presumes the technician actually closes the valve during the test and this isn’t always the case. Despite the fact that locking the valve only requires a single press of the [space bar] I’ve seen technicians who seem to think it is better (more fun?) to exhort the patient to hold their breath by themselves without any help. I think that patients need all the help they can get and that you are likely to get better test quality by closing the valve during test and this is the lab’s policy as well, but this doesn’t seem to stop some technicians from doing it the other way.
Normally I’d reject this DLCO test because it has a suboptimal inspired volume but this was the best the patient was able to perform so we needed to try to salvage it. So the question is what effect does this late, extra inspiratory effort have on the test results?
It was unlikely the patient’s lung was at its maximum surface area throughout most of the test. The most common error I see patients make with the DLCO test is to not exhale to RV before they inhale to TLC. This means their inspired volume is really equivalent to an inspiratory capacity not a vital capacity but it doesn’t necessarily mean they aren’t at TLC when they breath-hold. In this case however, when I used a ruler function on the graph I found that the average inspiratory volume was 21% less than the peak inspiratory volume. Even if you assume the peak inspiratory effort was at TLC, during most of the test the maximum lung volume was therefore below the 85% threshold and for this reason, the DLCO is probably underestimated.
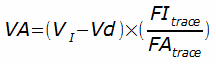
On the other hand, the inspired volume is also used to calculate the alveolar volume (VA):
Where:
VI = Inspired volume
Vd = Dead space volume
FItrace = Inspired trace gas cocentration (helium or methane)
FAtrace = Exhaled trace gas concentration
In this case, the peak inspired volume occurred for only fraction of a second. This time period is probably too short to allow the DLCO gas mixture to re-distribute itself in any meaningful manner so the inspired volume is actually overestimated. This means that the VA is also overestimated. The DLCO calculation is largely a function of K, which is the rate of disappearance of carbon monoxide from the lung, and VA. Since K is a function of the inhaled and exhaled gas concentrations, this means that DLCO scales with VA, and that the patient’s DLCO was likely overestimated because the VA was overestimated.
The patient’s DLCO was probably underestimated because their lung’s surface was reduced through most of the test but at the same time it was probably overestimated because the alveolar volume was overestimated. Do these cancel each other out? In a real sense they can’t because trying to do this would be like adding apples and subtracting oranges but it does make it a touch more likely the results are not as inaccurate as would be expected. We ended up reporting the DLCO with the notation that it had suboptimal quality. It turns out the patient had a DLCO test with acceptable quality about a half a year ago and the present results were not significantly different but this too is not a reason by itself to report suboptimal results.
This was a suboptimal DLCO test and if there had been any alternative it would not have been reported. You often have to work with whatever a patient is capable of doing however and then it becomes important to have a good understanding of the tests so you can try to determine what effect their testing error has on the results. The most interesting thing about this test was that it pointed out a hole in the assumptions a lot of us have about breath-holding during the DLCO test.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standisation of Lung Function Testing. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 2005; 26: 720-735.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.