Sooner or later we all get lucky and find ourselves able to replace older equipment. When you have equipment that’s so old it can’t be repaired (either because the manufacturer no longer supports it or because the manufacturer no longer exists), you’d think this would be a no-brainer but money is always in short supply. I’ve often had to try to keep equipment running long past its expected life time and was only allowed to replace it when it finally broke beyond all hope of repair.
One of the reasons to perform biological QC is so that you can recognize changes in the equipment that don’t appear during a calibration. It also a useful (and recommended) way to assess new test equipment. So what happens when you finally get that new test system and your results are substantially different from what they were before?
I was recently contacted by the manager of an employee health service that had replaced their 18 year old spirometer with a brand-new one. When using their new spirometer they had found their biological QC results coming out noticeably lower (-9%) than they had gotten from their old spirometer and I was asked if I could help them determine why.
My first question was whether or not they were using the same 3 liter syringe to calibrate the different spirometers. Once I found out this was the case I then asked them to use the 3 liter syringe in test mode. The results from this were actually very informative. The old spirometer showed an average FVC of 3.24 liters and the new spirometer showed an average FVC of 3.06 liters.
Both spirometers were flow-based systems although the older one used a pneumotach and the newer one used an ultrasonic sensor. I did not expect the FVC for either spirometer to be exactly 3 liters and this is because the spirometer software always performs a temperature correction on the results. The results showed that the older spirometer was applying a correction factor of 1.08 and the newer spirometer was using 1.02 which is approximately a 6% difference.
Spirometer results need to be corrected for temperature because exhaled air cools as it leaves the body and when it does it contracts. This fact was recognized quite early and Hutchinison’s 1846 spirometer included a thermometer for this reason. The early correction factors were actually too simplistic since they didn’t take into account how much water vapor contributed to the change in volume. This wasn’t recognized until about half a century later and the formula for BTPS derived. Specifically:
where:
VATP = volume at ambient temperature and pressure
PB = barometric pressure
PH2O = partial pressure of water vapor
t = spirometer temperature
37 = body temperature
PH20 in turn can be estimated from:
This worked well when spirometers were all volume-displacement water-seal types with a lot of thermal mass and when all that was measured was the vital capacity (remember, the FEV1 didn’t exist before 1950). Even so, with repeated spirometry efforts spirometer temperature has been shown to increase up to 4 degrees C, which means the temperature of the spirometer itself needs to be monitored, not just room temperature.
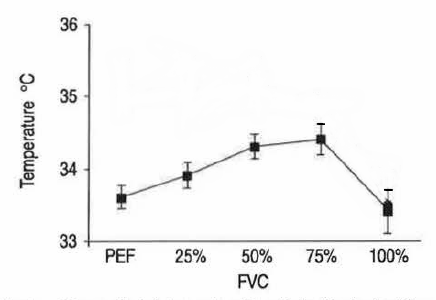
Temperature correction for flow sensors is much more complicated. This is partly because they tend to have a lot less thermal mass, but also because exhaled air flows through them relatively rapidly and doesn’t have much time to be as affected by their temperature. Like a volume-displacement spirometer however, a flow-sensor’s temperature rises with repeated spirometry efforts and this can affect results if it is not corrected for. Exhaled air temperature however, also changes throughout exhalation so a single correction factor is actually too simplistic.
Measuring air temperature during exhalation (dynamic correction) would seem to be a good idea but is actually quite difficult. In particular the thermal mass and response time of a temperature sensor needs to be carefully characterized and these factors change over time. For this reason, there are almost no flow-based spirometry systems that are capable of measuring exhaled air temperature and most manufacturers make assumptions about it instead.
The ATS/ERS 2005 statement on spirometry does discuss some of the issues involved in BTPS and temperature correction, but it does not present any clear solutions nor are there any precise specifications. This means that temperature correction is left up to the equipment manufacturers.
There isn’t anything necessarily wrong with this, since the manufacturers are the ones who should know their equipment best. The manufacturer of the older spirometer went out of business at least a decade ago however, and any manual that came with that system has long since disappeared, so exactly how temperature correction is applied is unknown. I did some digging on the website for the manufacturer of the new spirometer and found that a correction factor of 1.02 is applied to exhaled air regardless of room temperature or sensor temperature. This may be more or less correct but it also seems to be an overly simple response to a complex problem.
So what, if anything, can be done about the discrepancy in spirometry results from the two systems?
About two-thirds of the difference appears to be associated with the difference in temperature correction factors. This is hard-wired into each system’s software and cannot be adjusted. Even if it was possible to adjust the temperature correction factor for the new spirometer to match the old spirometer this isn’t the right way to fix the problem. And that’s only if you assume it actually is a problem. It is a problem in the sense that new results don’t match old results, but it’s also possible that the newer results are more accurate and if that’s the case, it isn’t a problem.
The remaining difference (~3%) is within ATS/ERS specifications. The older spirometer was manufactured in 1997 and uses a pneumotach. Pneumotachs are well understood and characterized but that’s not the same as saying they are 100% accurate. Pneumotachs rely on analog circuitry which is subject to drift and the flow signal needs to be corrected in software for alinearity. Ultrasonic flow sensors are primarily a digital technology and, theoretically at least, are less likely to drift and more likely to be linear across a wide range of flows. Other than that it isn’t possible to say which of the two systems is more accurate.
Since temperature correction can have a significant effect on test results one interesting question this brings up is how temperature correction was applied in the studies that generate the reference equations we use. Most labs that I know use the NHANESIII spirometry reference equations. When I went to the original research paper (Hankinson et al, 1999) I found that the specifications for the volume-displacement spirometry systems used in the study were located in an earlier paper (Hankinson et al, 1991). Neither paper however, explained how temperature correction had been performed other than to state that spirometry was performed according to the 1994 ATS standards. The language in the ATS 1994 statement on spirometry regarding BTPS correction is essentially identical to the 2005 ATS/ERS statement, and other than saying that temperature correction is a good idea, there are no requirements or specifications. The earlier paper (Hankinson et al, 1991) also stated that the spirometers had been “independently tested” and referred to another research paper (Nelson et al, 1990) but that article specifically stated that BTPS correction was not tested.
So was the NHANESIII spirometry data corrected for BTPS? Probably yes, but exactly how temperature was measured and how a temperature correction was applied is not clear in any way. Does this mean the NHANESIII reference equations are inaccurate? Probably not, or at least not any more than any other set of reference equations, but I will admit I have some reservations about them I didn’t have before.
The effect that temperature has on measuring exhaled volume has been known and understood for a long time, but applying it is both technically difficult and inconsistently performed. Since an error in measuring (or estimating) spirometer temperature of 1 degree centigrade causes an error of approximately 0.5% in measured volume it is easy to say that the ATS/ERS spirometry standard should be more precise about how temperature correction should be performed. Given our limited understanding (after all this time!) of the temperature characteristics of flow sensors and volume-displacement spirometers this isn’t realistic. Even if the equipment side of temperature correction was better understood the BTPS calculation assumes that patient body temperature is 37 degrees centigrade; that inhaled air has been warmed to that temperature before being exhaled; and that exhaled air is a consistent temperature. These assumptions are usually not true and this means that temperature factors will always cause a certain amount of error in our test results and that both the amount and direction of this error is unknown.
Over the years I’ve gone through numerous changes in equipment and reference equations. Each time this has occurred there has been a discontinuity (sometimes small, sometimes large) between newer and older test results. There is no easy way to reconcile these differences and usually the best you can do is to keep moving forward and put them behind you. I’d like to think that we improve every time this happens and to some extent I suppose we do, but when I dig into basic problems like temperature correction all too often I find that not much has really changed.
Kudos to the manager of the employee health service that contacted me for doing the QC, paying attention to the results and for worrying about them.
References:
American Thoracic Society. Standardization of spirometry. 1994 Update. Am J Resp Crit Care Med 1995; 152: 1107-1136.
Brusasco V, Crapo R, Viegi G. ATS/ERS task force: Standardisation of lung function testing. Standarisation of spirometry. Eur Respir J 2005; 26: 319-338.
Cotes JE, Leathart GL. Lung Function. Assessment and application in medicine. 6Th Edition. Blackwell Scientific Publications, 1993.
Gilliland FD, Linn W, Rappaport E, Avol E, Gong H, Peters J. Effect of spirometer temperature on FEV1 in a longitudinal epidemiological study. Occup Environ Med 1999; 56: 718-720.
Hankinson JL, Viola JO. Dynamic BTPS correction for spirometric data. J Appl Physiol 1983; 55(4): 1354-1360.
Hankinson JL, Bang KM. Acceptability and reproducibility criteria of the American Thoracic Society as observed in a sample of the general population. Am Rev Resp Dis 1991; 143: 516-521.
Hankinson JL, Viola JO, Petsonk EL, Ebeling TR. BTPS correction for ceramic flow sensor. Chest 1994; 105(5): 1481-1486.
Hankinson JL, Odencrantz JR, Fedan KL. Spirometric reference values from a sample of the the general U.S. population. Am J Respir Crit Care Med 1999; 159: 179-187.
Johnson LR, Enright, PL, Voelker HT, Tashkin DP. Volume spirometers need automated internal temperature sensors. Am J Respir Crit Care Med 1994; 150: 1575-1580.
Linn WS, Solomon JC, Gong H, Avol EL, Peters JM. Temperature standardization of multiple spirometers. J Occup Environ Med 1998; 40: 148-152
Madan I, Bright P, Miller MR. Expired air temperature at the mouth during a maximal forced expiratory maneuver. Eur Respir J 1993; 6: 1556-1562.
Nelson SB, Gardner RM, Crapo RO, Jensen RL. Performance of contemporary spirometers. Chest 1990; 97: 288-297.
Zawadski DK, Lenner KA, McFadden Jr. ER. Comparison of intraairway temperatures in normal ans asthmatic subjectes after hyperpnea with hot, cold and ambient air. Am Rev Resp Dis 1988; 138: 1553-1558.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License