There have been numerous criticisms of the single-breath DLCO technique, many of them quite valid. In particular, the standard equation for calculating DLCO makes no consideration for the inspiratory and expiratory phases of the maneuver when lung volume and the alveolar capillary surface area are changing. Some investigators have devised ways of correcting for inhalation and exhalation, however other investigators have sidestepped the issue entirely by showing that DLCO can instead be calculated from information acquired only during exhalation.
During exhalation, once the gas that exits the lung leaves the alveoli, diffusion ceases. Gas that exits the lung during the early part of exhalation will have had less time for CO to diffuse from the alveoli into the pulmonary capillaries and will have a higher concentration of carbon monoxide than will gas that exits later. Exhaled gas can therefore be considered to consist of a continuous set of alveolar gas samples, separated by time and the differences between these “samples” can be used to calculate DLCO.
Several techniques have been developed to calculate DLCOexh. What these techniques have in common is that they all use a relatively standard single-breath DLCO gas mixtures in conjunction with fast responding carbon monoxide and helium or methane gas analyzers. They also require the subject exhale slowly (approximately 0.5 L/sec) after inhaling the DLCO gas mixture to TLC. The primary differences between these techniques lies in the way DLCOexh is calculated.
DLCOexh – Point Sample Technique:
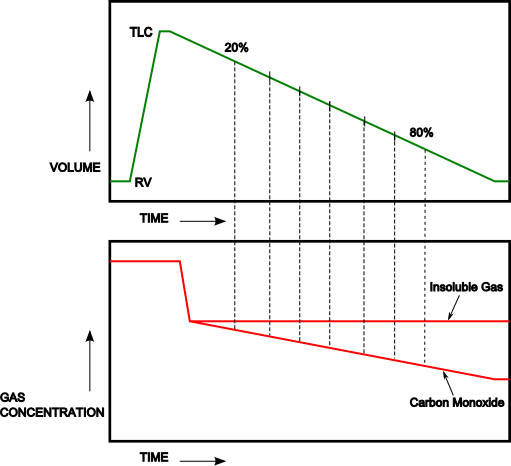
In the study of Newth et al [9] the carbon monoxide and helium gas concentrations were determined for the midpoint of each 10% decrement in lung volume from 20% to 80% of the subjects exhaled volume.
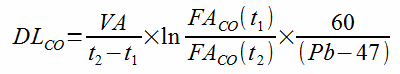
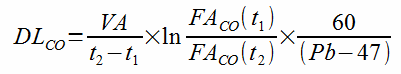
For each interval DLCOexh was then calculated from:
where:
t1 = time at start of 10% interval
t2 = time at end of 10% interval
FACO(t1) = CO concentration at start of 10% interval
FACO(t2) = CO concentration at end of 10% interval
and:
where:
VI = inspired volume, ml
Vd = dead space (machine + anatomic), ml
FIHe = initial concentration of helium
FexhHe(50%) = concentration of helium at 50% of exhalation
Volexh = volume exhaled from peak inhalation at midpoint of interval
Newth’s study showed that in normal subjects DLCOexh did not change when preceded by different inspiratory flow rates and different breath-hold periods. DLCOexh was, however, constant at all lung volumes only during slow exhalations.
DLCOexh – Discrete Sample Technique:
In an analysis of the point-sample technique, Graham et al [3] showed that a 1 percent error in the measurement of carbon monoxide could lead to an 8 to 14 percent error in DLCOexh. In light of this they took two approaches towards increasing the accuracy of the DLCOexh calculation.
First, gas concentrations were averaged over larger intervals. After deadspace clearance, the subject’s digitally recorded exhaled volume was divided into both two and three equal intervals. This made the filtering of the exhaled gas concentration signals unnecessary. The average carbon monoxide and methane gas concentrations for each of these intervals were then used to calculate a series of DLCOexh values.
Second, they used an iterative procedure for calculating DLCOexh that depends on comparing the ratios of exhaled gas concentrations rather than on the absolute values of the exhaled gas concentrations. A complicated and computationally intensive approach highly suited to computerized analysis, this algorithm starts by first predicting the gas concentration ratios of two gas samples based on an assumed DLCOexh value, which during the first iterative cycle is usually the subject’s predicted DLCOSB. This predicted ratio is compared to the actual ratio and a new DLCOexh value is calculated. This process is repeated until the difference between the new and old DLCOexh values is less than an 0.01 percent, which usually takes about 20 iterations to achieve.
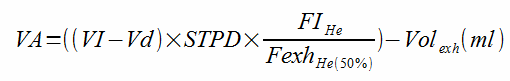
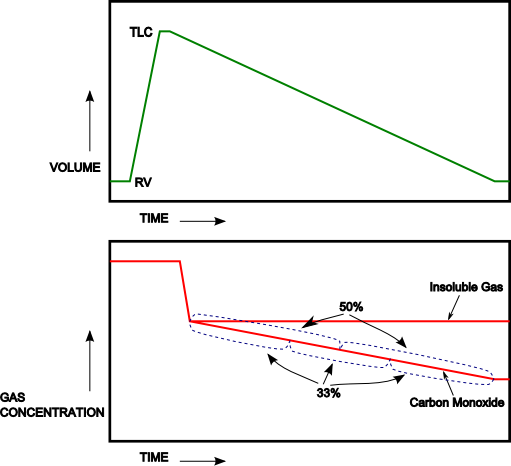
Intrabreath DLCO (Log Slope) Technique:
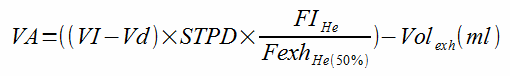
An alternate approach first proposed by Martonen and Wilson [8], the natural logarithm of exhaled carbon monoxide and of alveolar volume are used to calculate DLCOexh. After exhaling to RV, subjects inhale the DLCO gas mixture to TLC. After breath-holding for approximately 1 to 2 seconds, the subjects exhale slowly at a constant rate (0.3 to 0.6 L/sec). Gas concentrations measured between 20% and 80% of the exhaled volume are used to calculate DLCOexh as follows:
Where:
Ve = exhaled flow rate in liters/second
FACO = Fractional concentration of CO
FACO0 = Fractional concentration of CO at end-inspiration
VA = Alveolar volume in liters
VA0 = Alveolar volume in liters at end-inspiration
And:
Where:
Vi = inspired volume
FiCH4 = Fractional concentration of inhaled methane
FeCH4 = Fractional concentration of exhaled methane
Vexh = Volume exhaled from end-inspiration
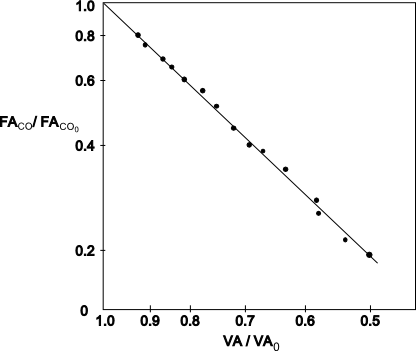
The slope of the relationship of ln FACO/FACO0 vs ln VA/VA0 is analyzed through least squares regression analysis and uses data from the beginning of dead space washout to closing volume.
A possible advantage of this technique compared to the other more discrete techniques is that essentially the entire exhaled gas stream is used to calculate DLCO although most investigators have excluded data after closing volume has been achieved.
Comparing Single-breath DLCO with DLCOexh:
Comparable values between single-breath DLCO and DLCOexh results have been shown in groups of patients with normal lungs, patients with obstructive lung disease and patients with severe congestive heart failure pre- and post-heart transplant. A closer inspection however, of the scattergrams presented in Wilson’s [13], Quantz’s [10] and Huang’s data [4], however, shows that some individuals had significant differences in results between the two techniques and the reasons for this have not been studied.
One of the most serious criticisms of the DLCOexh technique is that it assumes that the lung fills and empties homogeneously and that the rate of diffusion remains constant over a wide range of lung volumes. Both of these assumptions have been shown to be incorrect by numerous investigators. The same criticism can be leveled at the single-breath technique, but the effect that heterogeneous filling and emptying has differs between the two approaches and this has not been studied other than to compare averaged results.
Newth [9] stated that DLCO did not change as lung volume decreased in patients with normal lungs and this finding is seconded to some degree by Cotton [1], however other researchers [3][5][11][7] have shown that DLCOexh does change, with the most common finding to be an elevated value near TLC and reduced value near RV. This leaves open to question about which lung volume DLCOexh is “most” correct and should be the reported value.
Additionally, alveolar volume (VA) remains a significant component of the DLCOexh calculation and how this is derived differs between specific DLCOexh techniques. When the method used to calculate VA was reported investigators measured either the methane or helium gas concentration at 50% of the exhaled vital capacity [11][12], or from the methane or helium gas concentration at the beginning of exhalation [13][7][2] whereas other studies [5][4] only stated that expired methane was used to calculate VA without saying whether this value was obtained at the beginning or middle of exhalation, or was a mixed-expired value.
Wilson [13] noted that VA was smaller and DLCO/VA higher when using the log slope technique when compared to DLCOSB. This difference was attributed to the fact that the longer breath-hold period of the DLCOSB technique allows for a more complete distribution of methane. Other researchers however, have reported higher VA results from the log slope technique than from the DLCOSB technique and noted that these VA measurements were closer to the TLC measured by plethysmography [6] and by nitrogen washout [10] than the DLCOSB VA. The reason for these discrepancies in reported VA has not been determined.
Finally, a steady expiratory flow rate is necessary for the accuracy of the exhaled DLCO calculations. Where reported several studies have used visual feedback and/or a flow restrictor to enable the patient to do this. The expiratory flow rate of 0.5 L/sec appears to have been empirically chosen by Newth [9] because results at this flow rate were reproducible whereas results from a higher flow rate of 2.0 L/sec were not. Subsequent studies have used this target value but where reported subjects have exhaled anywhere between 0.23 and 1.00 L/sec and the effect of these different expiratory flow rates has not been studied.
Proponents of the DLCOexh technique say that it allows DLCO to be measured during exercise but there are only a small number of studies of DLCOexh during exercise and the actual details of how DLCOexh was performed in these circumstances have been limited. This makes it difficult to assess whether DLCOexh is better or even as valid as other exercise DLCO measurement techniques. As importantly, the fact that expiratory flow must be limited to measure DLCOexh limits its usefulness during exercise, particular in comparison with rebreathing DLCO techniques that do not place any significant constraints on the subject’s breathing pattern.
Overall, the exhaled DLCO technique is an interesting approach to measuring DLCO that appears to be able to show results that are comparable to single-breath DLCO. Although it is potentially useful in some patients who have difficulty with the single-breath DLCO maneuver its clinical relevance is hampered by a lack of standardization and the fact that differences in specific individual’s results when compared to the single-breath DLCO have not been explained.
REFERENCES:
[1] Cotton DJ, Newth CJL, Portner PM, Nadel JA. Measurement of single-breath CO diffusing capacity by continuous rapid CO analysis in man. J Appl Physiol 1979; 46:1149-1156
[2] Felton C, Rose GL, Cassidy SS, Johnson RL. Comparison of Lung Diffusing Capacity during Rebreathing and During Slow Exhalation. Resp Physiol 1981; 43:13-22
[3] Graham BL,Mink JT, Cotton DJ. Dynamic measurements of CO diffusing capacity using discrete samples of alveolar gas. J Appl Physiol 1983; 54:73-79
[4] Huang YC, Helms MJ, MacIntyre NR. Normal values for single exhalation diffusing capacity and pulmonary capillary blood flow in the sitting, supine positions and during mild exercise. Chest 1994; 105:501-508
[5] Huang YCT, O’Brien SR, MacIntyre NR. Intrabreath Diffusing Capacity of the Lung in Healthy Individuals at Rest and During Exercise. Chest 2002; 122:177-185
[6] Kiss D, Popp W, Wagner C, Havelec L, Sertl K. Comparison of the single breath with the intrabreath method for the measurement of the carbon monoxide transfer factor in subjects with and without airways obstruction. Thorax 1995; 50:902-905
[7] MacIntyre NR, Nadel JA. Regional Diffusing Capacity in Normal Lungs during a Slow Exhalation. J Appl Physol 1986; 52:1487-1492
[8] Martonen TB, Wilson AF. Theoretical Basis of single-breath gas absorption tests. J Math Biol 1982; 14:203-220
[9] Newth CJL, Cotton DJ, Nadel JA. Pulmonary Diffusing Capacity Measured at Multiple Intervals During a Single Exhalation in Man. J Appl Phys 1977; 43:617-625
[10] Quantz M, Wilson S, Smith C, Stitt L, Novick R, Ahmad D. Advantages of the Intrabreath Technique as a Measure of Lung Function Before and After Heart Transplantation. Chest 2003; 124:1658-1662
[11] Ramage JE, Coleman RE, MacIntyre NR. Rest and exercise cardiac output and diffusing capacity assessed by a single exhalation of methane, acetylene and carbon monoxide. Chest 1987; 92:44-50
[12] Stokes DL, MacIntyre NR, Nadel JA. Nonlinear increases in diffusing capacity during exercise by seated and supine subjects. J Appl Physiol 1981; 51:858-863
[13] Wilson AF, Hearne J, Brenner M, Alfonso R. Measurement of Transfer Factor during Constant Exhalation. Thorax 1994; 49:1121-1126

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

Questions –
1. Can DLCO by intra breath method be done on patients with vital capacity less than 1 L ?
2. Which are the PFT systems offering DLCO intra breath method ?
Neeraj –
1) Theoretically, yes, but I think it depends a lot on why the VC is so low. If it was a restrictive defect, then there is at least some probability that the diffusion gas mixture was distributed relatively homogeneously and the results would apply to the lung as a whole. If it was a severe obstructive defect, then the gas mixture was probably inhomogeneously distributed and the results would be questionable.
2) Carefusion (aka Sensormedics, aka Viasys, aka Vyaire) did offer an intrabreath DLCO option on their test systems up until at least 10 or so years ago. I don’t know whether they still do or not.
I have reservations about the accuracy of intrabreath DLCO testing. First, there’s an assumption that the lung fills and empties more or less homogeneously, and that’s just not true. For individuals with reasonably normal lung function this probably doesn’t make a significant difference, but for those with significant ventilation inhomogeneities it likely does. There’s also technical issues with the level of accuracy you can get with real-time multi-gas analyzers when you are continuously sampling exhaled air (resolution and sample size) and in just how VA is calculated.
Finally, there are no reference equations for Intrabreath DLCO results so interpretation is always going to be a bit iffy. The only recent articles on intrabreath DLCO are for measurements made during exercise, and where results are compared across groups.
Regards, Richard