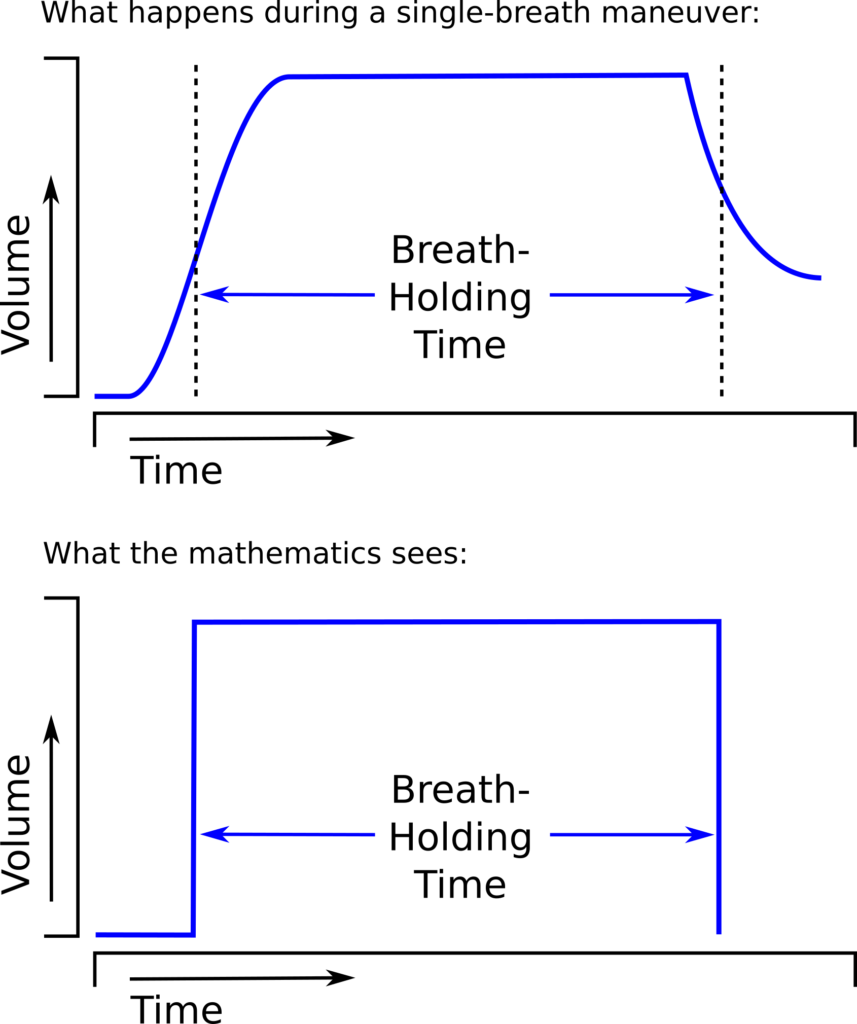
One of the limitations of the single-breath DLCO is that the equation used to calculate results implicitly assumes that the entire breath-holding period occurs at TLC. Mathematically, what happens to the diffusion of carbon monoxide (CO) during inspiration and expiration is not a consideration:
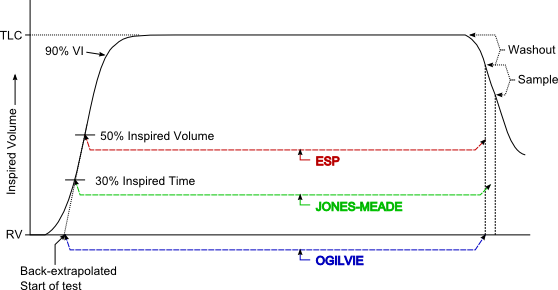
The different approaches towards measuring breath-holding time (BHT) make allowances for inspiration and expiration to one extent or another but realistically they should be considered fudge factors.
The 3-equation DLCO was first proposed by Graham et al in 1980 and it received its name because there is a separate equation for each phase of the single-breath DLCO maneuver. The individual equations are based on the mass-balance equation and attempt to account for the mass of CO inhaled, absorbed and exhaled during the single-breath maneuver. One of the most significant differences is that an iterative approach is used to determine DLCO. Specifically, an initial estimate of DLCO is made and then compared against the values measured during the three phases. Any differences in observed versus expected values is used to re-estimate the DLCO, and then re-compare it. The authors indicated that 10 iterations are usually sufficient to converge on a DLCO value that meets all measured conditions with a high degree of accuracy.
Because the amount of exhaled CO is important the 3-equation method requires that the patient exhale to RV (or at least until the expiratory flow rate equaled the flow rate of the gas analyzer’s sampling line). In addition, the expiratory washout volume was estimated using the Fowler approach towards measuring dead space (which was included for the first time as a recommendation in the 2017 ERS/ATS DLCO standards).
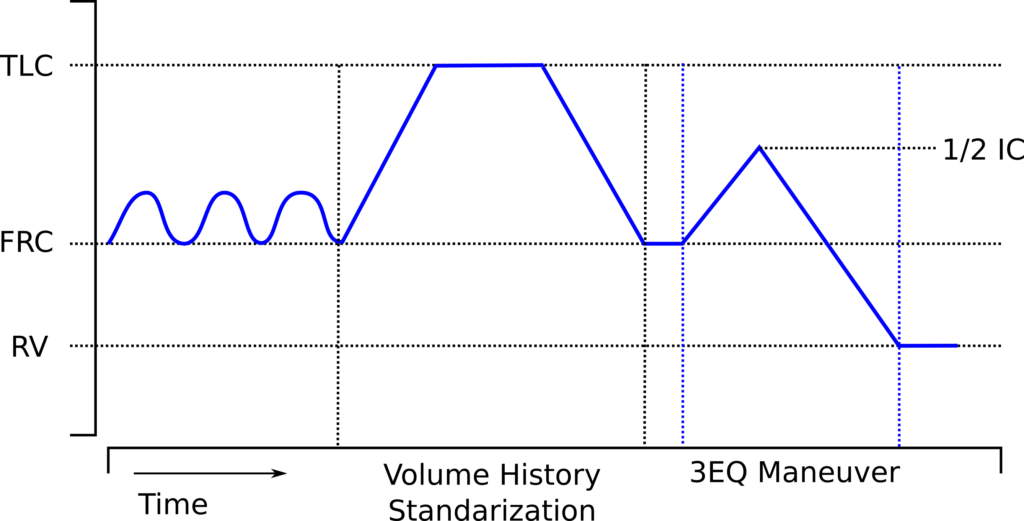
Using the 3-equation method, the authors found that DLCO remained relatively constant over a broad range of inspiratory, breath-holding and expiratory times as well as a variety of inspiratory volumes in normal subjects. Later studies however, indicated that in subjects with ventilation inhomogeneity DLCO decreased when breath-holding time was decreased. It was noted that there was a strong correlation between the phase III slope of the N2 washout curve and the amount of decrease in DLCO that occurred at shorter breath-holding time. For this reason this effect was attributed the fact that the amount of time needed for diffusive gas transport to the alveoli increases as ventilation inhomogeneity increases. Despite this, the authors have continued to advocate that the 3-equation DLCO be performed without a breath-hold period. In addition, they also advocate that the inspiratory phase of the 3-equation maneuver be performed from FRC, not RV, and that the inspired volume be ½ the IC. They state:
“While a VC inhalation minimizes ventilation nonuniformities in the lung and would be easier to standardize in the clinical setting, a submaximal breath from FRC is more sensitive in the detection of peripheral inhomogeneities in the lung…”
Interestingly, one study showed that the 3-equation DLCO was sensitive to volume history. Specifically, the DLCO measured more or less immediately after a deep breath was significantly higher than one performed after a prolonged period of tidal breathing. This was noted in normal subjects when the 3-equation DLCO was performed without a breath-holding period. Possible reasons for this include an increase in surface secondary to re-establishment of the alveolar surfactant, redistribution of capillary blood volume and a transitory change in hematocrit.
Note: No further research appears to have been done of this subject however, and little or no research has been done on the effects of volume history on the traditional single breath DLCO method. Notably the 2017 ERS/ATS DLCO standard says nothing about volume history, so it’s unclear how important this actually is to routine DLCO testing.
Regardless of the cause, the authors have suggested that the 3-equation DLCO always be performed immediately after a deep breath in order to standardize volume history. For this reason a 3-equation maneuver is expected to be performed like this:
Since the 3-equation DLCO seems to be relatively insensitive to inspiratory and expiratory time, and would be easier to perform than the standard DLCO why hasn’t its use become more widespread?
One major reason for this is that a primary assumption of the 3-equation method is that DLCO remains the same regardless of lung volume. There is, however, a large amount of research that indicates that this is not true. Admittedly this is based primarily on the standard single-breath DLCO methodology but even so, the fact that other techniques like rebreathing DLCO and steady-state DLCO which are measured at lung volumes below TLC always produce results that are lower than single-breath DLCO would seem to support this.
Another reason is that there are no reference equations for the 3-equation DLCO. One population study (283 subjects) did compare the 3-equation DLCO (performed with an RV to TLC inspiration) to the standard single-breath DLCO, using the three BHT measurement approaches (Ogilvie, ESP, Jones-Meade). It found that the 3-equation and Jones-Meade were in close agreement in both normal patients and those with restriction or obstruction. However the 3-equation DLCO was not performed as advocated by the original authors so it is unclear how well these results actually compare to those. In addition the 3-equation method has not been formally studied with any lung disorders so interpreting results remains somewhat problematic.
In addition almost all of the research on the 3-equation DLCO has been performed by the same small group of researchers. Rightly or wrongly this may have implied that the technique was not easily transferable. There has been some truth to this in that at the time the majority of this research was performed (1980’s through 1990’s) testing required a mass spectrometer, a fast-responding CO analyzer, and careful attention to gas sample transit time and analyzer response time. This has since changed and the type of equipment needed to perform the 3-equation method has become fairly standard. For this reason some manufacturers have at one time or another offered the ability to perform 3-equation DLCO testing but this is likely too little, too late.
Finally, although I have a great deal of respect for the originators of the 3-equation method, I also have to say that they’ve done a remarkably poor job of making it understandable. Their explanation, such as it is, has always begun (and pretty much ended) with a series of mathematical formula that require an understanding of integrals and calculus. A simpler and more detailed explanation might have gone a long way towards improving acceptance and a more widespread use of the 3-equation DLCO.
The 3-equation DLCO attempts to include the inspiratory and expiratory phases of the single-breath maneuver and thereby overcome one of the conceptual faults of the standard DLCO test. To some extent it succeeds at this but it does so at the cost of assuming that DLCO remains constant regardless of lung volume despite evidence to the contrary. Although it is an interesting technique that could have simplified DLCO testing it never achieved “critical mass” and instead remains a historical footnote.
References:
Beck KC, Offord KP, Scanlon PD. Comparison of four methods for calculating diffusing capacity by the single breath method. Chest 1994; 105(2): 594-600.
Cotton DJ, Taher F, Mink JT, Graham BL. Effect of volume history on changes in DLCO SB-3EQ with lung volume in normal subjects. J Appl Physiol 1992; 73(2): 434-439.
Cotton DJ, Prabhu MB, Mink JT, Graham BL. Effect of ventilation inhomogeneity on DLCO SB 3EW in normal subjects. J Appl Physiol 1992; 73(6): 2623-2630.
Cotton DJ, Mink HT, Graham BL. Nonuniformity of diffusing capacity from small alveolar gas samples is increased in smokers. Can Respir J 1998; 5(2): 101-108.
Graham BL, Dosman JA, Cotton DJ. A theoretical analysis of the single breath diffusing capacity for carbon monoxide. IEEE Trans Biomed Eng 1980;BME-27:221-227.
Graham BL, Mink JT, Cotton DJ. Improving the accuracy and precision of single-breath diffusing capacity measurements. J Appl Physiol 1981; 51(5): 1306-1313.
Graham BL, Mink JT, Cotton DJ. Effect of breath-hold time on DLCO(SB) in patients with airway obstruction. J Appl Physiol 1985; 58(4): 1319-1325.
Graham BL, Mink JT, Cotton DJ. Implementing the three-equation method of measuring single breath carbon monoxide diffusing capacity. Can Respir J 1996; 3(4): 247-257.
Graham BL, Brusasco V, Burgos F, et al. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J 2017; 49: 1600016.
Wand JS, Abboud RT, Wang LM. Effect of lung resection on exercise capacity and carbon monoxide diffusing capacity during exercise. Chest 2006; 129: 863-872

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International Lic

Graham’s 3 equation formula always fascinated me since I found out about it and, with my surprise, noticed that my equipment can calculate it. Unfortunately our CosMed QBox calculate it with the usual maneuver, meaning 10 seconds of breath hold. It’ll be really interesting if manufacturers started to implement more “open” maneuver settings, since in our experience 10 seconds breath old for severely ill patients may be too many, making DLco useless.