When assessing the response to bronchodilators the change in FEV1 is used far more frequently than any other spirometry result. Other values such as inspiratory capacity (IC) and peak inspiratory flow (PIF) have also been proposed as indicators, but the ATS/ERS standards includes changes in FVC as well as changes in FEV1 and this is often overlooked. Specifically they:
“…recommend using the per cent change from baseline and absolute changes in FEV1 and/or FVC in an individual subject to identify a positive bronchodilator response. Values >12% and 200 mL compared with baseline during a single testing session suggest a ‘‘significant’’ bronchodilatation.”
I don’t have any particular disagreement with this since post-BD increases in FVC are probably similar in nature to the post-BD changes in IC seen in some individuals with COPD. So when spirometry results like this:
| Pre-BD: | %Predicted: | Post-BD: | %Change: | |
| FVC: | 1.82 | 66% | 2.55 | +40% |
| FEV1: | 0.66 | 32% | 0.72 | +10% |
| FEV1/FVC: | 37 | 49% | 29 | -22% |
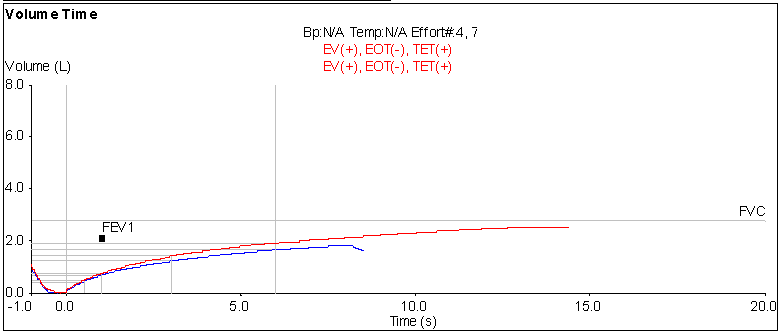
comes across my desk, I’m inclined to consider that the results show a positive bronchodilator response. Post-BD increases in FVC are not usually quite as large as 40% however, so I took a closer look at this particular test. When I did what I saw was that the post-BD test length was significantly longer than the pre-BD test length.
Although FEV1 is often thought of as being a measurement of expiratory flow it is by definition a volume measurement. The time period over which it is measured (i.e., 1 second) is also tightly defined since by default it also includes a definition of how the beginning of exhalation is determined (back-extrapolation). FVC, on the other hand, it much more open-ended. It is simply defined as the maximum amount of air an individual can exhale after a maximal inhalation.
Note: A low FEV1/FVC ratio is one of the primary indicators of airway obstruction but the FEV1/FVC ratio can be falsely elevated when there is a submaximal FVC. This is at least one of the reasons that the FEV6 and the FEV1/FEV6 ratio have been proposed a substitute for the FVC and FEV1/FVC ratio.
The indications for judging an adequate FVC include the end-expiratory flow rate (which is actually defined as no change in volume more than 0.025 L in 1 sec) and that the effort is at least 6 seconds long. In this case both the pre-BD and post-BD spirometry efforts met the 6 second criteria but neither met the end-expiratory flow criteria. Given the very severe airway obstruction seen in the results this is not surprising and judged by themselves either effort would probably have been considered adequate for routine spirometry.
So is the increase in FVC an indication of a positive reponse to a bronchodilator or is it simply from an increase in expiratory time? Conversely, is an increase in expiratory time itself an indication of a positive response to a bronchodilator?
In order to look at this more carefully I downloaded the raw FVC test data from our database (paired flow and volume signals, 200 samples/sec) and compared what the difference would have been if both efforts had the same expiratory time. What I saw was that at 8.25 seconds (the length of the pre-BD effort) the post-BD volume was 2.02 L, which is a 0.20 L increase from the pre-BD effort, but at the same time only an 11% increase. That’s almost significant by the ATS/ERS standards, but not quite. It’s not clear that this is a fair comparison however, since I’ve not seen any study that measured the post-BD expiratory volume that occurred at the same expiratory time as the pre-BD FVC.
A number of studies have shown that subjects with moderate to severe COPD often have a significant increase in FVC following bronchodilator but the role that expiratory time has in this is often undocumented. In those studies where expiratory time was reported it usually increased post-bronchodilator and in at least one study the investigators were able to show that the increase in expiratory time was most likely attributable to the effects of the bronchodilator and not solely to a learning effect. It appears, therefore, that although a post-BD increase in FVC can be explained in part by an increase in expiratory time, that an increase in expiratory time may also be due to the action of the bronchodilator.
All studies that showed an increase in FVC following bronchodilator thought it was likely due to a decrease in gas trapping. Interestingly more one study indicated that an isolated post-BD increase in FVC (i.e. with little or no change in FEV1) is almost solely seen in severe COPD. Although this does not appear to have been specifically addressed results from one study indicate that those individuals with a significant post-BD increase in FVC are also those who have a significant post-BD increases in IC and decreases in FVC.
Since SVC is frequently larger than FVC in patients with airway obstruction an interesting question is that whether individuals that have a significant post-BD increase in FVC show a similar increase in SVC. Another question would be that since FEV6 is used as a substitute for FVC does FEV6 show as significant change as FVC or not?
An additional point concerning SVC is that the ATS/ERS standards suggest calculating the FEV1/VC ratio using the largest VC available regardless of its source (i.e. FVC, SVC or FIVC). I’ve seen a lab with software that automatically substituted the largest VC into the reported results for FVC, SVC and FEV1/FVC without documenting which specific test it was taken from. Since SVC is rarely measured post-bronchodilator this kind of automatic substitution could obscure significant post-BD changes in FVC.
The ATS/ERS standards state that a significant increase in FVC is a sign of bronchodilation but do not explicitly consider the effect that expiratory time has on FVC. Even though there can be a significant post-BD increase in expiratory time and this can be considered to be an effect of the bronchodilator the quality of the pre-BD effort should always be considered as well. When a pre-BD spirometry effort ends abruptly or early, particularly when compared to a better quality post-BD effort then I’d be far more inclined to discount it as a significant improvement.
In this particular case, there was an almost significant increase in FVC when the same expiratory time was considered and certainly a significant increase in expiratory time and FVC overall so I’d have to consider this was a significant response to bronchodilator.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of lung function testing. Standardisation of spirometry. Eur Respir J 2005; 216: 319-338.
Brusasco V, Crapo R, Viegi G. Interpretive strategies for lung function tests. Eur Respir J 2005; 26: 948-968.
Cerveri I, Pellegrino R, Dore R, Corsico A, Fulgoni P, Van de Woestijne KP, Brusasco V. Mechanisms for isolated volume response to a bronchodilator in patients with COPD. J Appl Physiol 2000; 88(6): 1989-1995.
Girard WM, Light RW. Should the FVC be considered in evaluating response to bronchodilator? Chest 1983; 84(1): 87-89.
O’Donnell DE. Assessment of bronchodilator efficacy in symptomatic COPD. Chest 2000; 117: 42S-47S.
O’Donnell DE, Forkert L, Webb KA. Evaluation of bronchodilator responses in patients with “irreversible” emphysema. Eur Respir J 2001; 18: 914-920.
Schermer T, Heijdra Y, Zadel S, van den Bemt L, Boonman-de Winter L, Dekhuijzen R, Smeele I. Flow and volume responses after routine salbutamol reversibility testing in mild to severe COPD. Respiratory Medicine 2007; 101: 1355-1362.
Tashkin DP, Celli B, Decramer M, Liu D, Burkhart D, Cassino C, Kesten S. Bronchodilator responsiveness in patients with COPD. Eur Respir J 2008; 31: 742-750.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License