I was reviewing spirometry reports and noticed several patients in a row with an early termination of exhalation that was not reflected in the reported expiratory time. This is far from the first time I’ve noticed this but seeing several examples more or less at the same time got me curious about how the software was determining expiratory time.
The ATS/ERS standards are somewhat mute on how the total expiratory time of a spirometry effort is determined. The closest the standard comes to addressing this is the end-of-test (EOT) criteria:
“The volume–time curve shows no change in volume (<0.025 L) for >=1 s[econd]”
But this is meant primarily as a quality indicator to show the patient has really achieved an adequate exhalation and not as a definition of expiratory time. In fact total expiratory time is not defined in the ATS/ERS standards at all and this leaves it up to individual equipment manufacturers to determine when a spirometry effort is over. This is a problem because the ATS/ERS standards also say that patients should:
“exhale for >=3 s in children aged <10 yrs and for >=6 s in subjects aged >10 yrs.”
So despite not being defined, the length of a spirometry effort is a critical quality indicator.
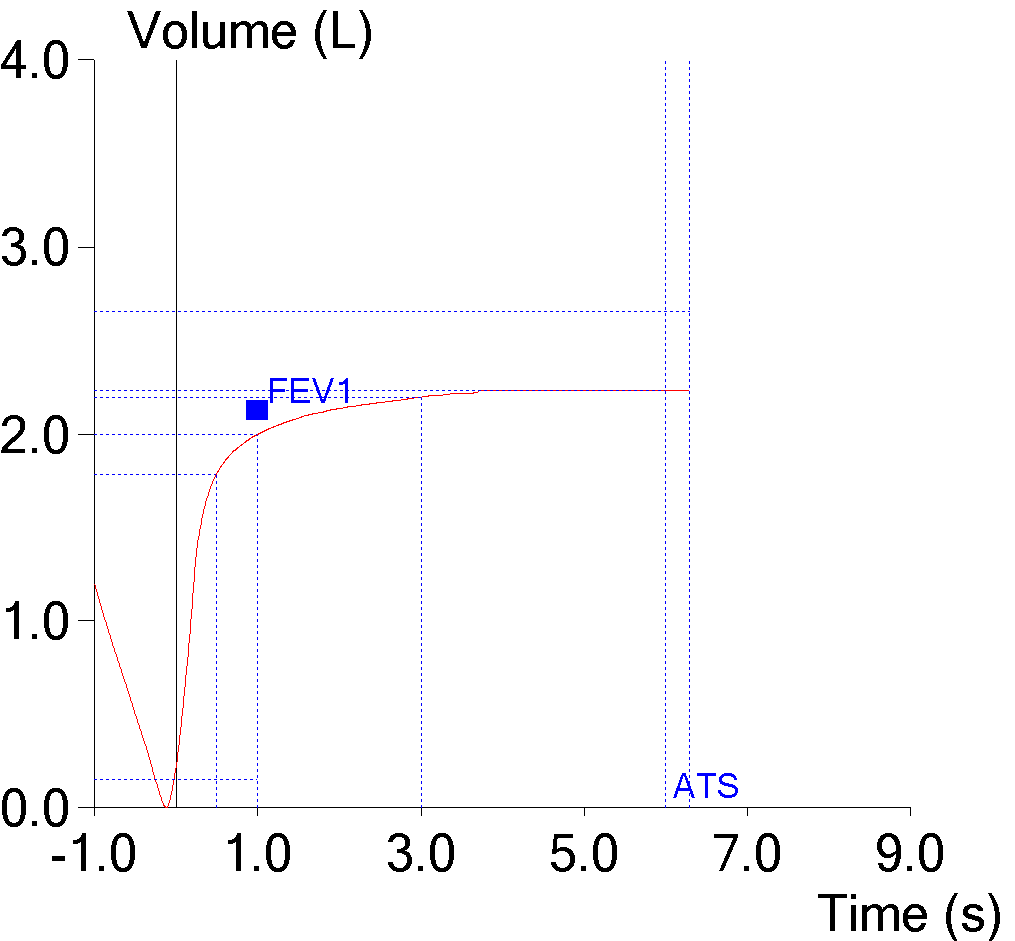
This spirometry effort was reported at being 6.41 seconds long, but it is clear the patient stopped exhaling well before that time. I downloaded the raw data for the effort into a spreadsheet and by looking at the volume and flow results I was able to see the patient had actually exhaled for 3.96 seconds. During the final 2.45 seconds there was no change in volume (the maximum change was 0.007 L, which is probably due to electronic noise). This makes it apparent that even if there is no change in expiratory volume our spirometry software continues to time the effort.
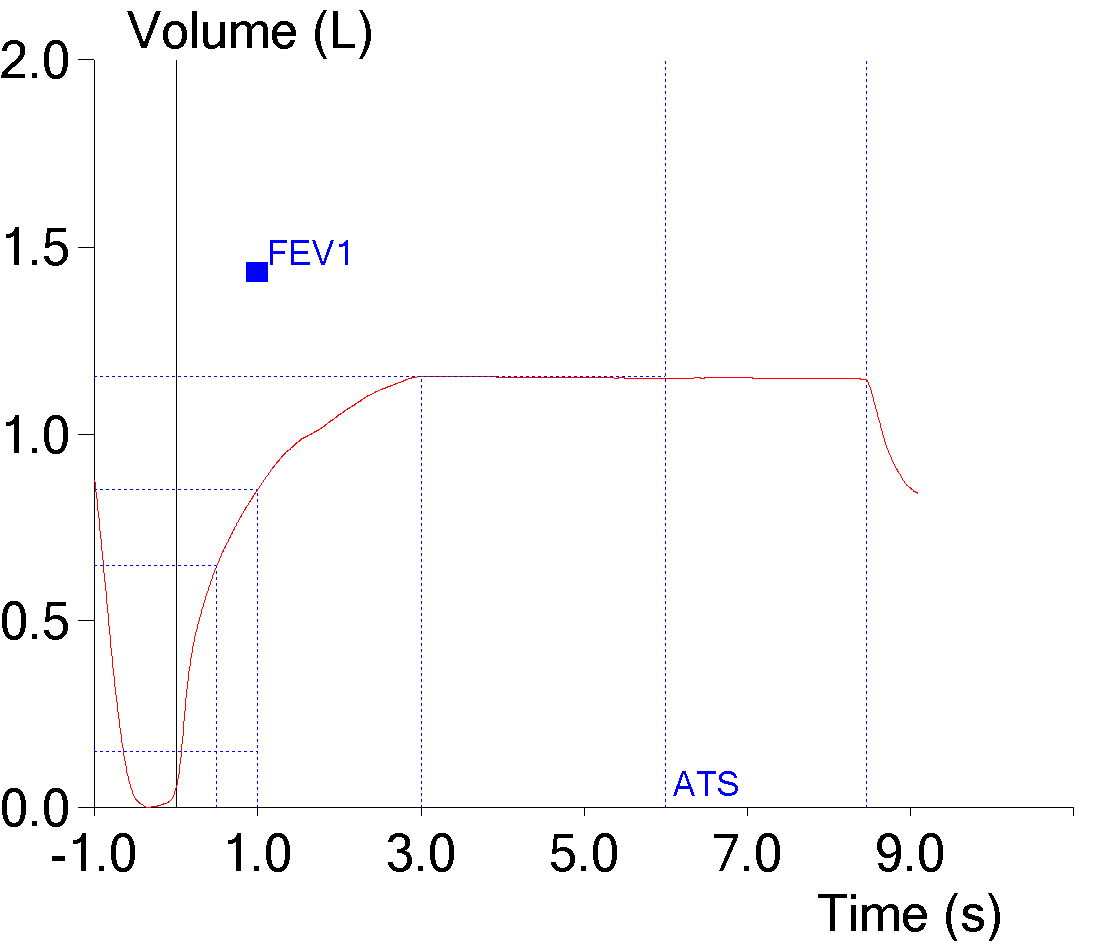
This spirometry effort was reported as being 8.29 seconds long, but the maximum exhaled volume occurred at 2.98 seconds and exhaled volume decreased slightly thereafter although the maximum decrease was only about 0.011 L. In one sense this is below the EOT threshold, but it is a negative volume and the EOT criteria is for a positive volume. What this does mean is that the software is not using a decrease in volume as a way to determine the end of exhalation, or at least it’s looking for a larger decrease than this.
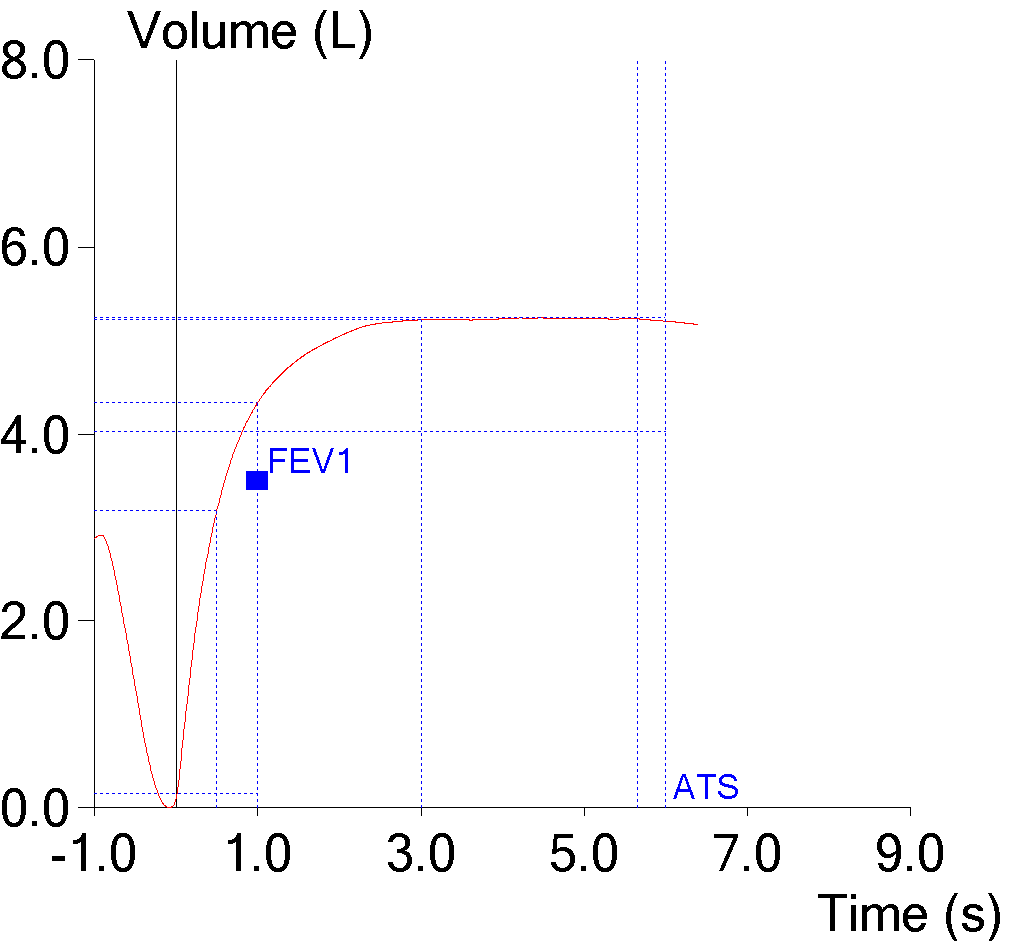
This spirometry effort was reported as 5.63 seconds. That’s less than 6 seconds but the real end of the effort occurs at around 3 seconds (although the maximum exhaled volume occurs around 4.2 seconds). The maximum change in volume between 3.00 seconds and 5.63 seconds was 0.023 L, which meets the EOT criteria but also means that our spirometry software doesn’t use the EOT criteria to determine expiratory time. This isn’t exactly a surprise, but it’s nice to see it verified.
So how does this software determine where the test ends? By looking at the raw data for a number of spirometry efforts my best guess (and it really is a guess but it fits what I saw) is that after the spirometry effort is over, the software first looks for the maximum exhaled volume. The software then continues to look forward until it finds an inspiratory flow rate of around -0.1 L/sec and uses this as an indicator that inspiration has begun. The software then looks backward from this point until it finds a zero or positive expiratory flow and when it does it marks this as the end of test.
Note: Interestingly, for our lab software it is evident that the computer algorithm used to measure expiratory time is not the same that is used to measure the FVC volume. As mentioned previously, when a patient’s expiratory effort includes a pause and a small inspiration before completing the effort (not a good quality effort of course, but sometimes you have to work with what you can get), the FVC volume is taken from the largest expiratory volume that occurred before the inhalation, and not the largest expiratory volume that occurred during the entire effort. This causes a discrepancy between the expiratory time for the measured FVC volume and the reported expiratory time for the entire effort.
Expiratory time is an important quality indicator for spirometry and many if not most test systems are able to report this value. The problem is that there is no official definition or approach for measuring expiratory time and every manufacturer must decide for itself how to measure it. For the majority of spirometry efforts this is likely not a problem, but when a patient stops exhaling this doesn’t mean that the reported expiratory time reflects this.
It could be argued that the time a patient continues to try to exhale even though there is no significant expiratory flow should be counted as expiratory time. The problem with this thought is that there is no way to determine why expiratory flow has stopped and inspiratory flow hasn’t started. It could be a that there is no more volume to exhale despite a continued effort, it could be glottal closure, or it could be that the patient has just arbitrarily stopped exhaling.
Like many other testing issues, how expiratory time is determined is not explained in our lab system’s manuals. I was able to download raw test data that let me examine how well (or not so well) our software was determining expiratory time but this is not an option on many other manufacturer’s test systems.
In addition, I’ve run across a couple spirometry systems that did not display or print a volume-time curve, and for these systems it is not possible to verify the reported expiratory time in any way. I would agree that a volume-time curve is not as informative as a flow-volume loop, but it is still useful as a way to verify a number of test quality issues that don’t appear (or don’t appear all that well) in a flow-volume loop.
Hopefully, the next version of the ATS/ERS standards for spirometry will include a definition of expiratory time. My personal inclination would be to use the point where the maximum exhaled volume occurred as the expiratory time but I can see a couple circumstances where the results from this approach (particularly since electronic noise can cause flow and volume signal excursions where none really exist) would be debatable, so some definition of a zero flow signal similar to EOT would be needed as well. In any case, I would argue that a period of zero expiratory flow at the end of a spirometry effort should not be included as part of the reported expiratory time and that whenever possible the reported expiratory time should always be verified against a volume-time curve.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS task force: Standardisation of lung function testing. Standardisation of spirometry. Eur Respir J 2005; 26: 319-338.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License