The ATS/ERS standard for spirometry recommends reporting the highest FEV1 and the highest FVC even when they come from different tests. Our lab software allows us to do this, but only with some annoying limitations. One of the bigger limitations has to do with how expiratory time is reported. In particular, expiratory time is lumped in with a number of other values like Peak Flow (PEF) and FEF25-75. As importantly, the flow-volume loop and volume-time curve can only come from a single effort.
Our lab software defaults to choosing a single effort with the highest combined FVC+FEV1. The technician performing the tests will override this when other spirometry efforts have a larger FVC or a better FEV1 (which is chosen not just if it is higher but also on the basis of peak flow, back-extrapolation and other quality indicators). The usual order for this is to first choose a spirometry effort with the “best” FEV1, then if there is a different effort with a larger FVC that FVC is selected for reporting. When things are done this way what happens is that the expiratory time, flow-volume loop and volume-time curve that come from the effort selected for its FEV1 are reported. This means is that the expiratory time and volume-time curve often don’t match the reported FVC.
I always take a look at the raw test data whenever a spirometry report comes across my desk with an expiratory time less than 6 seconds or the technician noted that the spirometry effort is a composite. What I often find is that even though the reported expiratory time may be low, the FVC actually comes from an effort with an adequate expiratory time. Although I can select the right expiratory time the problem is that doing so also selects the PEF and the PEF from the effort with the highest FVC is often significantly less than the effort from the best FEV1. The same problem applies to selecting the volume-time curve since the associated flow-volume loop often doesn’t match the effort with the best FEV1 and best PEF. For these reasons I only select the correct expiratory time and volume-time curve when it doesn’t really affect the flow-volume loop and PEF.
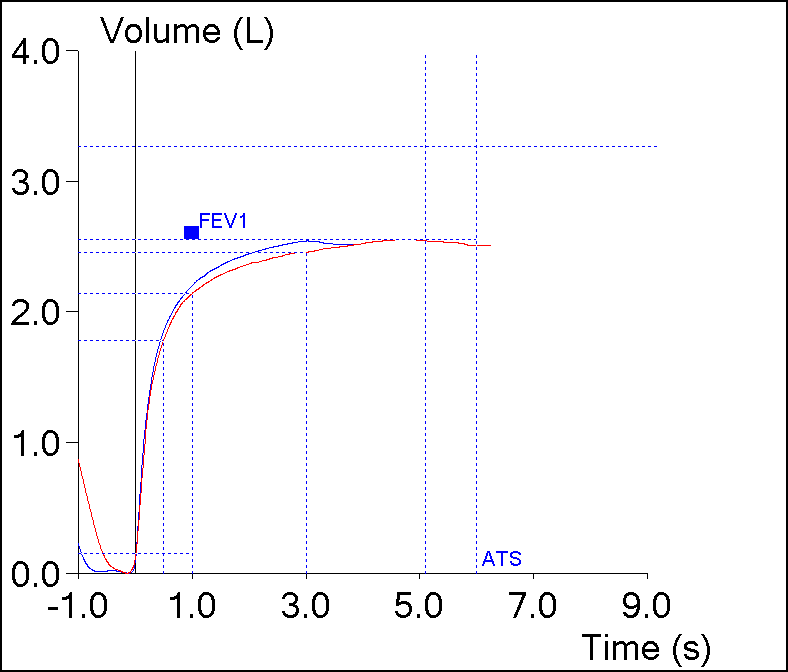
However, I’ve always assumed that the expiratory time from the effort with the highest FVC was probably the most correct expiratory time. Yesterday however, this spirometry effort came across my desk:
| Blue | Red | |
| FVC: | 2.53 | 2.54 |
| FEV1: | 2.19 | 2.13 |
| FEV1/FVC: | 86 | 84 |
| PEF: | 6.94 | 5.07 |
| Exp. Time: | 3.05 | 5.09 |
The expiratory time from the effort with the highest FVC was about 2 seconds longer than the effort with the best FEV1, but the difference in FVC from the two efforts was only 0.01 L. Strictly speaking the effort with the highest FVC does have the longest expiratory time but should this expiratory time be considered correct?
In one sense it really doesn’t matter in this case because even though the expiratory time from the largest FVC is longer, it is still under 6 seconds and that means it’s still probably a suboptimal test effort. But what if the effort the FEV1 came from was 5 seconds long and the effort the FVC came from was 7 seconds long and the difference was still only 0.01 L?
What if there were two spirometry efforts with the same FVC and FEV1 and one had an expiratory time of 5 seconds and the other 7 seconds? Would it be acceptable to select the spirometry test that was 7 seconds long because it met the ATS/ERS criteria or should the test with the shorter expiratory time be selected because it better reflects the patient’s effort and ability?
The answer has to be the shorter expiratory time because the longer time is falsely elevated.
But part of the problem is that there is no official definition of expiratory time in the ATS/ERS spirometry standards. Most test systems use an inspiratory flow or volume that’s above some arbitrary threshold as the end of exhalation or when the technician performing the test ends it manually. This is a probably a reasonable rule-of-thumb approach but it also means that expiratory time has a fairly high level of uncertainty.
At least once or twice in the past researchers have put forward the notion that measuring the expiratory time at 98% of the vital capacity would be a way to standardize expiratory time. This idea never gained any traction but it was also proposed before the ATS/ERS included expiratory time as a quality indication for spirometry. Perhaps it’s time to resurrect this notion or something like it (I’d vote for 95% of the FVC).
We take it for granted that expiratory time should be a good indication of test quality (and it probably is) but given the uncertainty of the expiratory time measurement I’m not sure how to prove that. In addition although a 6 second expiratory time seems to be reasonably correct it is still an arbitrary length of time. If expiratory time is going to be used as a quality indicator shouldn’t it also acknowledge that expiratory time generally increases with age?
Note: Even though the fact that expiratory time increases with age is something we all “know” to be true, I don’t think I’ve ever seen this studied. Nor do any of the spirometry reference equations include predicted expiratory time. Given this is the case, how do we know what an acceptable expiratory time really is?
I’m not saying that expiratory time isn’t useful as an indication of test quality but I do think it’s clear that we need a better definition of how to measure expiratory time and a better definition of what constitutes an acceptable expiratory time.
This is getting a bit far off track however, since the more immediate problem is that I can’t always get our lab software to report the expiratory time for the largest FVC, at least not without compromising other reported values. I also can’t get the volume-time curve to always come from the spirometry effort with the largest FVC for much the same reasons. Admittedly it’s just my opinion the flow-volume loop and PEF should be associated with the FEV1, and the expiratory time and the volume-time curve with the FVC; it’s not in the ATS/ERS standards but doesn’t it make sense to do it this way?
Note: Selecting FVC and FEV1 from different test efforts does leave somewhat of a quandary about which effort the FEF25-75% (not that I believe it’s of any real use) and the FEF50% and other similar measurements should come from. It’s not an issue for me since I don’t think that any of these measurements are particularly useful when assessing spirometry. It’s an interesting problem however, since all of these measurements depend on both expiratory volume and expiratory flow rates and the criteria for selecting the “best” FEV1 and FVC aren’t necessarily the same criteria for the “best” FEF50%.
The fact that our lab software doesn’t let me mix-and-match the reported values better is due partly to decisions our equipment manufacturer made while designing and writing the software but maybe also in larger part because the ATS/ERS spirometry standards don’t address or even particularly acknowledge this issue. I don’t disagree that the “best” FEV1 and FVC should be selected from different spirometry efforts whenever necessary, but this has left the way that other measurements are selected as indeterminate. Hopefully a better definition for expiratory time and how results other than the FVC and FEV1 should be selected and grouped will be addressed whenever the ERS/ATS releases the next set of spirometry standards.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License