I was reviewing a PFT recently and noticed that the FEV1 was severely reduced and that the FRC and RV were both elevated. This is a pattern we associate with obstructive gas trapping but I’ve also been reviewing textbooks on pulmonary function interpretation and have found that there isn’t any kind of a universal definition for this.
Hyperinflation and gas trapping are used somewhat interchangeably but the distinction is that gas trapping causes hyperinflation. Gas trapping occurs to some extent in everybody but usually at lung volumes below FRC. The lung volume at which gas trapping occurs rises with age and with obstructive lung disease. Hyperinflation is usually considered to be an increase in FRC but FRC is a dynamic lung volume and there is a range in the response to increased gas trapping. The normal progression from mild to very severe COPD goes something like this:
| FEV1: | FVC: | FRC: | RV: | TLC: | RV/TLC: | |
| Mild | ↓ | – | – | – | – | – |
| Moderate | ↓↓ | ↓ | – | ↑ | – | ↑ |
| Severe | ↓↓↓ | ↓↓ | ↑ | ↑↑ | – | ↑↑ |
| Very Severe | ↓↓↓↓ | ↓↓↓ | ↑↑ | ↑↑↑ | ↑ | ↑↑↑ |
Gas trapping and hyperinflation have significant consequences for an individual’s exercise capacity and level of dyspnea. It is an important clinical finding but from a PFT point of view when is it clearly present?
Hyperinflation can’t be considered to be present when there just is a reduced FEV1 and FVC can be reduced along with FEV1 for reasons that have nothing to do with airway obstruction. This means that lung volumes need to be measured in order to assess the presence of hyperinflation.
I used to think that spirometry and DLCO tests were hard and that lung volumes were easy. In retrospect this had a lot more to do with how hard it was to get a patient to perform the tests correctly and not how easy it was to assess test quality. All lung volume measurements more or less start by measuring FRC and without sufficient care (regardless of whether the technique is helium dilution, nitrogen washout or plethysmography) it is relatively easy to overestimate (and harder but not impossible to underestimate) FRC.
The best way to verify that lung volume measurements are accurate is when they are reproducible. Interestingly, the ATS/ERS standards on lung volumes only discusses repeatability for plethysmographic FRC (+/- 5%) and not for helium dilution or nitrogen washout results. I do not think this is the correct approach since there are a number of reasons why FRC can vary from test to test without affecting the TLC and RV. For this reason we primarily look at TLC and RV when assessing reproducibility and try to make sure they are within 5%.
Even though it is my lab’s policy that lung volumes be measured at least twice there are many reasons (some good, some bad) why we aren’t always able to get two lung volume tests with acceptable quality. In these instances we have to rely on quality indicators when selecting a specific set of results but without repeatability there is always a level of uncertainty. For this reason I would be hesitant about the presence of hyperinflation when only a single set of lung volume measurements are available.
Assuming that good quality lung volume measurements are available however, is gas trapping present if the RV/TLC ratio is elevated? I’ve seen several research studies from around forty years ago where an elevated RV/TLC ratio was called the “emphysema index”. The RV/TLC ratio hasn’t been called this in a while and the phrase is now applied to specific radiological CT findings but it is clear that an elevated RV/TLC ratio has been considered a symptom of COPD for quite a while.
The RV/TLC ratio cannot be taken as a sole indication of hyperinflation because there is at least one instance (and probably more) where an elevated RV/TLC ratio is not a symptom of COPD at all. When restrictive lung disease is caused by neuromuscular weakness FRC tends to be normal but TLC is reduced and RV is elevated because the individual lacks the strength to sufficiently inhale or exhale. In these cases the RV/TLC ratio will be elevated but this has nothing to do with airway obstruction.
In fact, even though the RV/TLC ratio has been a standard element of PFT reports for as far back as I can remember there I times I wonder why it is reported at all. It’s not at all clear to me that the RV/TLC ratio is any more informative than just the RV and in addition I haven’t seen an elevated RV/TLC ratio used as part of an interpretation in decades.
So, is gas trapping present when the RV is elevated? Maybe. My problem with this is that the RV is frequently increased when SVC test quality is suboptimal. When I review results, I always compare the FVC and SVC. This is usually in order to make sure the largest VC is used to calculate the FEV1/VC ratio but it can also pinpoint problems with lung volume measurements. I expect the SVC to be at least as large as the FVC but when it is significantly less I am not surprised to see an elevated RV.
Interestingly, the ATS/ERS statements on lung volumes say nothing about using a larger FVC in place of a smaller SVC in order to determine RV and TLC. This is not all that surprising given that IC and ERV are a critical part of the calculation. Depending on whether the ERV or the IC part of the SVC maneuver is performed first then:
RV = FRC – ERV and TLC = RV + SVC
or
TLC = FRC + IC and RV = TLC – SVC.
IC and ERV are not measured from an FVC maneuver but only from an SVC maneuver. If the SVC is suboptimal, there is no way to know whether the IC or the ERV is correct or whether they are suboptimal as well. Depending on the calculation order replacing a suboptimal SVC with a larger FVC can lead to either to over- or under-estimating the RV and the TLC.
Having an SVC that is larger than an FVC is no guarantee it’s accurate since for this kind of comparison the FVC needs to be reasonably accurate as well. There are always some individuals that can’t seem to exhale longer than two seconds, if that. For these people, an SVC that is only slightly larger than what is clearly a suboptimal FVC is still a suboptimal SVC.
So what about when both FRC and RV are elevated? I think this is a reasonably clear signal for gas trapping and hyperinflation and is pretty much the standard my lab uses. Obstructive gas trapping occurs because of expiratory flow limitation and when it causes FRC to move a higher volume the FRC is then on a less efficient portion of the lung’s pressure-volume curve. This increases the work of breathing and reduces an individual’s ability to increase ventilation. To me, this has to be the definition of clinically relevant hyperinflation.
Finally, should hyperinflation be considered to be present only when TLC, FRC and RV are elevated? Hyperinflation is certainly present when this is the case but I think this misses the point somewhat. TLC does not have to be elevated for clinically relevant gas trapping and hyperinflation to be present. I’d also point out that elevated TLCs are not as common as the used to be or at least I certainly don’t see them as often as I used to. This is a good thing and I believe it is occurring because of earlier recognition and intervention of COPD as well as better medications. I would think that requiring the TLC to be elevated as well as FRC and RV as the definition of hyperinflation would be too limiting.
One problem with all of this is that lung volumes can only assess resting hyperinflation which is a consequence of relatively advanced airway obstruction. Gas trapping can occur during exercise because of expiratory flow limitation and increased ventilatory demands. When this happens FRC increases. We monitor this during our CPETs by having the patient perform an IC maneuver every two minutes during exercise. The IC lets us track the patient’s End-Expiratory Lung Volume (EELV) which is a surrogate for FRC. When IC decreases this is an indication that FRC is increasing and a sign of dynamic hyperinflation. An individual however, can have dynamic hyperinflation and still have a normal resting FRC.
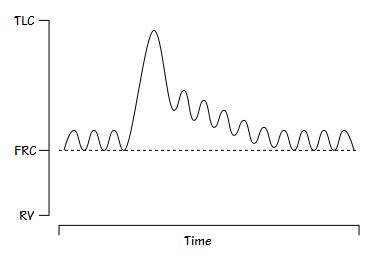
As useful as CPETs are, performing one solely to determine whether dynamic hyperinflation is occurring may be overkill. I’ve seen at least one test system intended for 6-minute walk tests that is able to measure IC which may be an interesting solution for this. Also, back in the 1970’s, before we had such new-fangled things like flow-volume loops we would place a patient on a closed-circuit spirometer and after they had settled into normal tidal breathing we’d have them take a deep inspiration:
Individuals with COPD would take several tidal breaths after the deep breath to return to their prior FRC baseline. This was a qualitative test in that there were no numbers you could get from it, just the observation that their FRC baseline shifted. I’m not sure how well this correlates with resting or dynamic hyperinflation but it was a simple test. Unfortunately I don’t know of any test systems today that would allow this test to be performed.
Hyperinflation is a clinically important finding and the earlier it is discovered the better prognosis a patient will likely have. Dynamic hyperinflation likely occurs earlier in the progression from mild to severe COPD than does resting hyperinflation but requires specialized testing to confirm its presence. Determining that resting hyperinflation is present requires attention to lung volume test quality and repeatability. Although an elevated RV is frequently a consequence of airway obstruction, and may be an early stage of hyperinflation, it is not by itself a clear sign of resting hyperinflation. Resting hyperinflation is clearly present when an individual has an increased FRC and RV, and this fact should be noted in an interpretation.
References:
Brusascoi V, Crapo R, Viegi G. ATS/ERS Task force: Standardisation of lung function testing. Standardisation of the measurement of lung volumes. Eur Respi J 2005; 26: 511-522.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License