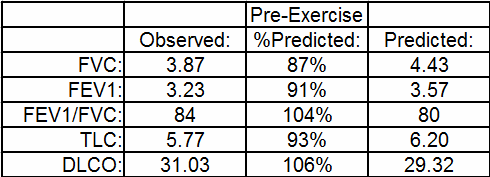
Recently I was reviewing a cardio-pulmonary exercise test (CPET) that at first glance seemed to show the patient had a pulmonary mechanical limitation. Specifically, the patient’s minute ventilation (Ve) at peak exercise was 93% of predicted. This was something you’d expect if a patient had an obstructive or restrictive lung disease but I could see right away that the patient’s baseline pulmonary function tests were actually pretty normal.
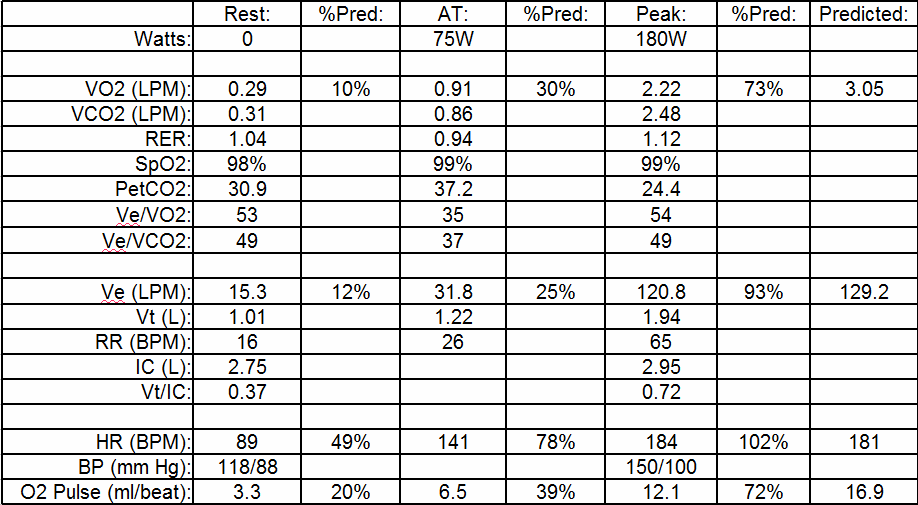
The maximum oxygen consumption was 73% of predicted so it was apparent the patient had an exercise limitation of some kind but based on a number of other factors I didn’t think it had anything to do with the mechanical aspects of the patient’s lung.
The first question that should always be asked when looking at a CPET report is whether the test was adequate or not. Although in this case the elevated minute ventilation by itself says it was, the patient’s maximum heart rate was also 102% of predicted (our threshold is 85%) and the RER at peak exercise was 1.12 (our threshold is 1.10) so it was apparent that the patient had given a good exercise test effort.
Once you get past adequacy, there are a number of odd aspects to this CPET. When looking at the ventilation data, the elevated minute ventilation (93% of predicted) and respiratory rate (65 breaths/min) at peak exercise would be something you’d expect to see in a patient with a restrictive lung disease. The patient’s TLC was normal however and in addition the Tidal Volume/Inspiratory Capacity ratio (Vt/IC) at peak exercise was only 0.72. Patients with restrictive (and obstructive) lung diseases tend to have high Vt/IC ratios, with values above 0.90 not being particularly unusual. In this case, the Vt/IC ratio of 0.72 is normal and also says that the patient still had reserves in their tidal volume available to them at that point.
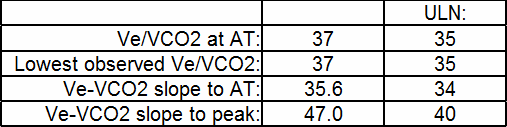
So what was driving the patient’s ventilation so high? Ventilation is usually driven by arterial carbon dioxide (PaCO2) and pH. My lab only does non-invasive exercise testing so we don’t insert arterial lines or perform arterial punctures in order to get blood gases. For this reason we rely heavily on the ventilatory equivalents, and in particular the relationship between Ve and VCO2. There are several different ways to look at these values (Ve/VCO2 at AT, lowest observed Ve/VCO2, Ve-VCO2 slope to AT and Ve-VCO2 slope to peak exercise) and we report all of them. This may appear to be overkill but even though many studies have shown both the value and the power of the Ve-VCO2 relationship there is a great deal of contradictory information about which specific relationship is most informative. I keep hoping to be able to simplify this at some point but until that time I feel it is better to report all of the Ve-VCO2 values rather try to guess which is most relevant. In this patient’s case, all values were mildly abnormal:
An elevated Ve-VCO2 is usually a strong indication of a problem with gas exchange. For this reason it is seen in obstructive lung diseases like COPD and restrictive lung diseases like pulmonary fibrosis. It is also seen however in cardiovascular diseases and this is because even mildly elevated pulmonary arterial pressures can cause micro-fracturing and micro-scarring of the pulmonary vasculature. When this happens, DLCO can remain more or less normal for prolonged periods of time but DLCO is performed at rest and does not predict gas exchange during exercise. When cardiac output increases during exercise the pulmonary capillary blood volume usually increases as well which acts to improve overall lung perfusion and ventilation-perfusion matching. A consequence of pulmonary vascular disease is therefore not only an elevated ventilation-perfusion mismatching at rest but an inability to increase pulmonary capillary blood volume during exercise.
The primary clue that this patient’s problem is probably cardiovascular in nature is their VO2 at AT, which is only 30% of the predicted maximum. The LLN for this patient’s age and sex is 44%, so they are well below normal. A low VO2 at AT is an indication of a low cardiac output or at least a diminished ability to get oxygen to the exercising muscles. Seconding this is the fact that despite indications of pulmonary vascular disease the patient did not desaturate (i.e. their SpO2 remained normal). SaO2 will remain normal even if gas exchange poor when the cardiac output is decreased by an equivalent (or greater) amount.
Finally, the Ve at AT was only 25% of the predicted maximum. At least one study has shown that when a true pulmonary mechanical limitation is present the Ve at AT will be elevated as well and for this reason we use a Ve at AT above 42% as an indicator for this.
Despite having a maximum minute ventilation of 93% of predicted, this patient’s problem was not really due to a pulmonary mechanical limitation. When patients have obstructive or restrictive lung diseases their predicted maximum minute ventilation is usually decreased as well. This patient’s predicted maximum Ve was reasonably normal but their ventilation is being driven to excessively high values probably due to a combination of ventilation-perfusion mismatching and a diminished cardiac output.
Exercise limitation is often multi-factorial. In the very strictest sense of the term this patient did have a pulmonary mechanical limitation but in this case the fact that it existed at all was likely due to a combination of pulmonary vascular and cardiovascular disease and not to a defect in the patient’s ventilation.
References:
Medoff BD, Oelberg DA, Kanarek DJ, Systrom DM. Breathing reserve at the lactate threshold to differentiate a pulmonary mechanical from a cardiovascular limit to exercise. Chest 1998; 113: 913-918.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.