Well, not necessarily anything, although as usual that depends on the circumstances. Recently I was contacted by an individual who was concerned that their DLCO had decreased from 120% of predicted to 99% of predicted. They also mentioned that their DLCO results have normally ranged from 117% to 140% of predicted over the last 9 months.
More interestingly however, they said that
“the technician told me before I even took the test that anything over 100% for DLCO is essentially a testing error.”
Wow. That statement is wrong on so many levels it’s hard to know where to start but I’ll give it a shot anyway.
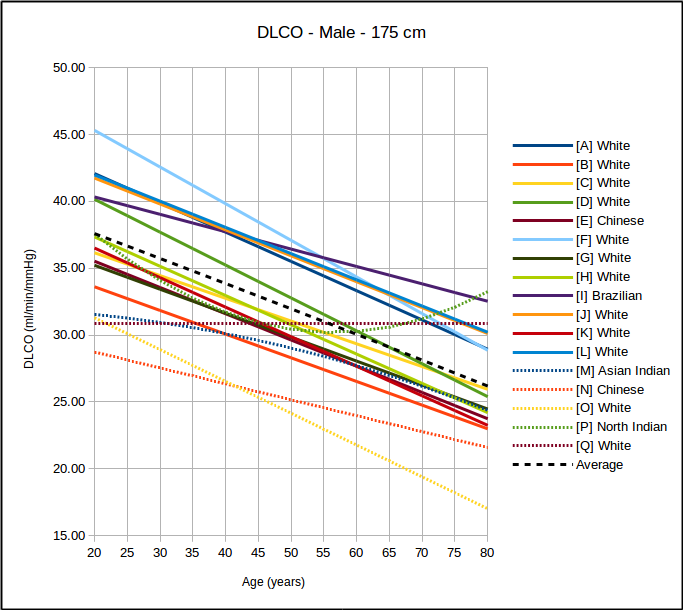
First, there are a variety of DLCO reference equations. The ATS/ERS guidelines recommends that PFT Labs pick the reference values that most closely matches their patient population but how this is done is left to individual labs. There are at least a couple dozen DLCO reference equations to choose from and probably about a half dozen of these are in common use in PFT labs around the world.
Because no patient population is ever going to precisely match those of a study this means that DLCO results are going to tend to be above or below 100% of predicted depending on which reference equation the lab is actually using. This also means that if results from otherwise normal subjects are mostly above or mostly below 100% of predicted then the wrong reference equations are being used.
Moreover, if a lab selects a DLCO reference equation based on the expectation that everybody will be either 100% of predicted or less, that is also wrong. DLCO, like all other pulmonary function results, follows a normal, bell-shaped distribution.
Reference equations are used to calculate the mean value and this means that approximately half the study population is above the mean and half is going to be below it. Admittedly most study subjects aren’t going to be too far away from the mean, but as an example Miller et al (H in the above graph) is one of the more commonly used DLCO reference equations. They did not include a lower limit of normal (LLN) in their original paper but did include extensive statistics on the study population. Although I have some significant disagreements with this approach many labs calculate the LLN for DLCO as:
For Miller et al the SEE (Standard Error of the Estimate) x 1.645 is 7.99 ml/min/mm Hg. The upper limit of normal (ULN) can be calculated the same way,
Since the predicted DLCO for a 50 year old, 175 cm male is 30.77 ml/min/mmHg, the ULN for the same patient would be 38.76 ml/min/mmHg, but that value is 126% of predicted. So it’s easily possible to be within normal limits, but above 120% of predicted.
Probably far more pertinent to the person who contacted me about this issue (who has a tentative diagnosis of reactive airways disease and a BMI > 30), is that DLCO is frequently elevated in both asthma and in obesity. In a study of 245 patients with a DLCO >140% of predicted, Saydain et al found that most of the patients had a diagnosis of either asthma, obesity, or both. The reasons for this are unclear but subjects with asthma have been noted to have increased airway vascularization, and therefore an elevated capillary surface area in the lung. Other researchers have noted that asthma is associated with an elevated perfusion of the lung apices. And numerous other researchers have shown that obese individuals have an elevated capillary blood volume and an elevated cardiac output.
So, is an elevated DLCO abnormal in these individuals? Probably not since no one has shown that an elevated DLCO is an adverse clinical findings in either asthma or obesity but in particular it also means that an elevated DLCO should not be dismissed as a testing error in these patients.
A much smaller minority in Saydain et al’s study had pulmonary hemorrhage, polycythemia or left-to-right shunting. These are adverse clinical findings and for this reason, even more so than asthma or obesity, an elevated DLCO should not be ignored as a testing error.
This is not to say that there aren’t DLCO testing errors that lead to an elevated DLCO and I’d be interested in what that lab’s policy was on checking test systems when a patient has an elevated DLCO.
The DLCO test is sensitive to the pulmonary capillary blood volume and this can be affected by excess resistance during inspiration and by a Müller maneuver (inspiratory effort against a closed mouthpiece) both of which cause a negative intrapulmonary pressure and act to increase the capillary blood volume. The 2017 ERS/ATS DLCO standards explicitly mentions the need to avoid a Müller maneuver and the standard’s equipment specifications includes the statement that:
“Circuit resistance must be <1.5 cmH2O·L−1·s−1 up to 6 L·s−1 flow. If a demand-flow regulator is used on a compressed test gas cylinder, the maximal inspiratory pressure required for 6 L·s−1 inspiratory flow through both the circuit and the valve must be <9 cmH2O.”
The demand valve specifications in the ERS/ATS standard are not based on any particular evidence however, and are essentially a way to grandfather-in existing test systems. To my knowledge the effect that an inspiratory pressure of -9 cm H2O has on DLCO has not been studied (although at least one equipment manufacturer I’m familiar with has designed their DLCO systems without demand valves specifically because of their concerns with this issue). Regardless of whether or not an inspiratory pressure of -9 cm H2O affects DLCO, a sticking demand valve will significantly increase a subject’s inspiratory pressure. This will probably increase the measured DLCO as well and should be considered a testing error.
Interestingly, although the ERS/ATS standard acknowledges that exercise affects pulmonary capillary blood volume (due to an elevated cardiac output), other than stating that:
“…the subject must be seated comfortably throughout the test procedure…”
it does not specify any pre-test waiting period although a minimum 4 minute between-test waiting period is recommended. This waiting period however, is intended to allow for adequate elimination of test gas from the lungs and not as a way to ensure the patient is in a resting state.
Note: I’ve used the effects of exercise as a talking point when teaching students about DLCO testing. To do this I perform a DLCO on a student after they’ve sat quietly for several minutes. Next I get the test system set up for another DLCO test but first I have them walk briskly up and down the hallway for several minutes, then sit down and immediately perform another DLCO. Their second, post-exercise, DLCO is almost always at least 15% to 30% higher than their resting DLCO.
Most of the time however, testing errors such as a valve and tubing failures, a reduced inspiratory volume, a reduced breath-holding time or an inadequate or mistimed alveolar sample tend to cause a decrease in DLCO, not an increase. Having said that, I’ve run across problems with gas analyzers that can cause an elevated DLCO, and these can be hard to detect because they are often transient. The same applies to computer glitches of one kind or another.
I remain somewhat baffled about the statement that any DLCO over 100% of predicted is a testing error. What is it based on and is it blaming the patient or the test system? If the technician and the lab actually believes it, then why were the elevated DLCO’s reported anyway?
Unfortunately, I think that it’s more likely the technician was pontificating about a subject they did not understand. It’s worse if they were parroting a statement made by a co-worker, their manager or their medical director since that points to a systemic lack of understanding about testing issues and idiosyncrasies which is (also unfortunately) more common than it should be.
In my lab we get DLCO’s >140% of predicted several dozen times a year and >120% of predicted far more frequently. I always review the raw data for these tests but then I review the raw data for all DLCO tests so they are not singled out in any particular way. I don’t find any apparent testing errors with elevated DLCO results any more often than I do with regular DLCO results. I’ve also been aware of the association between asthma and elevated DLCO’s for more than 30 years so I’ve never seen any reason not to report them.
The original question however, was whether a decrease in DLCO from 120% of predicted to 99% of predicted was abnormal and I don’t have a good answer for that. Partly this is because the intrasession reproducibility of elevated DLCOs has not been studied. Partly it’s because the specific causes of an elevated DLCO in a given individual are poorly understood and for this reason it’s not possible to say whether changes like this are clinically significant or not.
It’s also unclear why this individual is having their DLCO tested so frequently. The only working diagnosis they have is mild shortness of breath and possible reactive airways disease, and those are not good reasons to repeat DLCO tests so frequently. Does their physician suspect something they haven’t yet shared or is it just the policy that DLCO is tested with each patient visit? I’m left with a number of questions but at least I was able to let them know that an elevated DLCO is actually normal for many individuals and not a testing error.
References:
Graham BL, Brusasco V, Burgos F, et al. 2017 ERS/ATS standards for single-breath
carbon monoxide uptake in the lung. Eur Respir J 2017; 49: 1600016.
Miller A, Thornton JC, Warshaw R, Anderson H, Teirstein AS, Selikoff IJ. Single breath diffusing capacity in a representative of Michigan, a large industrial state. Am Rev Resp Dis 1983; 127: 270-277.
Saydain G, Beck KC, Decker PA, Cowl CT, Scanlon PD. Clinical significance of elevated diffusing capacity. Chest 2004; 125: 446-452.
Tanaka H, Yamada G, Saikai T, Hashimoto M, Tanaka S, Suzuki K, Fujii M, Takahashi H, Abe S. Increased airway vascularity in newly diagnosed asthma using a high-magnification bronchovideoscope. Am J Respir Crit Care Med 2003; 168: 1495-1499.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

Hi Richard,
Up until recently I worked with a private pulmonologist for nearly 15 years and we followed many repeat patients with elevated DLCO’s.
Very high DLCO’s were seen with patients who were morbidly obese (140% predicted, and higher), and the average asthmatic patient who wasn’t obese (with no other known pathology), had DLCO’s averaging around 120-130% predicted. The very highest DLCO’s (sometimes over 160% predicted) were seen seen with patients who were morbidly obese in combination with asthma.
Whenever the elevated DLCO in either group of these patients dropped significantly, it almost always was a good sign. In the obese patients, their DLCO came down when they lost a considerable amount of weight, probably because cardiac output was reduced. In the asthmatics, the DLCO usually came down in response to treatment, where we saw a significant improvement in FVC, FEV1 and FEF 25, 50 and 75. With many of these patients their lung scans showed a lessening of perfusion in the apices of the lung. Although no one knows the actual etiology of the increased perfusion in the apices of the lungs of asthmatics, it is well documented.
So, to contribute to the discussion, I would say that a decrease in a higher than predicted DLCO in cases of asthma and morbid obesity is probably a good sign, unless some other undiagnosed damage to the lung parenchyma, or pulmonary micro circulation, is taking place.
If the DLCO starts to go down in the asthmatics without significant improvement in spirometry, or it goes down in the morbidly obese patients without weight loss, there’s a good chance something else is going on, and raises a red flag.
Hope this helps,
Ira
Whenever the obese patients lost a significant amount
Ira –
Thanks for the input. I’d like to be more definitive about changes in an elevated DLCO but my lab rarely repeats DLCO tests on patients with asthma any more often than several years apart.
– Richard
Just wanted to point out – in regards to reference equations – that the GLI TLCO predicted equations were released in the ERJ this month: http://erj.ersjournals.com/content/50/3/1700010
Ron –
Thanks for the heads-up. I’ve got to get some new glasses. Looked at that issue and never saw the article.
Regards, Richard
Hi there, just studying for my board exams, your sites been a great help!
Can I check if all causes of higher cardiac output result in elevated DLCO?
For example in Thyroid disease, Pregnancy, Liver disease?
Anand –
The relationship between cardiac output and DLCO is complex. An increased cardiac output tends to cause an increase in pulmonary capillary blood volume and, even more importantly, better ventilation-perfusion matching across the lung, both of which cause an increased DLCO. An increased cardiac output also causes a decreased pulmonary capillary transit time and up to a point this exposes more blood to the DLCO test gas and therefore a greater uptake of carbon monoxide but when transit time gets too short then any further increases in CO no longer cause an increase in DLCO. In either case any increase in DLCO is very approximately 40%-50% above baseline and cardiac output can easily increase 200% to 300% (even higher in trained athletes) so there is no precise correlation between increase in cardiac output and DLCO.
However, this all presupposes a fairly normal Qs/Qt, and in liver disease in particular (hepatopulmonary syndrome) there is an increase in the “depth” of the pulmonary capillary blood such that CO (and O2) cannot reach the red blood cells on the far side of the capillary in the time available. In fact, the increase in resting CO in hepatopulmonary syndrome is primarily due to hypoxia. Any pulmonary vascular syndrome that has a high Qs/Qt will not necessarily show a correlation between cardiac output and DLCO.
Pregnancy is often accompanied by a reduction in TLC and to some extent this tends to counterbalance increases in DLCO. More specifically, the decrease in TLC is accompanied by an increase in Qs/Qt because of hypoventilation of the lower portions of the lung and in some cases is potentially significant enough to cause hypoxia. In general though, DLCO tends to increase in the early stages of pregnancy and returns to normal in the latter part but it’s not clear this is due to any changes in cardiac output.
I’m not sure what to say about thryoid disease. I’ve checked several of the textbooks I have on hand and there is no specific mention of thyroid disease and DLCO. More than one mentioned that thyroid disease is often accompanied by other cardiovascular problems, often with a reduced maximum VO2, so I guess it depends on the patient.
Regards, Richard
Thank you, that’s been a great help!
A further question I had with regards to capillary transit time, I might be getting things mixed up here. I was under the impression that CO is a diffusion limited gas as it binds so rapidly to Hb that it has a negligible effect on the partial pressure in blood and therefore no effect on the pressure gradient so it will continue diffusing across irrespective of the perfusion per se. Why then does capillary transit time have any effect on the DLCO? I can see why it would have an effect on Oxygen exchange (as it moves from being a perfusion limited to a diffusion limited gas in diseased states during exercise, so it would worsen in this case) but not Carbon Monoxide exchange. Is it simply just to do with greater availability of Hb molecules to bind with as opposed to greater blood volume passing through (which has no effect on CO exchange)?
Anand –
My thought is that the diffusion of carbon monoxide across the alveolar-capillary membrane takes a certain amount of time. As cardiac output increases at some point the amount of carbon monoxide that can diffuse across the membrane isn’t enough to fill all the available binding sites on hemoglobin and this causes a limit beyond which DLCO cannot increase. If this wasn’t the case then DLCO would scale linearly with cardiac output but it doesn’t and DLCO reaches its maximum value below maximum cardiac output. I don’t remember seeing any research however, that looked solely at the relationship between cardiac output and DLCO so this is my take on what happens and I could well be missing something.
Regards, Richard
Great thank you for explaining quite a complicated concept Richard!
Regards
Anand
Hi Richard,
Just wanted to make a quick comment about why DLCO increases in the early stages of pregnancy.
About 25 years ago I did a five year study of 1,100 patients, over a vast range of pathology, exploring how it effected sedimentation rates. One of the things I discovered was that, in pregnant women, their hematocrits increased to the point where it could be considered to be polycythemic, often in the 18-20 range. I was not aware, as you pointed out, that this changes in the latter stages of pregnancy.
Although I’m not certain what function the increased hematocrit serves, it could easily explain why the DLCO would be elevated.
Hope this helps a little,
Ira