Recently I reviewed a set of completely irreproducible spirometry results. The patient had made eight attempts and the FVC, FEV1 and Peak Flow were different every time. In particular, there were frequent stops and starts during exhalation. I’ve always wondered why some patients have so much difficulty with what should be a simple test and although in this particular case it could simply be glottal closure I wondered if it could be Vocal Cord Dysfunction (VCD). For this reason I spent some time reviewing the literature.
Vocal Cord Dysfunction is defined as the paradoxical closure of the vocal cords with variable airflow obstruction that often mimics asthma and in fact VCD is often mistaken for refractory asthma. Unfortunately, for this reason individuals with VCD are often treated with corticosteroids and bronchodilators for years without any improvement of their symptoms.
The gold standard for diagnosing VCD is direct visualization of the vocal cords with a laryngoscope. Characteristically, the anterior (frontal) two-thirds of the vocal cords are closed with a narrow posterior glottal chink. The difficulty with this is that VCD symptoms are often transitory and a large number of patients that are suspected to have VCD are asymptomatic when a laryngoscopy is performed.
Since most PFT labs are not equipped with laryngoscopes nor are they prepared to perform a laryngoscopy at a moment’s notice we have to rely on the tests that measure airflow. Although the wheeze and shortness of breath that accompanies VCD mimics asthma the most common problem associated with VCD is inspiratory obstruction. The flow-volume loop pattern is therefore that of a variable extrathoracic airway obstruction.
Many individuals with VCD have reduced inspiratory flows with an elevated MEF@50%/MIF@50% ratio even when not symptomatic. Because the inspiratory obstruction is primarily in the vocal cords and not the airways most individuals with VCD do not have a significant response to bronchodilators. Because of the inspiratory obstruction, symptomatic individuals with VCD tend to have an MVV that is reduced well below the expected FEV1 x 40.
Although VCD is usually described as being primarily an inspiratory obstruction some individuals with VCD have expiratory instead of inspiratory obstruction, and many have both inspiratory and expiratory obstruction. When expiratory obstruction occurs it causes the flow-volume loop and spirometry to mimic results that would be seen in mild to moderate airway obstruction.
Some researchers have indicated that VCD is associated with a hyper-reactive upper airway and have shown that VCD symptoms can be elicited during methacholine, exercise and cold air challenges. The primary goal of these tests is usually to assess decreases in FEV1 but for VCD it is an increase in inspiratory obstruction that is important. For this reason, an individual with VCD can become symptomatic during a challenge test but often do not show a significant change in FEV1.
Although most individuals with VCD do not have a significant response to bronchodilators it is possible to have both VCD and asthma and at least one study reported an incidence of asthma with VCD in 55% of their study population although most studies have reported a much smaller proportion.
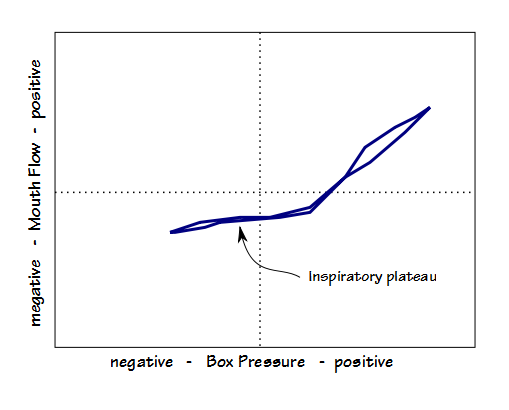
When airway resistance is measured symptomatic individuals with VCD have a fairly distinct Raw loop that shows an inspiratory flow plateau. Raw in general is also usually elevated.
Some researchers have suggested that there are two distinct types of VCD: spontaneous and exercise-induced. Spontaneous VCD occurs without any specific precipitating factors. It is usually not triggered by exercise and can occur at any time. Exercise-induced VCD is usually only precipitated by exercise and individuals are usually symptomatic only during exercise. When tidal loops are obtained during exercise in individuals with exercise-induced VCD they often show a flattening in both inspiratory and expiratory flows. One case study indicated that a inspiratory sawtooth pattern also appeared during exercise.
Vocal cord dysfunction occurs for a variety of reasons and the one that is most commonly put forward is that it has psychogenic causes, and to some extent this may well be true. A significant number of individuals with VCD have anxiety and personality disorders. As well as exercise however, VCD is also associated with gastro-esophageal reflux disease (GERD), chronic rhinosinusitis, inhaled irritants (ammonia, chlorine, cleaning fluids, smoke) and certain neurologic disorders.
VCD also occurs post-operatively and this has been attributed to the possible trauma of the vocal cords during intubation, trauma from inflation of the tracheal cuff and nerve injury from central venous cannulation. Post-op VCD has been severe enough to require re-intubation and even tracheostomy in some cases.
The incidence of VCD is unclear. Different studies have variously reported that 2.5%, 2.8%, 9.5%, 15% and 22% of subjects with stridor and/or dyspnea referred to their studies have VCD but how common it is in the general population has never been estimated. VCD appears to be more common in females than in males and the ratios of female to male in study populations has been reported to be between 2:1 and 3:1.
The report that got me to thinking about VCD showed primarily irreproducible spirometry with mostly truncated expiratory efforts. Inspiratory flows, when they were captured, were relatively normal. When spirometry efforts are discussed in the VCD literature, inspiratory obstruction has been the most commonly reported feature but most researchers have also indicated that this is variable and that often not even a majority of their study population shows this. Occasionally, the irreproducibility of spirometry results has been noted in passing and one case study noted frequent glottal closure, but this aspect hasn’t been studied in any detail so it’s not clear just how reproducible or irreproducible spirometry in individuals with VCD actually is. A related question would be whether irreproducibility or particular forms of irreproducibility are in themselves a potential indication of VCD. So does did this particular patient have VCD? I’d say it was certainly possible but it’s just not possible to be certain from the spirometry results alone.
VCD should be considered as a potential diagnosis for patients that appear to have asthma but do not respond to treatment with bronchodilators and corticosteroids. Despite being a somewhat variable aspect inspiratory obstruction is the primary feature seen in patients with symptomatic VCD. For this reason care needs to be taken when performing spirometry to include a good inspiratory maneuver (particularly during challenge testing). Individuals with VCD tend to show airway obstruction mostly when symptomatic however, and an actual diagnosis of VCD is multi-factorial. Although spirometry (and other pulmonary function tests) can suggest the presence of VCD, they are not in any way definitive.
References:
Deckert J, Deckert L. Vocal cord Dysfunction. Am Fam Physician 2010; 81: 156-159.
Doshi DR, Weinberger MM. Long-term outcome of vocal cord dysfunction. Ann Allergy Asthma Immunolo 2006; 96: 794-799.
Goldman J, Muers M. Editorial: Vocal cord dysfunction and wheezing. Thorax 1991; 46: 401-404.
Haverkamp H, Miller J, Rodman J, Romer L, Pegelow D, Santana M, Dempsey J. Extrathoracic obstruction and hypoxemia occurring during exercise in a competitive female cyclist. Chest 2003; 124: 1602-1605.
Kenn K, Balkissoon R. Vocal cord dysfunction: what do we know? Eur Respir J 2011; 37: 194-200.
Morris MJ, Deal LE, Bean DR, Grbach VX, Morgan JA. Vocal cord dysfunction in patients with exertional dyspnea. Chest 1999; 116: 1676-1682.
Morris MJ, Christopher KL. Diagnostic criteria for the classification of vocal cord dysfunction. Chest 2010; 138(5): 1213-1223.
Newman KB, Mason UG, Schmaling KB. Clinical features of vocal cord dysfunction. Am J Respir Crit Care Med 1995; 152: 1382-1386.
Perkins PJ, Morris MJ. Vocal cord dysfunction induced by methacholine challenge testing. Chest 2002; 122: 1988-1993.
Shafei H, El-Kholy A, Azmy S, Ebrahim M, Al-Ebrahim K. Vocal cord dysfunction after cardiac surgery: an overlooked complication. Eur J Cardio-Thoracic Surg 1997; 11: 564-566.
Stanton AE, Bucknall CE. Vocal cord dysfunction. Breathe 2005; 2(1): 30-37.
Tonini S, Dellabiana A, Costa CM, Lanfranco A, Scafe F, Candura SM. Irritant vocal cord dysfunction and occupational bronchial asthma: differential diagnosis in a health care worker. Int J Occup Med and Environ Health 2009; 22: 401-406.
Vlahakis NE, Patel AM, Maragos NE, Beck KC. Diagnosis of vocal cord dysfunction. The utility of spirometry and plethysmography. Chest 2002; 122: 2246-2249.
Watson MA, King CS, Holley AB, Greenburg DL, Mikita JA. Clinical and lung-function variables associated with vocal cord dysfunction. Respir Care 2009; 54(4): 467-473.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License


I have completed a study which shows that a higher FVC% predicted compared to FEV1 is suggestive of VCD. I’m trying to understand the mechanism behind this, do you have any thoughts? 💭
Claire –
I guess my first question is how many VCD patients you had and what your criteria was for selecting them. I would also ask what reference equations you’re using and whether they’re appropriate to your population. Taken at face value however I have difficulty seeing any correlation. Sorry.
– Richard