Last week I was discussing the use of DL/VA to differentiate between the different causes of gas exchange defects with a physician. DL/VA is DLCO divided by the alveolar volume (VA). It is an often misunderstood value and the most frequent misconception is that it is a way to determine the amount of diffusing capacity per unit of lung volume (and therefore a way to “adjust” DLCO for lung volume). This is not the case because dividing DLCO by VA actually cancels VA out of the DLCO calculation and for this reason it is actually an index of the rate at which carbon monoxide disappears during breath-holding.
[Note: The value calculated from DLCO/VA is related to Krogh’s constant, K, and for this reason DL/VA is also known as KCO. The term DL/VA is misleading since the presence of ‘VA’ implies that DL/VA is related to a lung volume when in fact there is no volume involved. The use of the term DL/VA is probably a major contributor to the confusion surrounding this subject and for this reason it really should be banned and KCO substituted instead.]
I’ve written on this subject previously but based on several conversations I’ve had since then I don’t think the basic concepts are as clear as they should be.
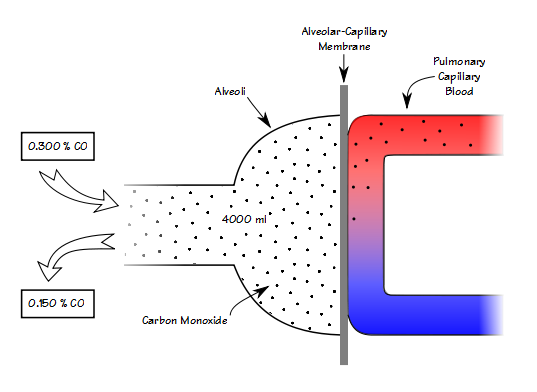
When you know the volume of the lung that you’re measuring, then knowing the breath-holding time and the inspired and expired carbon monoxide concentrations allows you to calculate DLCO in ml/min/mmHg. When you remove the volume of the lung from the equation however (which is what happens when you divide DLCO by VA), all you can measure is how quickly carbon monoxide decreases during breath-holding (KCO).
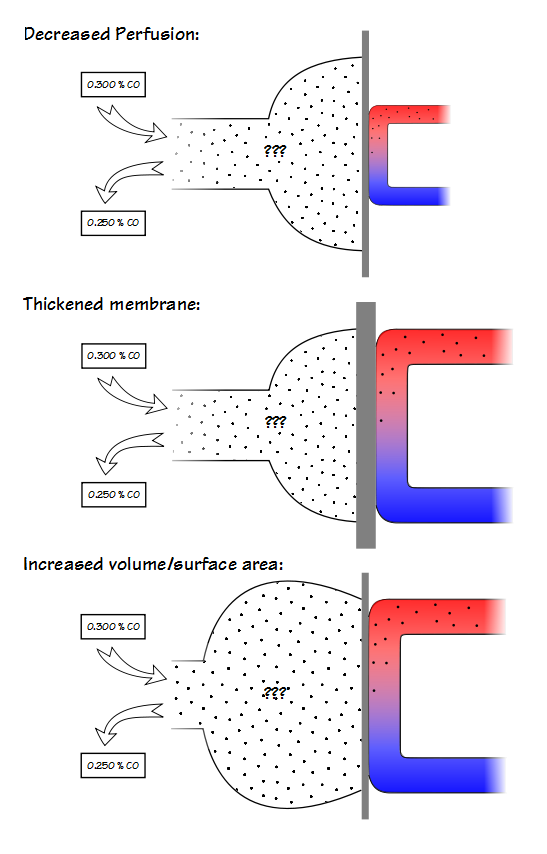
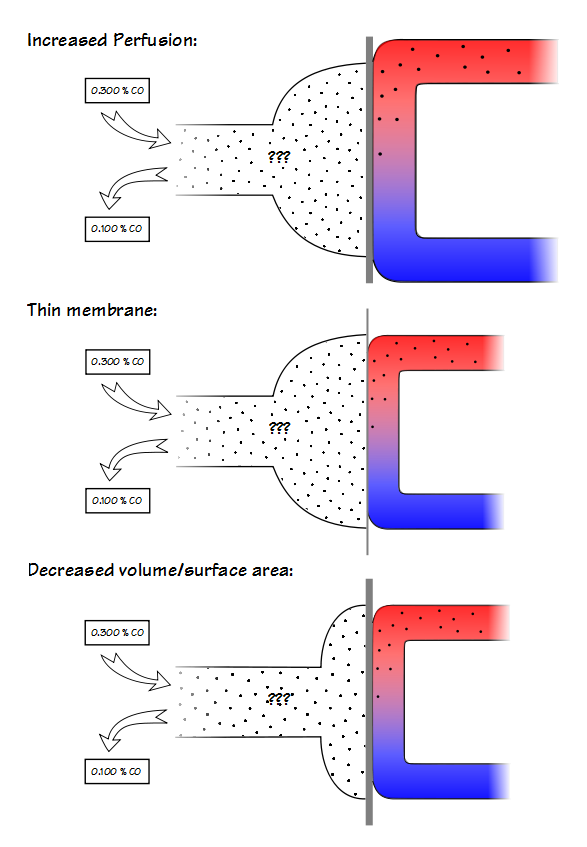
A low KCO can be due to decreased perfusion, a thickened alveolar-capillary membrane or an increased volume relative to the surface area.
A high KCO can be due to increased perfusion, a thinner alveolar-capillary membrane or by a decreased volume relative to the surface area. Because it is not possible to determine the reason for either a low or a high KCO this places a significant limitation on its usefulness.
This doesn’t mean that KCO cannot be used to interpret DLCO results, but its limitations need to recognized and the first of these is that the rules for using it are somewhat different for restrictive and obstructive lung diseases.
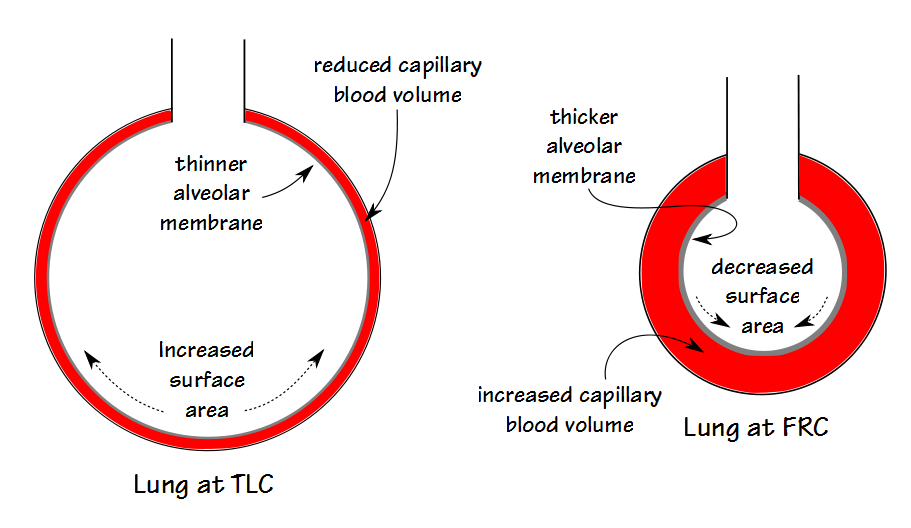
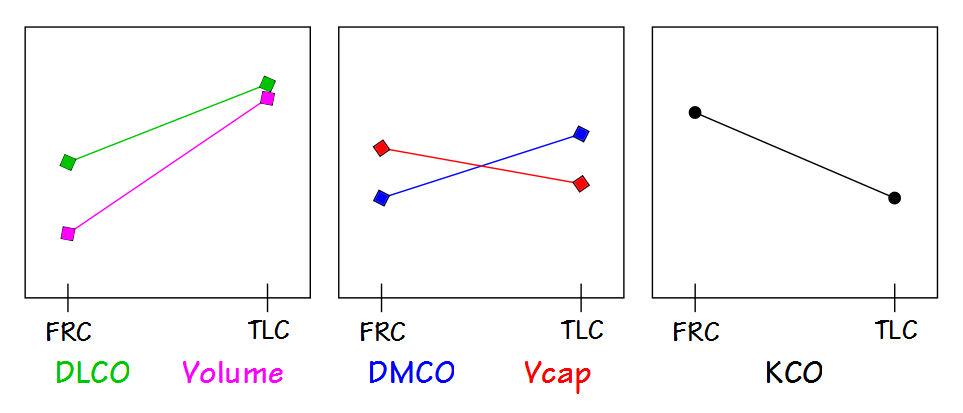
KCO is probably most useful for assessing restrictive lung diseases and much that has been written about KCO is in reference to them. The basic idea is that for an otherwise normal lung when the TLC is reduced DLCO also decreases, but does not decrease as fast as lung volume decreases. Part of the reason for this is that surface area does not decrease at the same rate as lung volume. This by itself would be a simple reason for KCO to increase as lung volume decreases but the complete picture is a bit more complicated.
The lung reaches its maximum surface area near TLC, and this is also when DLCO is at its maximum. At this time the alveolar membrane is stretched and at its thinnest which reduces the resistance to the transport of gases across the membrane. Simultaneously however, the pulmonary capillaries are also stretched and narrowed and the pulmonary capillary blood volume is at its lowest.
As lung volume decreases towards FRC, the alveolar membrane thickens which increases the resistance to gas transport but this is more than counterbalanced by an increase in pulmonary capillary blood volume. When factored in with a decrease in alveolar volume (which decreases the amount of CO available to be transferred), the rate at which CO decreases during breath-holding (for which KCO is an index) increases.
This means that when TLC is reduced but the lung tissue is normal, which would be the case with neuromuscular diseases or chest wall diseases, then KCO should be increased. There is no particular consensus about what constitutes an elevated KCO however, and although the amount of increase is somewhat dependent on the decrease in TLC, it is not predictable on an individual basis. For this reason, in my lab a KCO has to be at least 120 percent of predicted to be considered elevated (and I usually like it to be above 130% to be sufficiently confident).
Interstitial involvement in restrictive lung disease is often complicated and there can be multiple reasons for a decrease in DLCO. Scarring and a loss of elasticity causes the lung to become stiffer and harder to expand which decreases TLC. The alveolar membrane can thicken which increases the resistance to the transfer of gases. And probably most commonly there is destruction of the alveolar-capillary bed which decreases the pulmonary capillary blood volume and the functional alveolar-capillary surface area.
This means that when TLC is reduced and there is interstitial involvement, a normal KCO (in terms of percent predicted) is actually abnormal. A normal KCO can be taken as an indication that the interstitial disease is not as severe as it would considered to be if the KCO was reduced, but it is still abnormal.
KCO has a more limited value when assessing reduced DLCO results for obstructive lung disease. This is because the TLC is more or less normal in obstructive lung diseases and it is the DLCO, not the KCO, that is the primary way to differentiate between a primarily airways disease like asthma and one that also involves the lung tissue like emphysema. Strictly speaking, when TLC is normal and the DLCO is reduced, then KCO will also be reduced.
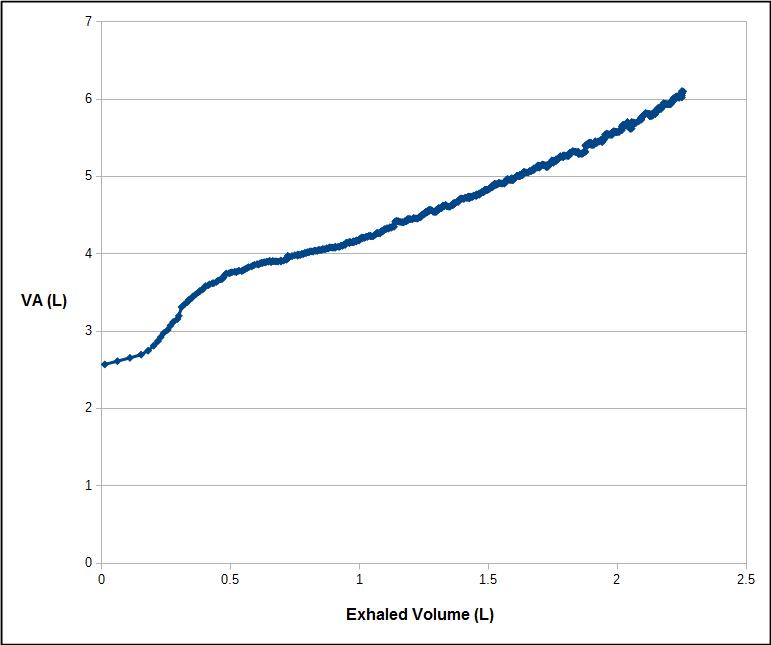
VA is a critical part of the DLCO equation however, so if VA is reduced because of a suboptimal inspired volume (i.e. inhalation to a lung volume below TLC), then DLCO may be underestimated. In this specific situation, if the lung itself is normal, then KCO should be elevated. When significant obstructive airways disease is present however, VA is often reduced because of ventilation inhomogeneity. This can be assessed by calculating the VA/TLC ratio from a DLCO test that was performed with acceptable quality (i.e. good inspired volume). A low VA/TLC ratio (less than 0.85) indicates that a significant ventilation inhomogeneity is likely present.
Does a low VA/TLC ratio make a difference when interpreting a low DLCO? Not really, but it brings up an interesting point and that is that the VA/TLC ratio indicates how much of the lung actually received the DLCO test gas mixture (at least for the purposes of the DLCO calculation). It also indicates that the DLCO result only applies to that fraction of the lung included within the VA/TLC ratio. Does that mean that the DLCO is underestimated when the VA/TLC ratio is low? The answer is maybe, but probably not by much.
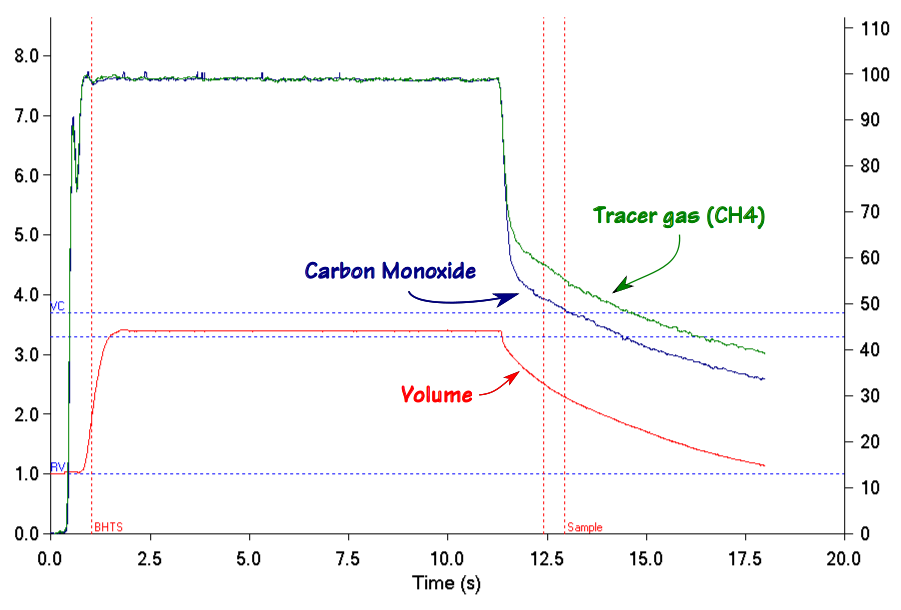
It is important to remember that the VA is measured from an expiratory sample that is optimized for measuring DLCO, not VA. When an individual with significant ventilation inhomogeneity exhales, the tracer gas (and carbon monoxide) concentrations are highest at the beginning of the alveolar plateau and decrease throughout the remaining exhalation.
The calculated VA therefore depends on where the tracer gas is measured during exhalation.
To one degree or another a reduced VA/TLC ratio is an artifact of the DLCO measurement requirements. At least one study has indicated that when the entire exhalation is used to calculate DLCO both healthy patients and those with COPD have a somewhat higher DLCO (although I have reservations about the study’s methodology). For the COPD patients at least part of the improvement was due to an increase in the measured VA. But the fact is that for regular DLCO testing any “missing” fraction isn’t measured so it really isn’t possible to say what contribution it would have made to the overall DLCO.
In general a low KCO is usually seen in:
- Interstitial disease
- Pulmonary hypertension
- Hepatopulmonary syndrome
- Emphysema
- Bronchiolitis
An elevated KCO is usually seen in:
- Pneumonectomy
- Neuromuscular disease
- Chest wall disease
- Alveolar hemorrhage
- Asthma
- Obesity
More than one study has cast doubt on the ability of KCO to add anything meaningful to the assessment of DLCO results. Despite this KCO has the potential be useful but it must be remembered that it is only a measurement of how fast carbon monoxide disappears during breath-holding. KCO can be reduced or elevated due to differences in alveolar membrane thickness, pulmonary blood volume as well as lung volume but it cannot differentiate between these factors, and the best that anyone can do is to make an educated guess. Realistically, the diagnosis of a reduced DLCO cannot proceed in isolation and a complete assessment requires spirometry and lung volume measurements as well.
In addition, there is an implicit assumption is that DLCO was normal to begin with. This is not necessarily true and as an example DLCO is often elevated in obesity and asthma for reasons that are unclear but may include better perfusion of the lung apices and increased perfusion of the airways. These individuals have an elevated KCO to begin with and this may skew any changes that occur due to the progression of restrictive or obstructive lung disease.
Finally DLCO tests have to meet the ATS/ERS quality standards for the KCO to be of any use and what we consider to be normal or abnormal about DLCO, VA and KCO depends a lot on the reference equations we select.
References:
Aduen JF et al. Retrospective study of pulmonary function tests in patients presenting with isolated reductions in single-breath diffusion capacity: Implications for the diagnosis of combined obstructive and restrictive lung diease. Mayo Clin Proc 2007; 82(1): 48-54.
Cotes JE, Chinn DJ, Miller MR. Lung Function. Physiology, measurement and application in medicine. 2006, Blackwell Publishing.
Frans A, Nemery B, Veriter C, Lacquet L, Francis C. Effect of alveolar volume on the interpretation of single-breath DLCO. Respir Med 1997; 91: 263-273.
Hansen JE. Pulmonary function testing and interpretation. 2011, Jaypee Brothers Medical Publishers, Ltd,
Horstman MJM, Health B, Mertens FW, Schotborg D, Hoogsteden HC, Stam H. Comparison of total-breath and single-breath diffusing capacity if health volunteers and COPD patients. Chest 2007; 131: 237-244.
Hughes JMB, Pride NB. In defence of the carbon monoxide transfer coefficient KCO (TL/VA). Eur Respir J. 2001; 17: 168-174.
Hughes JMB, Pride NB. Examination of the carbon monoxide diffusing capacity (DLCO) in relation to its KCO and VA components. Amer J Respir Crit Care Med 2012; 186(2): 132-139.
Johnson DC. Importance of adjusting carbon monoxide diffusing capacity (DLCO) and carbon monoxide transfer coefficient (KCO) for alveolar volume, Respir Med 2000; 94: 28-37.
Kaminsky DA, Whitman T, Callas PW. DLCO versus DLCO/VA as predictors of pulmonary gas exchange. Respir Med 2007; 101: 989-994.
Saydain Gm Beck KC, Decker PA, Cowl CT, Scanlon PD, Clinical significance of elevated diffusing capacity. Chest 2004; 125: 446-452.
van der Lee I, Zanen P, van den Bosch JMM, Lammers JWJ. Pattern of diffusion disturbance related to clinical diagnosis: The KCO has no diagnostic value next to the DLCO. Respir Med 2006; 100: 101-109.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

Hi Richard – I have been ejoying your posts for a while now and have forwarded on the link to my colleagues here at Monash. (I am the senior scientist in he pulmonary lab). I have had many arguments about KCO over the years and have tried my hardest to stop physicians using the phrase “TLCO is normal when corrected for lung volume” – yuk. Here at Monash we use KCO as a way to assess what might be the cause of reduction in TLCO. If KCO is low with a normal VA, then parenchymal/vascular dysfunction is the most likely cause of reduced TLCO. If KCO is low with a low VA, then we also have to consider the possibility of reduction in alveolar volume (for whatever reason) in conjunction with parenchymal changes. I agree with you that a supranormal KCO (120%) is highly suggestive of a true volume effect. A deliberately submaximal inspiration in a normal lung will show a very high KCO. Finally I always try to explain to the trainee physicians that VA is simply the volume of lung that that has been exposed to the test gas and may not reflect the true alveolar volume.
regards
Paul
Thank you for your blog
Im still not very clear about the difference between DLCO – Kco
Could you please make a quick table to compare between DLCO and KCO to make it easier for us to understand the difference between both of them ( i.e definition, factors they depend on, condition which make them high / low , etc )
A table wouldn’t simplify this. It would actually be more complicated because of the if-then’s and except-when’s.
DLCO is best thought of as a measurement of the functional gas exchange surface area of the lung. It’s reduced in diseases as different as COPD and Pulmonary Fibrosis, but in a sense for the same reason and that is a loss of functional surface area. DLCO is dependent on the adequacy of alveolar ventilation, the alveolar-capillary membrane resistance (its thickness) and the availability of hemoglobin in the blood. A disruption of any of those factors reduces DLCO. Increases in DLCO are less common and appear to be mostly due to an increase in blood volume and/or cardiac output.
KCO is only a measurement of the rate at which CO disappears during breath-holding (i.e. a change in concentration between inhaled and exhaled CO). DLCO is the volume of CO that is absorbed during breath-holding. In the normal lung KCO tends to increase at lung volumes below TLC because of a decrease in alveolar volume (less CO to transfer per unit of volume) and an increase in capillary blood volume per unit of alveolar volume. However, at the same time despite the fact that KCO rises at lower lung volumes (i.e. the rate at which the concentration of CO disappears increases) the DLCO (the actual volume of CO absorbed) decreases. KCO has an extremely limited clinical utility and frankly if it wasn’t reported at all there would be little to no difference in how DLCO results would be interpreted.
– Richard
Hi Richard. Thank you for your informative PFT Blog! I wonder this: During INSPIRATION (at TLC) I’ve learnt that the lung blood volume (LBV) increases due to a more negative intrathoracic pressure -> increased venous return to the RV -> increased lung filling AND reduced venous return to the LV -> reduced CO -> baroreceptor reflex -> reflex takycardia (to prevent drop in blood pressure).
Your statement above: “Near TLC… Simultaneously however, the pulmonary capillaries are also stretched and narrowed and the pulmonary capillary blood volume is at its lowest” -doesn’t really comply with this. You also state that at FRC (during expiration) “..an increase in pulmonary capillary blood volume”.. I’m getting a little confused. Would be great to hear your thoughts on this!
Markus –
The pressure in the alveoli and pulmonary capillaries changes throughout the breathing cycle. During inspiration the amount of negative pressure inside the lung will be the product of inspiratory flow and airway resistance. Inspiratory flow however, decreases to zero at TLC and at that time the pressure inside the alveoli and pulmonary capillaries will be equivalent to atmospheric pressure and the capillary blood volume will be constrained by the fact that the pulmonary vasculature is being stretched and narrowed due to the elevated volume of the lung. At end-exhalation (FRC), again the alveoli and pulmonary capillaries are at atmospheric pressure but the capillaries are mechanically relaxed and able to hold a greater amount of blood.
In particular, consider also the ratio between alveolar volume and pulmonary capillary volume at TLC and FRC. At TLC alveolar volume is at its greatest but pulmonary capillary blood volume is at least somewhat constrained. At FRC alveolar volume is reduced but capillary blood volume is probably at its greatest. This is why DL/VA (KCO!!! which is the rate at which CO disappears and nothing more) is lowest at TLC and highest near FRC. DLCO however, is highest at TLC and lowest at FRC and this is because it is primarily a measurement of functional gas exchange surface area (and not the rate at which CO disappears).
During the breath-hold period of the single-breath diffusing capacity maneuver the mouthpiece is usually closed by a shutter or valve. Many (most?) patients will relax against the valve and the pressure in the alveoli and pulmonary capillaries will actually rise slightly at this time due to the elastic recoil of the lung. This elevated pressure tends to reduce the capillary blood volume a bit further. An extreme example of this would be if the patient performed a Valsalva maneuver (attempted to exhale forcefully against the closed mouthpiece) which would significantly decrease capillary blood volume. If, on the other hand, the patient performs a Muller maneuver (attempts to inhale forcefully against the closed mouthpiece) this will cause negative pressure inside the lung and will increase the capillary blood volume. The ATS/ERS standards for DLCO of course contraindicate either Valsalva or Muller maneuvers during the breath-hold period because they do affect the pulmonary capillary blood volume (and therefore the DLCO).
Regards, Richard
Hi, Richard. I am one of the fans of your blog. I work as a cardiologist in Hokkido Univ Hospital, JAPAN. Pulmonary hypertension is my field and I have been curious why KCO/DLCO is severely low in pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis. Because, in both disease entities, pulmonary congestion is present and then DLCO and KCO should be increased. I understand some factors that decrease DLCO and KCO are present, such as a reduced cardiac output and pulmonary arterial disease, in such cases but even so it is not understandable that DLCO and KCO are reduces in such a critical degree (<30% in some cases). Thank you so much for your help in this issue!
Dr. Tsujino –
This is where I get to say I’m a technologist not a diagnostician but I do think about issues like this fairly often so this is my take on these disorders:
Pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis are both forms of pulmonary hypertension with a progressive occlusion of the pulmonary circulation. Hemangiomatosis is accompanied with a proliferation of pulmonary capillaries and fibrosis while veno-occlusive disease isn’t. DLCO is primarily a measurement of the functional alveolar-capillary surface area, so the simple answer is that if there is an increase in pulmonary capillary blood volume in these disorders it is occurring in poorly ventilated areas and that overall there is low V/Q. A more complex answer is that because vascular resistance increases, cardiac output will be diverted to the pulmonary circulation with the lowest resistance. This could lead to a couple additional issues; one, that the “depth” of the pulmonary capillary around ventilated alveoli is increased and this may prevent the diffusion of oxygen to the blood furthest away from the alveolar membrane. Two, this would also lead to an increase in the velocity of blood flow and oxygen may not have sufficient time to diffuse completely because of the decrease in pulmonary capillary residence time.
These disorders may also cause a thickening of the alveolar-capillary membrane (i.e. decreased DMCO). At least one study appears to confirm this in PAH (Farha S, et al. “Loss of alveolar membrane diffusing capacity and pulmonary capillary blood volume in pulmonary arterial hypertension”. Respiratory Research 2013, 14:6), although I have some concerns about the substitution of DLNO for DMCO.
Finally, pulmonary hypertension is often accompanied by a reduced lung volume and airway obstruction. I don’t know if this is the case for pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis since they are both rare and under-diagnosed. If so however, then for what are more or less mechanical reasons these factors could also contribute to a decrease in DLCO.
Regards, Richard
Dear Richard,
I appreciate your comments. It was very helpful!
But I still have two questions.
1. To me, the simple and more complex answeres in your comments were reasonable mechanisms for hypoxemia, but not necessarily for low KCO. I am not sure whether my question is reasonable or not…
2. I feel that hypoxemia is caused by the presence of low V/Q area rather than high V/Q. In the low V/Q area, Hb will have difficulties in getting oxygen due to a relatively limited ventilated area. In contrast, as to KCO, I suppose that it is caused predominantly by the presence of high V/Q area rather than low V/Q, because inhaled CO may have more difficulties in reaching Hb in the (too much) high V/Q area rather than in low V/Q area. However, I am not sure if my thoughts are correct because in patients with PVOD/PCH KCO is severely reduced in most cases…
Thank you so much again for letting me share my thoughts.
Sincerely yours,
Ichizo
Ichizo –
I may be missing something but I’m not quite sure what you expect KCO to be. Your original comment implied that DLCO and KCO were reduced by similar amounts. The diagnostic value of KCO is pretty much limited to restrictive lung defects and can only be used to differentiate between intrinsic and extrinsic causes for a reduced DLCO. By itself KCO is nothing more the rate at which CO disappears during breath-holding and the reduced DLCO already says there’s a diffusion defect. The fact that the KCO is similarly reduced to DLCO indicates that the cause is intrinsic but that’s already known from the etiology of the disorders.
A reduced KCO cannot indicate the site or scale of the diffusion defect. As an example, if a patient had a pulmonary emboli that blocked blood flow to one lung then DLCO would be about 50% of predicted, but in these circumstances KCO would also be 50% of predicted. The cause of the diffusion defect is a large scale V-Q mismatch but that doesn’t look any different from somebody with PVOD/PCH with a DLCO and KCO that were 50% of predicted and where the V-Q mismatch is occurring on a much smaller scale.
You suggest that both low V/high Q and high V/low Q areas are residing in these patient’s lungs. Given the fact that these disorders affect the pulmonary circulation I wouldn’t be surprised to see a wide degree of Q heterogeneity but I’m not certain I see a cause for a high degree of V heterogeneity. PAH can cause lung restriction but from what I know the effect is fairly homogeneous. Since a low Q regardless of V can explain both hypoxia and a low DLCO I’m not sure there needs to be a separate mechanism.
There is also another minor point that may be skewing the percent predicted DLCO and KCO somewhat. In my lab’s software predicted KCO is derived from [predicted DLCO]/[Predicted TLC-deadspace] but the DLCO and TLC come from entirely different studies and different populations. If we chose different DLCO and TLC reference equations we’d have a different predicted KCO. [Note: looking at the DLCO and TLC reference equations I have on hand, for a 50 y/0 175 cm male predicted TLC ranges 5.20 to 7.46 and predicted DLCO ranges from 24.5 to 37.1. Predicted KCO derived from these values would range from 3.28 to 7.13!] There are a few DLCO reference equations (most notably GLI) that have separate reference equations for DLCO and KCO. If your predicted KCO is derived from separate population studies I would wonder what effect re-calculating percent predicted DLCO and KCO using reference equations from a single study would have on your data and your expectations.
Good discussion.
Regards, Richard
Dear Richard,
Thank you so much again for your comments.
They helped me a lot!
I wish I can discuss again with you when I have more questions.
Best,
ichizo