Turbine spirometers have been around in one form or another for well over a hundred years. The accuracy of the early versions of this type of spirometer was poor, partly because of the turbine designs weren’t terribly efficient and partly because these devices were mechanical in nature and the gear trains or other mechanical linkages added a lot of friction and resistance.
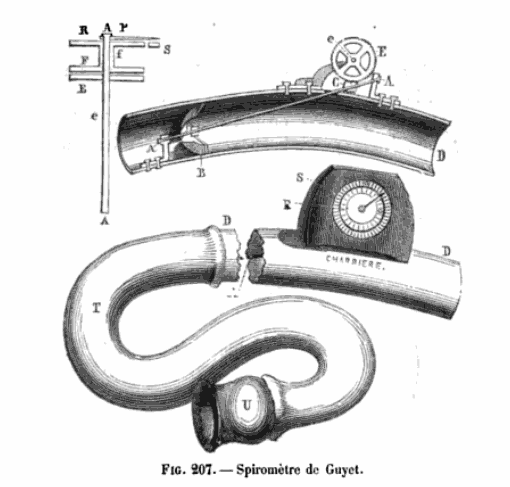
From: Nouveaux éléments de pathologie générale, de séméiologie et de diagnostic. by Eugène Bouchut, 1875, page 865. ]
The first electronic turbine spirometer was the Marion Labs Spirostat which came to market in the early 1970’s. It used a disposable in-line turbine where the turbine blades were directly in the stream of inspiratory and expiratory flow and rotated accordingly. There was an optical pickup (a light beam passing through a hole in the turbine) and the rotations were converted to inspiratory and expiratory volumes. The passageways through the Spirostat’s turbine sensor were quite narrow and the resistance to flow was high. The turbine also had a fair amount of mass, was perceptibly slow to start moving and slow to stop and would not have met the current ATS/ERS standards.
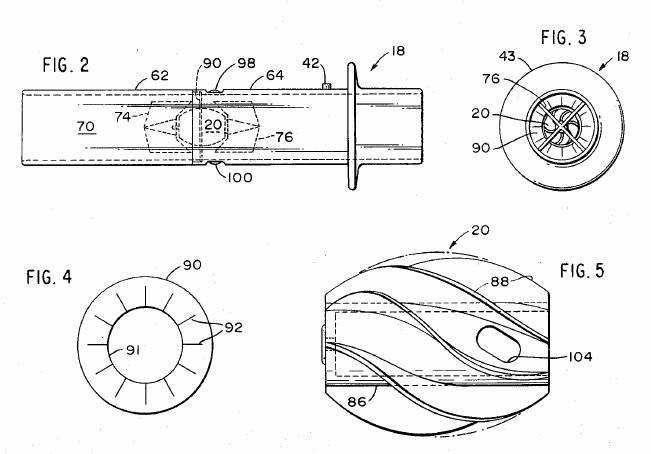
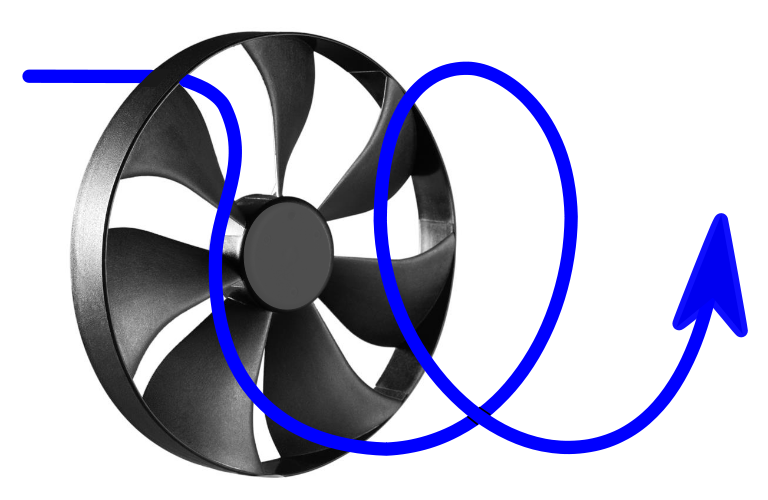
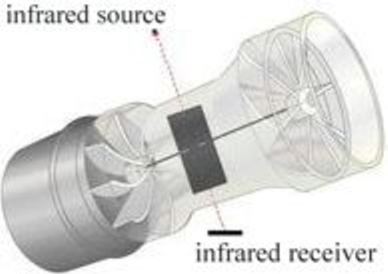
During the early 1980’s a turbine spirometer was developed and marketed that used swirl or deflector end-plates (the equivalent of fixed fan blades) to cause airflow to rotate helically through the body of the sensor.
This rotating airflow in turn causes a flat vane mounted vertically in the air stream to rotate. A pair of optical or Hall effect sensors count rotations and enable the direction of flow to be detected. This is the basis for most of the current turbine spirometers.
Rotating vane turbine sensors are primarily volumetric. This means is that across a relatively wide range of flow rates, each rotation of the vane is directly linked to the volume of gas flowing through the sensor. Even so, it is the differential pressure of the helical gas flow that causes a vane to rotate. The factors that affect the accuracy and sensitivity of any given turbine sensor are inertia, friction, the area of the vane and how effectively the deflector/swirl end-plates convert linear gas momentum into angular momentum.
The concerns I’ve heard most frequently voiced about turbine spirometers is their accuracy at low flow rates and how well they respond to rapid changes in flow rates.
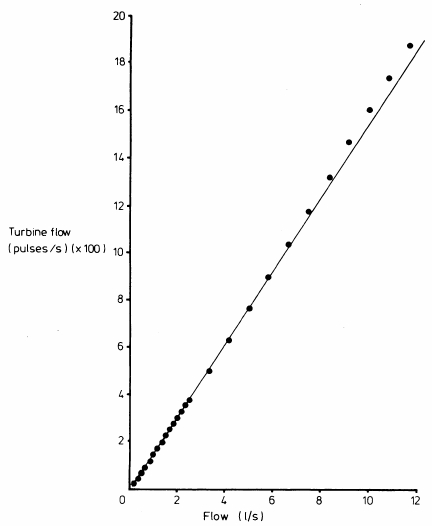
For a variety of reasons turbine spirometers would be expected to be least sensitive to low flow rates. The ATS/ERS specifications on spirometry state that the end-of-test indication is a flow rate below 0.025 L/sec. The ability to meet this specification is not usually detailed for any spirometer regardless of which measurement technology it uses, so whether turbine spirometers are any worse (or any better) at measuring a flow rate this low is difficult to determine. I will note that the specifications found in the advertising brochures for several turbine spirometers indicate a flow accuracy that is well above this value (for example +/- 200 ml/sec) and that some of the cheapest turbine spirometers do not claim to measure FVC, but FEV6 instead (or in some cases only FEV1 and PEF). This is verified to some extent by one study which noted that a turbine spirometer significantly underestimated volume at low flow rates (< 0.5 L/sec). On the other hand another comparison between precision flow meters and a turbine sensor appears to show larger discrepancies at higher flow rates than at lower so this isn’t quite as clear as it should be.
There have been numerous comparison studies between turbine and more conventional spirometers. Although the majority of these studies showed that turbine spirometers met the ATS/ERS guidelines they also showed that FVC tended to be underestimated somewhat and that the FEV1/FVC ratio tended to be slightly overestimated. This appears to a problem specific to turbine spirometers since similar findings were shown across a half dozen studies for at least three different brands of turbine spirometers. It has been suggested that an insensitivity to low flow rates would cause spirometers to terminate spirometry efforts early and thereby underestimate FVC but since none of the comparative studies tracked expiratory times this is just speculation. There were also significant differences in methodologies between these studies and overall there is no overwhelming reason to believe that turbine spirometers are significantly less accurate than any other measurement technique.
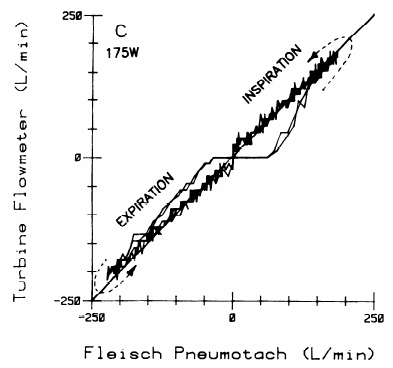
An early study of a turbine flowmeter by Yeh et al indicated the presence of significant inertia which caused “lag-before-start” and “spin-after-stop” effects.
This finding has formed the basis of numerous criticisms of turbine spirometers but its validity is open to question, most particularly since the study did not describe the turbine flow meter’s mode of operation. At the time of the study there were many different turbine designs which included both the in-line as well as the deflection end-plate and vane types. The vane used in most present-day turbine spirometers has a very low mass and a relatively large surface area which means they are likely to respond quickly to any changes in flow rate. Quick does not mean instantaneous however, and although it may be small all turbines have some lag but it is unlikely to be anywhere near the degree noted in Yeh et al’s study.
One interesting point is that most turbine spirometers produce one “pulse” for every half-rotation and that each rotation is related to a specific volume of gas. At high flow rates, the pulse count rate is also high. One manufacturer indicated that their device had 144 pulses per liter (which works out to 6.9 ml/pulse). The current ATS/ERS recommendation is that spirometers should have a sampling rate of 100 hz. Even at modest flow rates (> 0.69 L/sec), the number of pulses/second is above 100 hz, but at lower flow rates the pulse count rate drops below 100 hz. At terminal flow rates (0.025 L/sec) the pulse count rate is only 3.6 hz. To some extent this means that turbine flow meters do not meet ATS/ERS standards but in reality it is a reflection of how they operate.
One of the primary selling points of turbine spirometers is that they do not require frequent calibrations. This appears to relatively true and was verified in at least one two-year longitudinal study. For this reason turbine spirometers are probably well suited to portable or field applications where calibrations are infrequent or non-existent and where accurate trends may be more important than absolute accuracy (personal use or clinical trials, for example). The same characteristics may well apply to office spirometry but since this seems to be an area that’s on the dividing line between using spirometry for monitoring and using it for diagnostics I am uncomfortable saying that regular calibration is not necessary. It should also be remembered that turbine sensors are mechanical in nature and can be irreversibly damaged by a drop or fall and this also makes me uncomfortable saying that regular calibration of some kind for any turbine spirometer is not necessary.
Other reasons to select turbine spirometers would be that they are relatively insensitive to gas composition, humidity and altitude. One study did find a sensitivity to temperature but that may be limited to the specific model being tested.
No flow sensor is perfect. Although it may be small, turbine lag, and the circumstances under which it occurs (low flow rates, high flow rates, changing flow rates) as well as the overall linearity of a turbine sensor requires software correction. How much and what kind of a correction is performed for a given spirometer is proprietary information however, and details are not shared with end-users. Strictly speaking, this is not particularly different for turbine spirometer manufacturers than it is for the manufacturers of pneumotach, mass flow, pitot, variable-orifice and ultrasonic spirometers and given the amount of resources each manufacturer has devoted to developing a particular flow sensor it’s also mostly understandable.
But even though turbine sensors appear to be relatively simple details like the aerodynamics of the helical air flow are probably quite complex. Despite an extensive search however, I’ve been unable to find any study that explored the physics of their operation (any doctoral candidates out there looking for a thesis topic?). The lack of information about turbine spirometer characteristics leaves me in something of a quandary and I would be more comfortable discussing them if they were better studied and understood.
Turbine spirometers come in a variety of configurations. Some use disposable sensors and some don’t. Some come with jeweled bearings and some don’t. Most come in a horizontal orientation but at least one doesn’t. Although there is some equivocal evidence they are insensitive to low flows all claim to meet the ATS/ERS standards and there is no overwhelming evidence that they don’t. The bottom line is that a spirometer should be chosen based not on whether it does (or doesn’t) use a turbine, but on whether the software used to perform, store, manage and report tests meets your needs.
References:
Bongers T, O’Driscoll BR. Effects of equipment and technique on peak flow measurements. BMC Pulm Med 2006; 6: 14.
Caras WE, Winter MG, Dillard T, Reasor T. Performance comparison of the hand-held MicroPlus portable spirometer and the SensorMedics Vmax22 diagnostic spirometer. Respir Care 1999; 44(12): 1465-1473.
Chowienczyk PJ, Lawson CP. Pocket-sized device for measuring forced expiratory volume in one second and forced vital capacity. Brit Med J 1982; 285: 15-17.
Degryse J, Buffels J, Van Dijck Y, Decramer M, Nemery B. Accuracy of office spirometry performed by trained primary-care physicians using the MIR spirobank hand-held spirometer. Respiration 2012; 83: 543-552.
Dirksen A, Madsen F, Pedersen OF, Vedel AM, Kok-Jensen A. Long term performance of a hand held spirometer. Thorax 1996; 51: 973-976.
Godschalk I, Brackel HJL, Peters JCK, Bogaards JM. Assessment of accuracy of applicability of a portable electronic diary card spirometer for asthma treatment. Respir Med 1996; 90: 619-622.
Gunawardena KA, Houston K, Smith AP. Evaluation of the turbine pocket spirometer. Thorax 1987; 42: 689-693.
Jones KP, Mullee MA. Lung function measurement in general practice: a comparison of the Escort spirometer with the Micromed turbine spirometer and the mini-Wright peak flow meter. Respir Med 1995; 89: 657-663.
Liistro G, Vanwelde C, Vincken W, Vandevoorde J, Verleden G, Buffels J. Technical and functional assessment of 10 office spirometers. Chest 2006; 130: 657-665.
Paul KP, Schultz T. Evaluation of a pocket-sized turbine spirometer for clinical use with children. Respir Med 1997; 91: 369-372.
Pederson OF, Miller MR, Sigsgaard T, Tidley M, Harding RM. Portable peak flow meters: physical characteristics, influence of temperature, altitude and humidity. Eur Respir J 1994; 7: 991-997.
Pollard AJ, Mason NP, Barry PW, Pollard RC, Collier DJ, Fraser RS, Miller MR, Milledge JS. Effect of altitude on spirometric parameters and performance of peak flow meters. Thorax 1996; 51: 175-178.
Yeh MP, Adams TD, Gardner RM, Yanowitz FG. Turbine flowmeter vs. Fleisch pneumotachometer: a comparative study for exercise testing. J Appl Physiol 1987; 63(3): 1289-1295.
Wild LB, Dias AS, Fischer GB, Rech DR. Pulmonary function tests in asthmatic children and adolescents: Comparison between a microspirometer and a conventional spirometer. J Bras Pneumol 2005; 31(2): 97-102.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

In the past I have sold KoKo and currently sell Vitalograph, Morgan Scientific and MIR. I did a personal side by side comparison of test results on FVC, FEV1.0 and 25-75 on myself on the pneumotachs used with KoKo, Vitalograph/Morgan Scientific and the MIR MiniSpir. Everything was surprisingly consistent as far as accuracy. The big difference is software as far as features. This is my 34th year selling PFT equipment.
What people need is to be TRAINED PROPERLY!
My hospital has switched to a portable turbine spirometer with disposable turbines set in paper mouthpieces.
The first time I used it was when I went to the ER because I was doing badly and needed to start antibiotics ASAP. I blew a whopping 32%, which is 4% above my baseline. I immediately knew that this machine was crap. After 20 days of IVs, I asked to be tested on the large spirometry machines in the lab instead. Surprise surprise, I blew 28%, which is my baseline. The difference was reflected in the raw values too. So it does not have anything to do with either the algorithm used or the other information that was entered.
When I told my doctor about it, she gave me the usual spiel about how this is within normal variation, that people can vary this much within a day, yada yada… no. First, I blow very consistantly. Never, ever has it happened that I blew below what I blew before an IV treatment. Ever. Whenever there was a variation, it was upward and never above 1%. Second, I have not blown 32% in… 6+ years? I have changed nothing to my routine and my IV treatments have not changed in the last 2.5 years. So this sudden increase comes out of nowhere, happens to only happen on this machine, but the machine is not the cause? Thirdly, when you have a low lung function like that, 2-4% is a huge difference. You feel it in how much you can breath. If I had gained 4%LF I think I would have noticed.
I mean how much quality can go in disposable turbines? How accurate can they be? I was told the machine was calibrated using a syringe… but this is worthless to determine the performance in a real scenario.
So in my own n=1 study, turbine spirometers are trash. The hospital used to have a smaller machine that had metal leads in it. I don’t know what technology it used, but the results were comparable to the large spirometry machines in the lab.
Unhappy –
I can’t speak from my own experience since my lab has never used disposable sensors, regardless of which technology was used (turbine or pneumotach) but I’ve always been concerned about the fact that they cannot be calibrated (they can be checked with a 3 liter syringe but usually cannot be calibrated). I will say however, that I would have expected that if there was a problem with a disposable turbine sensor it would read low, not high. For this reason I suspect the difference may have to do with other things and in particular I suspect that the way in which the different systems correct for exhaled air temperature plays a significant role.
The fact is that although spirometry test systems are always marketed as meeting the ATS/ERS standards most PFT labs have no ability to verify this. In particular there is a significant difference in calibrating a spirometer with a 3 liter syringe using room air and in measuring exhaled air that is at body temperature and saturated with water vapor. I have noticed somewhat systematic differences in flow and volume measurements when pneumotach, hot wire anemometer, turbine and rolling-seal volume-displacement spirometers are compared on the same person. These differences however, are usually within acceptable limits depending on which part of the ATS/ERS standards you read.
When equipment in a PFT lab or doctor’s office (or whatever) needs to be replaced there is often a discrepancy between older and newer results. Sometimes this is because of differences in measurement technology. Sometimes it’s because of differences in software. Sometimes it’s because of changes in reference equations. We rarely have the time or the resources to do anything other than accept the differences and move forward. I’ll also point out that new equipment is often bought by hospitals based on financial considerations and without any input from those who use the equipment, so we’re often stuck without any recourse.
Given your situation I understand your frustration with getting consistent spirometry results. What you’re not going to want to hear is that it’s possible that the turbine spirometer is more accurate than the old portable system or the PFT lab system. Consistency is not the same as accuracy. For your peace of mind I’d suggest you request that your testing be done in the PFT lab because at least until such time as the PFT lab has to replace equipment you will get the consistency you’re looking for.
Regards, Richard