As workload increases during a progressive cardiopulmonary exercise test (CPET) there comes a point at which the amount of oxygen delivered to the exercising muscle is no longer able to meet its needs. This is the point at which lactic acid begins to accumulate, CO2 production increases and is the accepted definition of the Anaerobic Threshold (AT). The “gold” standard for determining AT is lactic acid measurements but these require sampling blood at regular intervals throughout the CPET. AT is far more commonly determined from respiratory parameters.
Recently I had the opportunity to observe a CPET performed at another PFT Lab. Following the CPET I saw that there was some difficulty in determining the AT. Part of the reason for this is that the staff had only been shown the V-slope method and weren’t aware that there are several alternative approaches.
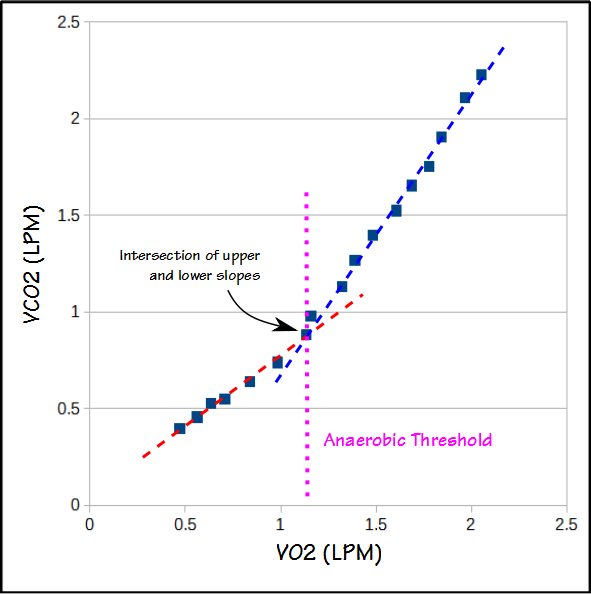
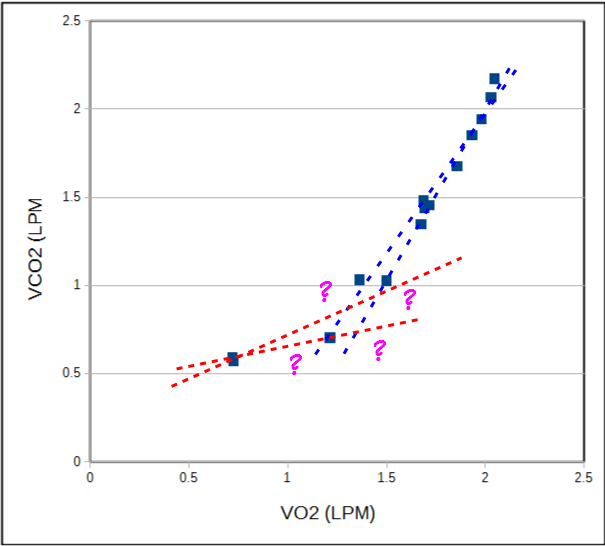
The V-slope method graphs VCO2 versus VO2. The slope of relationship between VCO2 and VO2 both above and below AT is relatively linear, but changes at AT.
CPET data is often “noisy” however, and it can be difficult to know which data points should be included in the upper and lower slopes.
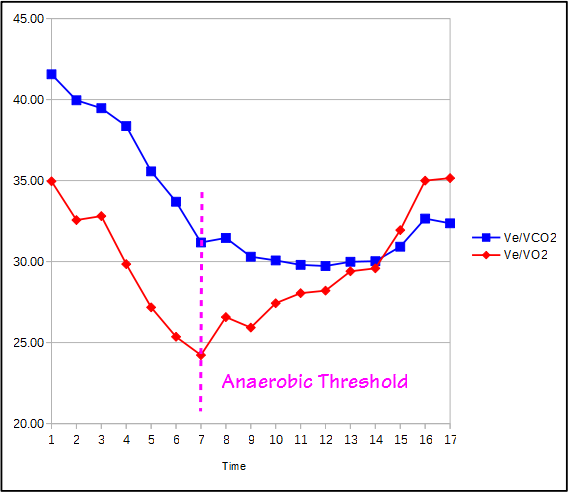
Another approach is to use the ventilatory equivalents for O2 and CO2 (Ve/VO2 and Ve/VCO2). When these two values are plotted against time, the point at which Ve/VO2 reaches a minimum and then begins to rise without a corresponding increase in Ve/VCO2 is the AT.
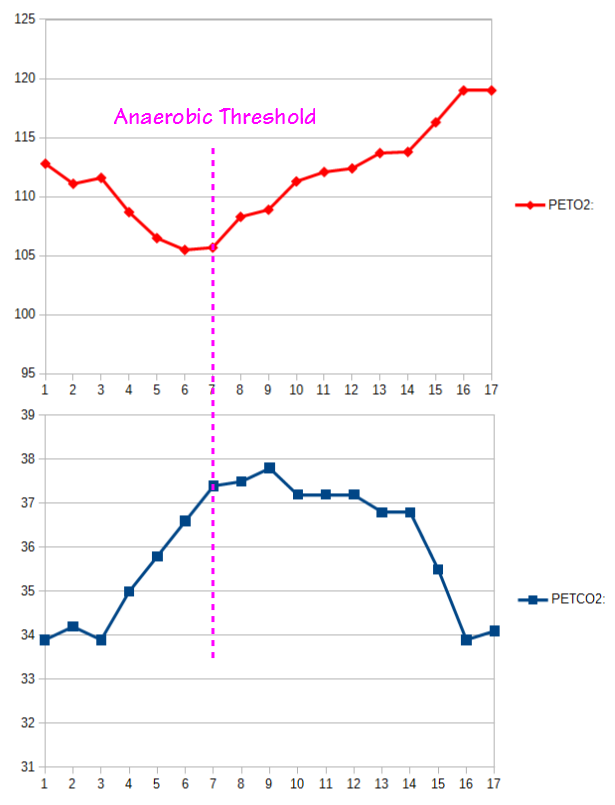
A similar approach is to use the PETO2 and PETCO2. When these two values are plotted against time, the point at which the PETO2 reaches a minimum and then begins to rise without a corresponding increase in PETCO2 is also the AT.
There are a couple other secondary techniques. Ve, VCO2 and Rq also rise along with the increasing workload and the VO2 at which the rate of increase in Ve, VCO2 or Rq suddenly increases should coincide with AT. These changes are often quite subtle however and hard to detect.
The ATS/ACCP and AHA guidelines for cardiopulmonary exercise testing do not recommend one technique over another and in fact state “there appears to be no clear advantage of any one noninvasive method for AT determination”. Depending on the patient, AT may be clearer in one method over another, but once it has been detected it by one method it should always be verified by the other methods.
Regardless of how “evident” an AT may appear to be, it should also get some kind of an overall reality check. As an example, a patient with a low VO2 at AT should not be able to reach a high maximum VO2. It should also be remembered that not all patients reach AT and that not all patients who have a normal exercise capacity have an identifiable AT. For these reasons there is no particular “shame” in not being able to identify an AT.
Some test systems will attempt to automatically determine AT, but this occurs with varying degrees of accuracy. I’ve seen some rather wild computer-generated AT’s so it is always important to understand the different methods for determining AT and to be able to verify them manually.
Anaerobic threshold is usually reported as the oxygen consumption (VO2) at which it occurs, and most often as the percent predicted of the maximum VO2. The VO2 at AT says a lot about cardiovascular fitness. The higher the VO2 at AT, the more fit an individual is. When the percent predicted VO2 at AT is below a certain threshold however, this is an indication that there is an abnormal limitation in the oxygen supply to the muscles. This can be due to a reduced cardiac output, vascular disease or even to mitochondrial myopathies.
| Male: | Female: | |||
| Age: | Mean: | LLN: | Mean: | LLN: |
| 20 | 53 | 42 | 52 | 41 |
| 30 | 54 | 43 | 55 | 44 |
| 40 | 55 | 44 | 58 | 47 |
| 50 | 56 | 45 | 60 | 49 |
| 60 | 57 | 46 | 63 | 52 |
| 70 | 58 | 47 | 65 | 54 |
Anaerobic threshold will vary in a given individual depending on what testing mode is used. Arm ergometry produces the lowest VO2 at AT. Treadmill testing produces the highest VO2 at AT with cycle ergometry between 5% and 11% lower than treadmill. For this reason it is important to select a predicted VO2 reference equation that takes the testing mode into consideration.
Not only is the VO2 at AT an important part of CPET interpretation, but the minute ventilation at AT can be informative. When a CPET is submaximal it can be difficult to determine if a patient has a pulmonary mechanical limitation. If the patient has achieved AT however, the minute ventilation at AT can help determine whether this would have occurred. Specifically, a minute ventilation at AT that is greater than 42% of the predicted maximum indicates the patient likely has a pulmonary mechanical limitation.
Maximum oxygen consumption has been the primary tool of surgical risk and general mortality assessments. VO2 max will likely be reduced when a CPET is submaximal and a CPET can be submaximal due to musculoskeletal limitations, patient safety concerns (EKG and blood pressure changes) or poor patient motivation. An individual can have a submaximal CPET and still attain anaerobic threshold. When patients with heart failure were studied, investigators found that those with a VO2 at AT less than 11 ml/kg/min showed an elevated mortality risk and that this was more significant than a low peak VO2. Similarly a survey of patients with post-operative complications and mortality showed that individuals with VO2 at AT less than 50% of predicted or 11 ml/kg/min had an elevated risk. VO2 at AT can also be used to assess which cardiac class a patient belongs to.
| Class: | Severity: | VO2 at AT: |
| A | Mild to none | > 14 |
| B | Mild to moderate | 11 to 14 |
| C | Moderate to severe | 8 to 11 |
| D | Severe | 5 to 8 |
Anaerobic threshold occurs as increases in workload surpass the ability to provide oxygen to the exercising muscles. The VO2 at which it occurs is a reflection of cardiovascular fitness and is a crucial part of interpreting CPET results. Accurate detection of the AT is therefore important and there are a variety of methods for doing this. The only reason that one method may be superior the others is that the data signaling AT may be more evident for the patient being evaluated. Regardless of which method is initially used to detect AT, AT should be verified across all methods.
References:
ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Resp Crit Care Med 2003; 167: 211-277.
Balady GJ, et al. Clinician’s guide to Cardiopulmonary exercise testing in Adults. Circulation 2010; 122: 191-225.
Caiozzo VJ, Davis JA, Ellis JF, Azus JL, Vandagriff R, Prietto CA, McMaster WC. A comparison of gas exchange indices used to detect the anaerobic threshold. J Appl Physiol 1982; 53(5): 1184-1189.
Gitt AK, Wasserman K, Kilkowski C, Kleeman T, Kilkowski A, Bangert M, Schneider S, Schwarz A, Senges J. Exercise anaerobic threshold and ventilatory efficiency identify heart failure patients for high risk of early deat. Circulation 2002; 106: 3079-3084.
Medoff BD, Oelberg DA, Kanarek DJ, Systrom DM. Breathing reserve at the lactate threshold to differentiate a pulmonary mechanical from a cardiovascular limitation to exercise. Chest 1998; 113: 913-918.
Older P. Anaerobic threshold, is it a magic number to determine fitness for surgery? Perioperative Medicine 2013: 2:2
Smith TB, Stonell C, Purkayastha S, Paraskevas P. Cardiopulmonary exercise testing as a risk assessment method in non cardio-pulmonary surgery: A systematic review. Anaesthesia 2009; 64: 883-893.
Sue DY, Wasserman K, Moricca RB, Casaburi R. Metabolic acidosis during exercise in patients with chronic obstructive pulmonary disease. Use of the V-slope method for anaerobic threshold determination. Chest 1988; 94: 931-338.
Wasserman K, Hansen JE, Sue DY, Stringer WW, Whipp BJ. Principles of exercise testing and interpretation, Fourth Edition. Lippincott, William and Wilkins, 2005.
Weber KT. What can we learn from exercise testing beyond the detection of myocardia ischemia? Clin Cardiol 1997; 20: 684-696.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

How can I determine RCP? Did u have done any post about that? How can i calculate PetO2 and PetCo2? Tks
Annan –
The RCP (Respiratory Compensation Point) is a secondary upwards inflection in Ve-VCO2 that occurs after anaerobic threshold. PetO2 and PetCO2 should be measured by your equipment otherwise you need traces of exhaled O2 and CO2 versus time and read them off these graphs.
– Richard
Isn’t the point at which Ve/VO2 reaches a minimum and then begins to rise without a corresponding increase in Ve/VCO2 the Aerobic Threshold and the Anaerobic one? What am I missing?
Radu –
It’s the anaerobic threshold. I haven’t heard of an aerobic threshold and maybe you’re thinking of the respiratory compensation point which happens, when it does at all, following the anaerobic threshold. It is a secondary upwards inflection point and is most likely due to an increased CO2 output and elevated lactic acid.
– Richard