A report came across my desk today and at first glance it looked fairly straightforward. There was a mildly reduced TLC and FVC, and although the SVC was slightly lower than the FVC it looked like this patient had mild restriction.
| Observed: | %Predicted: | Predicted: | |
| FVC: | 1.73 | 68% | 2.56 |
| FEV1: | 1.23 | 65% | 1.89 |
| FEV1/FVC: | 71 | 97% | 73 |
| TLC: | 3.58 | 73% | 4.89 |
| FRC: | 2.07 | 75% | 2.78 |
| RV: | 1.94 | 83% | 2.33 |
| RV/TLC: | 54 | 114% | 48 |
| SVC: | 1.69 | 66% | 2.56 |
| IC: | 1.51 | 72% | 2.11 |
| ERV: | 0.13 | 30% | 0.45 |
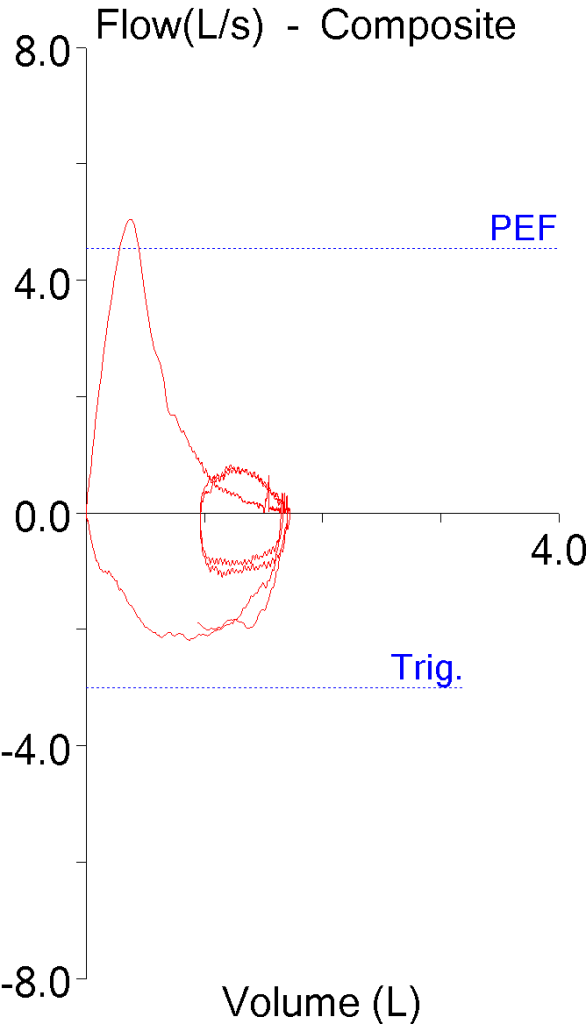
In addition, the flow-volume loop looked fairly typical for restriction, with a normal peak flow and a reduced volume.
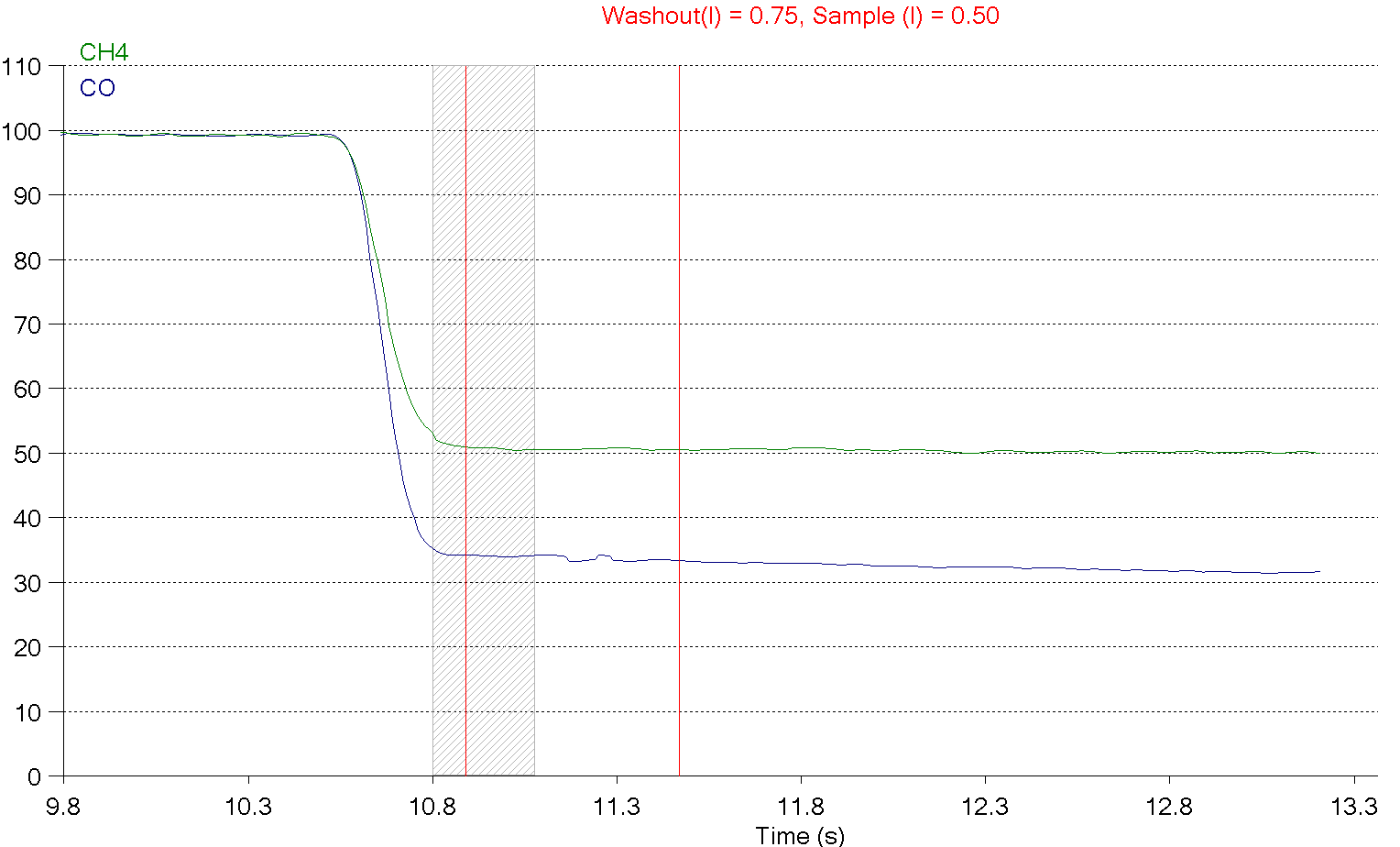
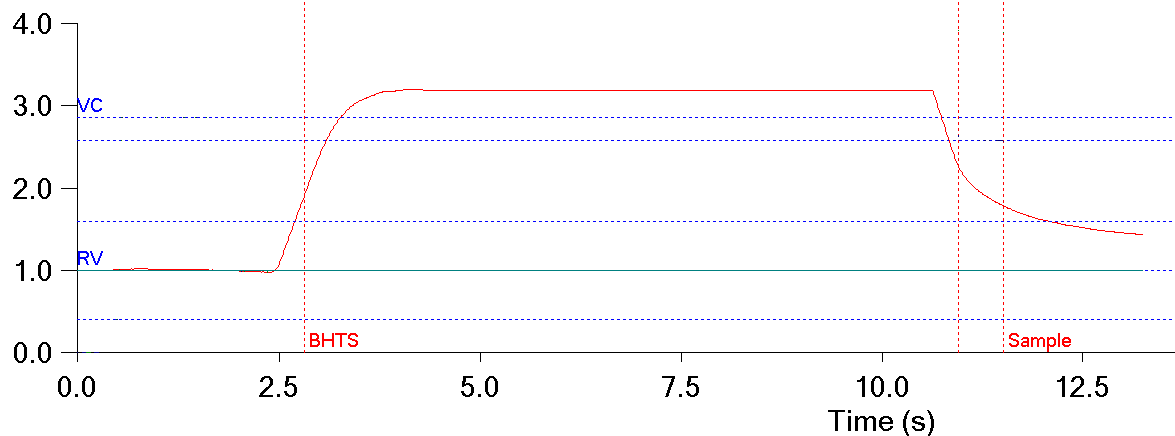
When I looked at the DLCO results however, I suddenly got a different picture. Specifically, the VA from the DLCO was larger than the TLC and the inspired volume (Vinsp) was significantly larger than both the FVC and the SVC.
| Observed: | %Predicted: | Predicted: | |
| DLCO: | 13.51 | 83% | 16.23 |
| VA: | 3.87 | 82% | 4.73 |
| Vinsp: | 2.26 |
The ATS/ERS recommends using the largest VC, whatever the source, when calculating the FEV1/VC ratio. When I substituted the Vinsp for the FVC in the FEV1/VC ratio I got was 54.4 (75% of predicted) and that immediately told me that the patient, despite the apparently normal FEV1/FVC ratio, actually had moderate airway obstruction.
As importantly, the VA and Vinsp made the reported TLC more than a bit questionable. Before thinking about making any corrections however, it’s important to determine whether the VA is believable. VA is calculated as a function of the inspired volume and the exhaled tracer gas concentration. The alveolar sample the exhaled gas concentration is measured from is optimized for DLCO measurements however, not lung volume measurements.
In this case, the tracer gas (CH4, green trace) is reasonably flat which indicates good gas mixing and suggests the VA is probably a good indication of the TLC.
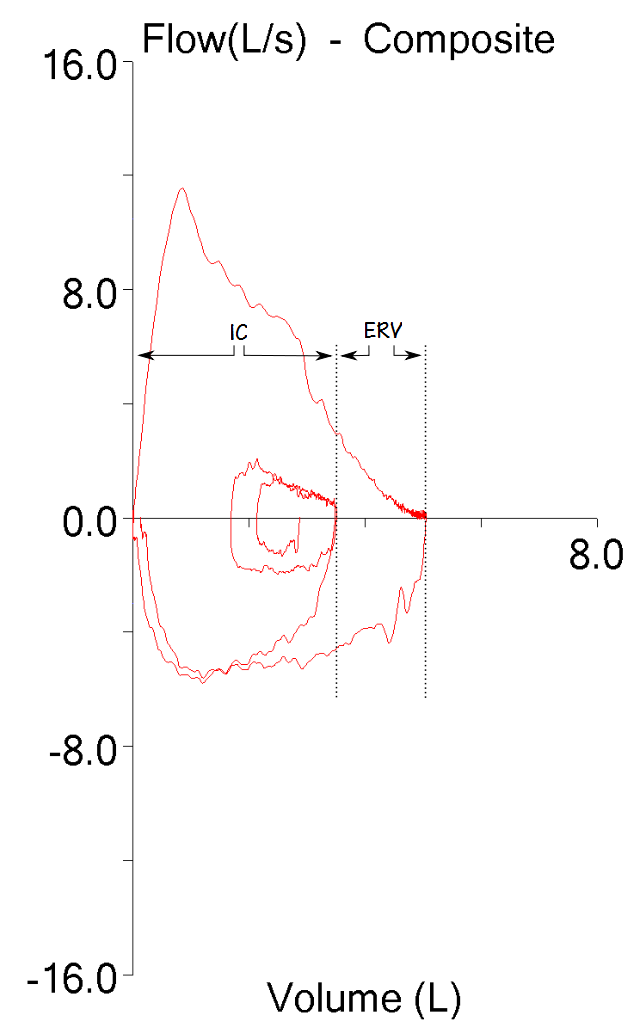
Given all this, is it possible to correct the reported TLC? In the past I’ve had reports where the FVC was substantially larger than the SVC and by analyzing the flow-volume loop I was able to derive IC and ERV.
In these cases I was able to correct the TLC by assuming the FRC was correct and then re-calculating the TLC and RV using the new IC and ERV. This time however, all I had was the volume curve from the DLCO test.
A simple approach would be to take the existing RV and then add the Vinsp:
1.94 L + 2.26 L = 4.20 L (86% of predicted).
but that assumes the existing RV was correct. The problem with this is that the existing SVC maneuver is already known to be suboptimal and that means that the ERV and therefore the RV are also questionable. If the patient’s ERV was instead assumed to be normal (0.45 L) then subtracting the predicted ERV from the FRC would give an RV of:
2.7 L – 0.45 L = 1.62 L (70% of predicted)
and TLC would be:
1.62 L + 2.26 L = 3.88 L (79% of predicted)
But a reduced RV in the presence of moderate airway obstruction just doesn’t seem quite right (although certainly not impossible if it is a mixed defect) and the TLC derived this way has a percent predicted that is a bit lower than the VA (predicted TLC and predicted VA differ by the amount of deadspace, which in this case is assumed to 0.16 L) so this probably isn’t correct.
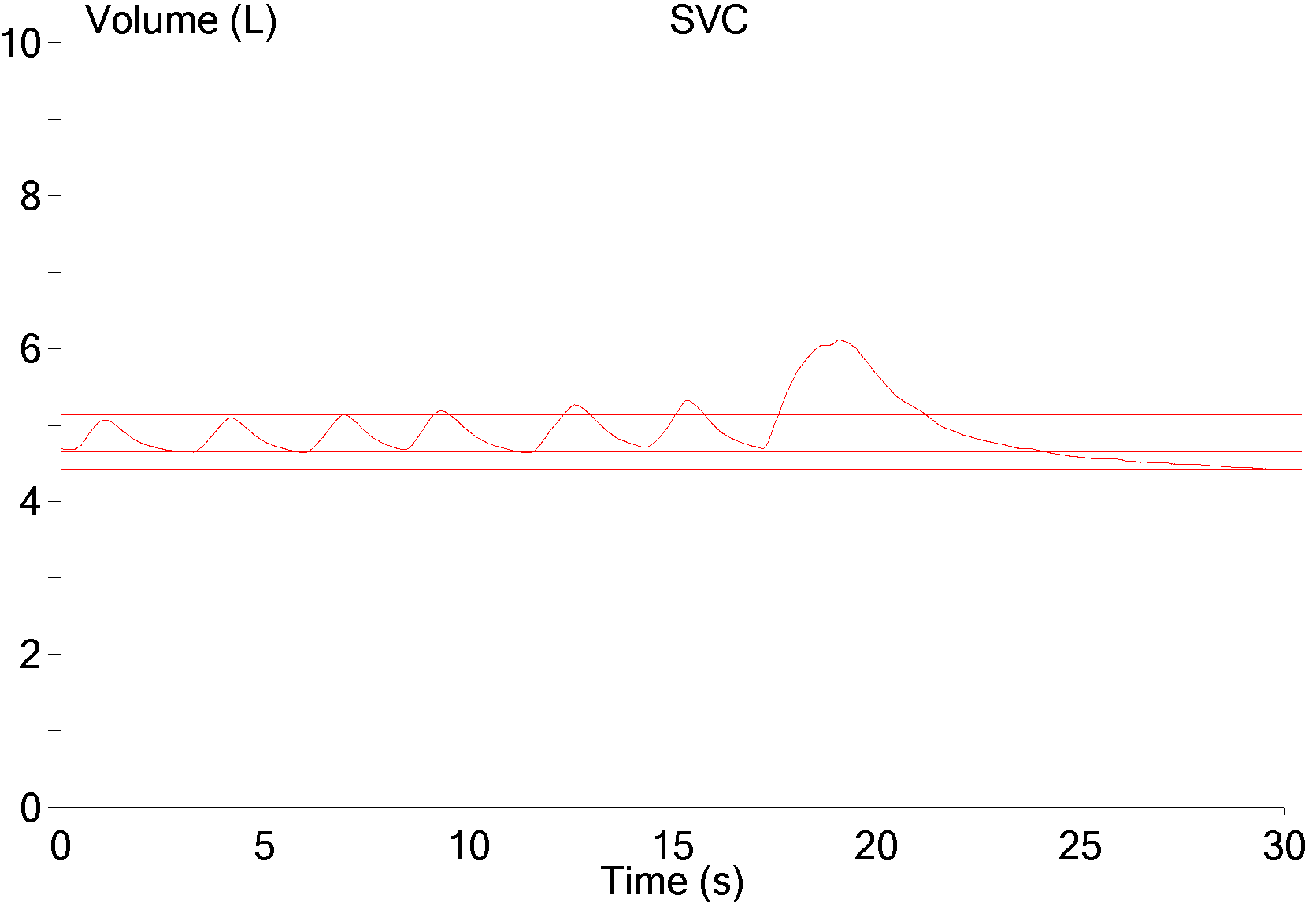
So is the ERV actually correct? Reviewing the SVC effort showed that the ERV portion looked fairly good.
The SVC effort lasted for about 10 seconds and half that time was below FRC. This means that there is a good chance that the RV is reasonably correct and that a TLC derived from the current RV and the Vinsp would also be reasonably correct.
As far as I’m concerned, the evidence shows the patient most likely has a TLC that is above our LLN (80% of predicted). The problem with all this and the reason that I am not actually able to correct the reported TLC is that without a “real” ERV or IC any method I use is just a guess and I can’t report numbers I can’t justify. In the end, the best I could do was to point out the moderate airway obstruction and say that the TLC was likely underestimated.
Despite the fact that the FVC, SVC and Vinsp are all vital capacities, our lab software does not alert a technician to any discrepancies between these measurements during testing. It’s not until the final report is generated that any differences between these values becomes evident. I would like to see the lab’s technicians take a harder look at the reported results and to be quicker to perform additional SVC maneuvers but I also realize that patients often balk at additional testing and that there can also be time constraints.
The SVC is an often overlooked part of lung volume measurement and it’s not clear to me that the link between the lung volume subdivisions measured during an SVC and the reported TLC and RV are as well understood as they should be. At one time or another we all learned that:
SVC = IC + ERV
FRC + IC = TLC
FRC – ERV = RV
Not exactly rocket science, but how often is this simple set of relationships kept in mind when assessing test results?

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License