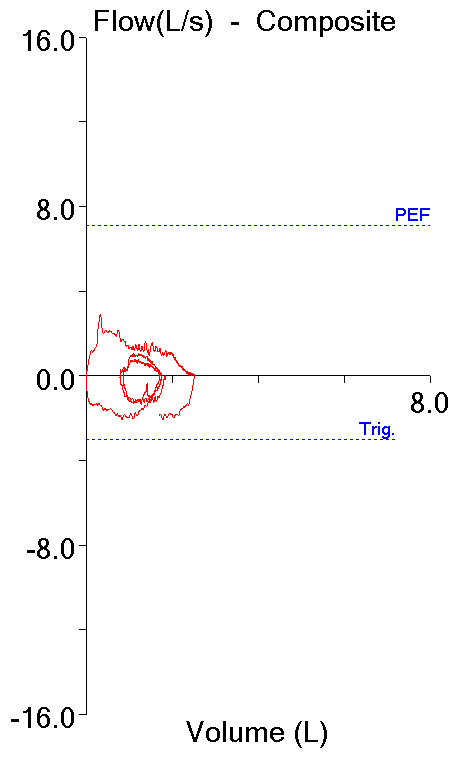
Recently I reviewed a set of completely irreproducible spirometry results. The patient had made eight attempts and the FVC, FEV1 and Peak Flow were different every time. In particular, there were frequent stops and starts during exhalation. I’ve always wondered why some patients have so much difficulty with what should be a simple test and although in this particular case it could simply be glottal closure I wondered if it could be Vocal Cord Dysfunction (VCD). For this reason I spent some time reviewing the literature.
Vocal Cord Dysfunction is defined as the paradoxical closure of the vocal cords with variable airflow obstruction that often mimics asthma and in fact VCD is often mistaken for refractory asthma. Unfortunately, for this reason individuals with VCD are often treated with corticosteroids and bronchodilators for years without any improvement of their symptoms.
The gold standard for diagnosing VCD is direct visualization of the vocal cords with a laryngoscope. Characteristically, the anterior (frontal) two-thirds of the vocal cords are closed with a narrow posterior glottal chink. The difficulty with this is that VCD symptoms are often transitory and a large number of patients that are suspected to have VCD are asymptomatic when a laryngoscopy is performed.
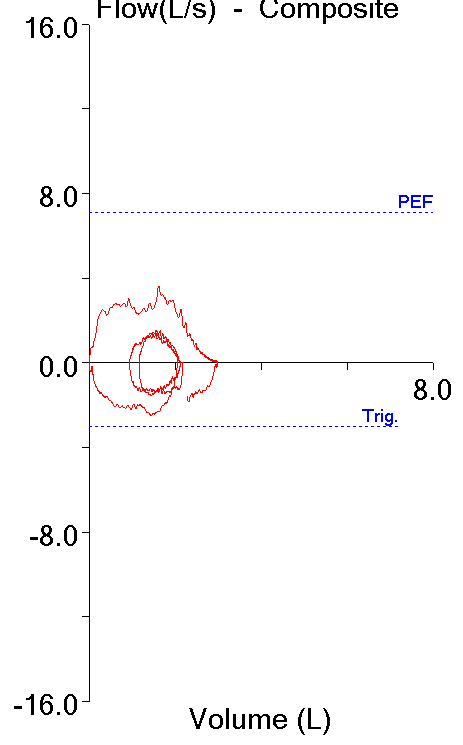
Since most PFT labs are not equipped with laryngoscopes nor are they prepared to perform a laryngoscopy at a moment’s notice we have to rely on the tests that measure airflow. Although the wheeze and shortness of breath that accompanies VCD mimics asthma the most common problem associated with VCD is inspiratory obstruction. The flow-volume loop pattern is therefore that of a variable extrathoracic airway obstruction.