The static respiratory pressures, Maximal Inspiratory Pressure (MIP or PIMAX) and Maximal Expiratory Pressure (MEP or PEMAX) are a way to non-invasively assess respiratory muscle strength. Respiratory muscle weakness is present in a number of conditions, most notably neuromuscular diseases and disorders, but also malnutrition, cardiovascular disease, polymyositis, sarcoid and COPD. Strictly speaking, the maximal inspiratory and expiratory pressures are not generated solely by the respiratory muscles but also by the elastic recoil. The elastic recoil of the lung at TLC contributes up to 40 cm H2O towards MEP and the elastic recoil of the chest wall at RV contributes up to 30 cm H2O towards MIP. Even so, an individual cannot reach TLC or RV without the use of their respiratory muscles so the measurements are still valid regardless of how the pressures are generated.
I have mixed feeling about MIPs and MEPs but this is mostly because many patients perform these tests poorly, making it hard to interpret results. Normal results can rule out respiratory muscle weakness but reduced results are not necessarily diagnostic. Nevertheless, they are still valuable tests and it is important for them to be performed correctly.
MIP is measured at RV and MEP is measured at TLC. The ATS/ERS statement on respiratory muscle testing indicates that each effort should last at least 1.5 seconds and that at least three measurements within 20% of the highest value should be obtained. A maximum number of attempts has not been specified but most research studies limited this to 5 or 6.
The actual maneuver depends somewhat on the equipment configuration. Respiratory pressures were originally measured using a pressure gauge and most early systems consisted of just a mouthpiece and a gauge (or gauges).
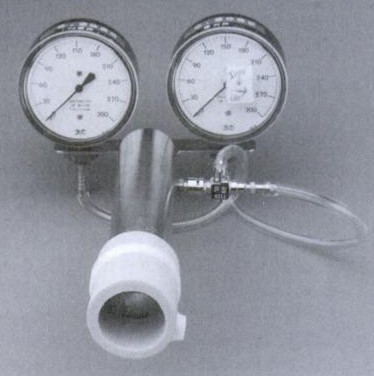
from ‘Interpretation of Pulmonary Function Tests – A Practical Guide’ by RE Hyatt, PD Scanlon and M Nakamura, Published by Lipincott-Raven, 1997, page 90.
To use this type of system the patient either exhales to RV or inhales to TLC, places their lips around the mouthpiece and then forcefully inhales or exhales. Because of the limited amount of time available for lip placement a round plastic or cardboard mouthpiece is usually used.
