Airway hyper-responsiveness is a primary feature of asthma. There are a number of bronchial challenge tests designed to evoke and measure this factor, the most common of which require the inhalation of one or another bronchoconstrictive agent such as methacholine, histamine, mannitol or hypertonic saline.
An elevated ventilation can cause many asthmatics to bronchoconstrict and this is often the cause of Exercise-Induced Bronchospasm (EIB). There are two competing theories as to why this happens. A number of researchers have suggested that the mechanism is a drying of the airway mucosa which changes the osmolarity of the respiratory tract fluid which in turn causes some cells to releases mediators that cause bronchoconstriction. Other researchers assert that it is the cooling of the airways during hyperventilation and an increased blood flow and edema during subsequent re-warming that causes the bronchoconstriction. There is evidence to support both interpretations and it is likely that both mechanisms coexist, with one or the other being more predominant in any given individual.
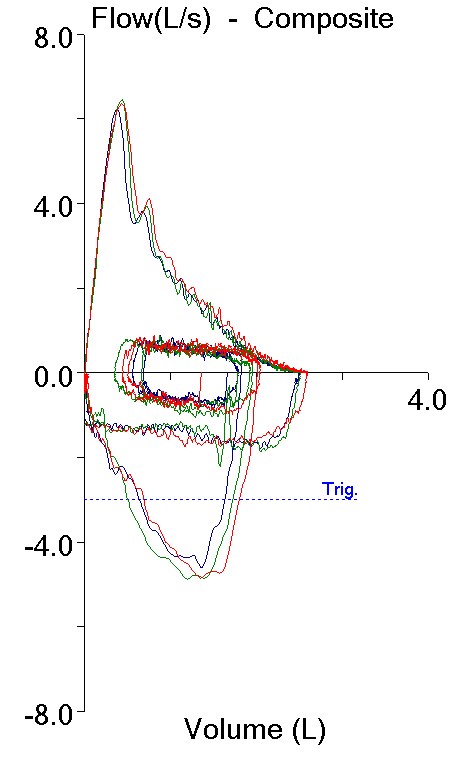
Although the inhalation challenge tests are reasonably sensitive not all patients with EIB have a positive reaction. When a patient’s primary complaint is exercise-related or when they have had a negative inhalation challenge test and are still symptomatic, a ventilatory challenge test should be considered. There are several ventilatory challenge tests that are specifically oriented towards evoking and characterizing EIB. These are the Cold Air challenge, Eucapnic Voluntary Hyperventilation and Exercise Challenge. There are a number of similarities between these tests.
Cold Air Challenge
A Cold Air Challenge (CACh) test consists of having a patient hyperventilate while breathing air that has been cooled to a temperature of between -10°C and -20°C. It is usually performed using a mixture of 5% CO2, 21% O2, 74% N2 in order to prevent dizziness from hypocapnia.