Outside the pulmonary lab there is this notion that spirometry is supposed to be so easy that anyone can do it. You just tell the patient to take a deep breath in and blow out fast and to keep blowing until they’re empty. What’s so hard about that?
Sheesh. GIGO. I keep finding ways in which the patient, their physiology and our equipment can conspire in ways to produce errors that even experienced technicians can miss. I’ve been paying a lot of attention to flow-volume loops lately and maybe it’s for this reason that I’ve seen a steady stream of spirometry tests that have something wrong with the FVC volume.
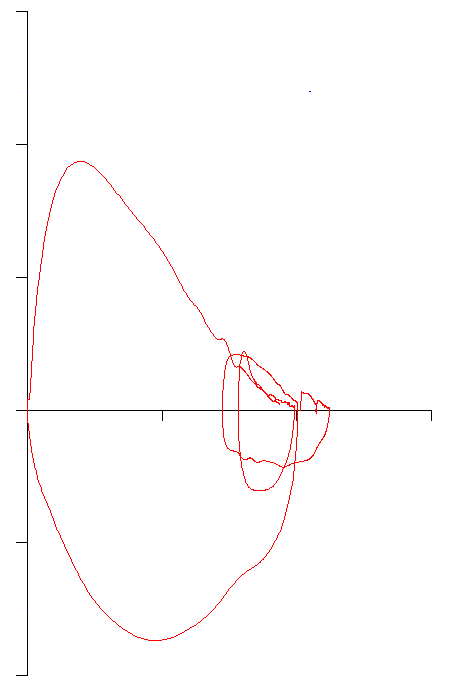
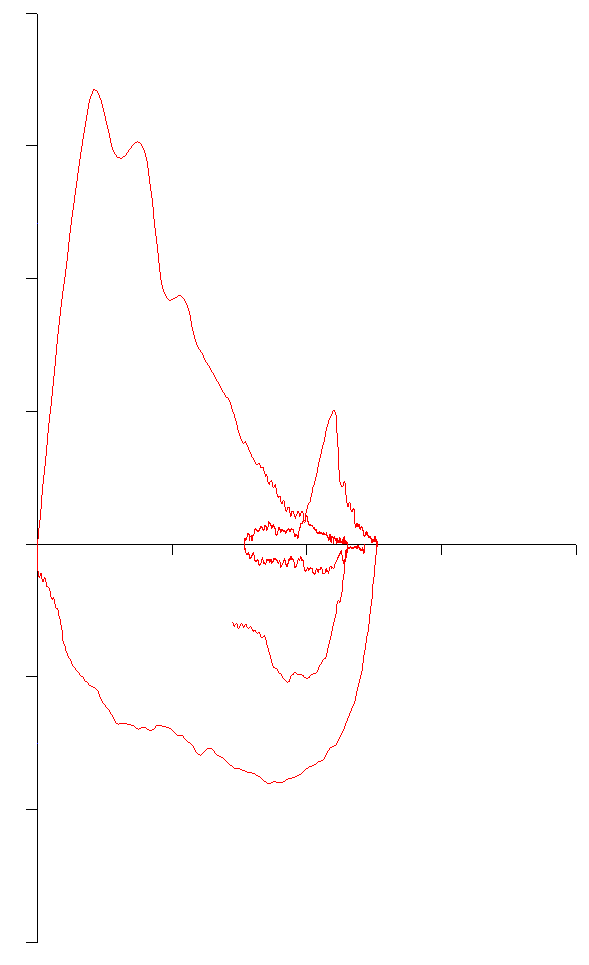
What I’ve been seeing are flow-volume loops where the end of exhalation is to the left of either the start of the FVC inhalation or of the tidal loop. Taken at face value this means that the patient did not exhale as much as they inhaled (and that the FVC is therefore underestimated) but there are several reasons why this happens and it takes a bit of detective work to figure out the cause and what to do about it.
The simplest reason is a short expiratory time. Flow-volume loops however, do not show time, only flow and volume. Sometimes when a patient stops exhaling abruptly it’s easy to see that the effort is short.
Other times it isn’t as clear:
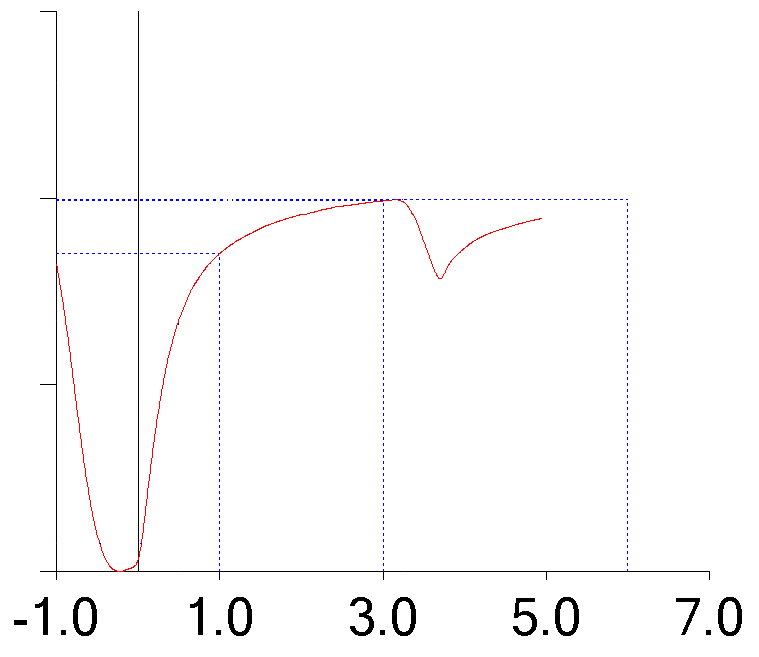
and you need to look at the volume-time curve as well.
In some ways this is both the easiest and hardest error to correct. The simple fix is to get the patient to exhale longer, but many patients can not or will not do this no matter how many times you try. Frequently it’s because the patient is SOB or just not feeling well. Sometimes it’s due to language or cultural barriers. Sometimes it’s just because the patient doesn’t “get it”. Surprisingly enough (for my lab at least) I’d say that a lack of cooperation is in a distant last place as a cause and this is probably because we mostly see outpatients and if they don’t want to do the tests, they don’t show up.
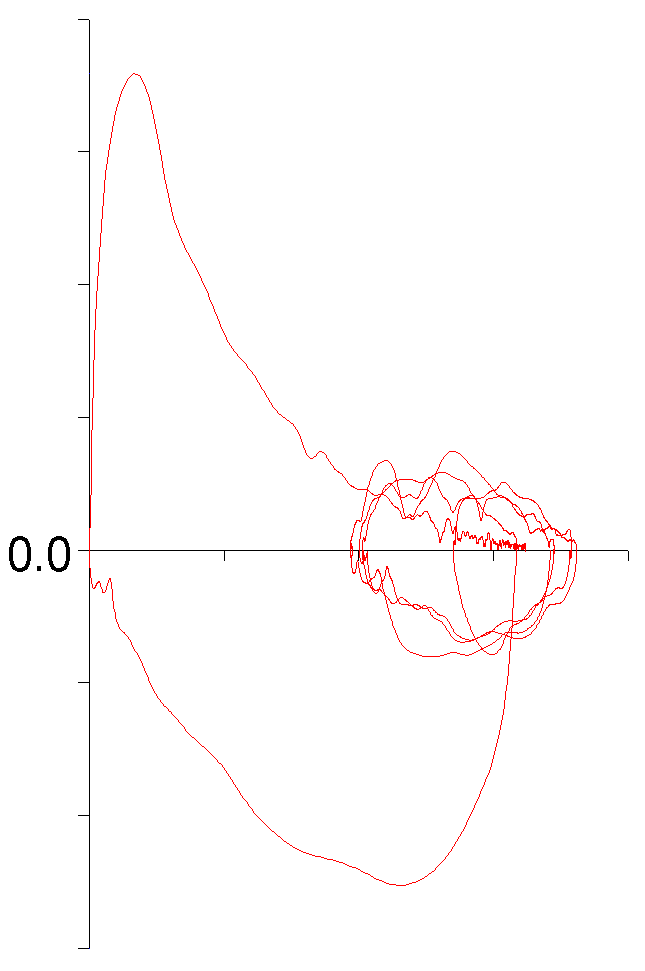
Another reason that the FVC can be underestimated is gas trapping. Gas trapping is usually seen with severe airway obstruction but this patient had an FEV1 that was within normal limits and their FEV1/FVC ratio was only slightly below the LLN.
And the expiratory time was adequate.
One clue that this is gas trapping and not something else is that the tidal loop overlaps itself reasonably well and is not obviously drifting to either the left or the right. When our lab software displays a volume-time curve it does not show more than one second of data before the start of the FVC effort. Fortunately, I can download the raw test data and re-graph it using a spreadsheet and when this is done, it can be seen that the patient was unable to return to the tidal baseline with the FVC effort.
There is no “fix” for gas trapping. Some investigators have proposed that after the initial blast (presumably including the peak flow and FEV1) patients should be told to relax their effort while continuing to exhale and that this will allow a larger FVC volume to be measured. To my knowledge this has not been formally studied so any improvement in FVC volume would be conjectural. In addition the difference between an FVC effort that is forced throughout the maneuver versus one that is only forced at the beginning is a distinction that many patients may not be able to make.
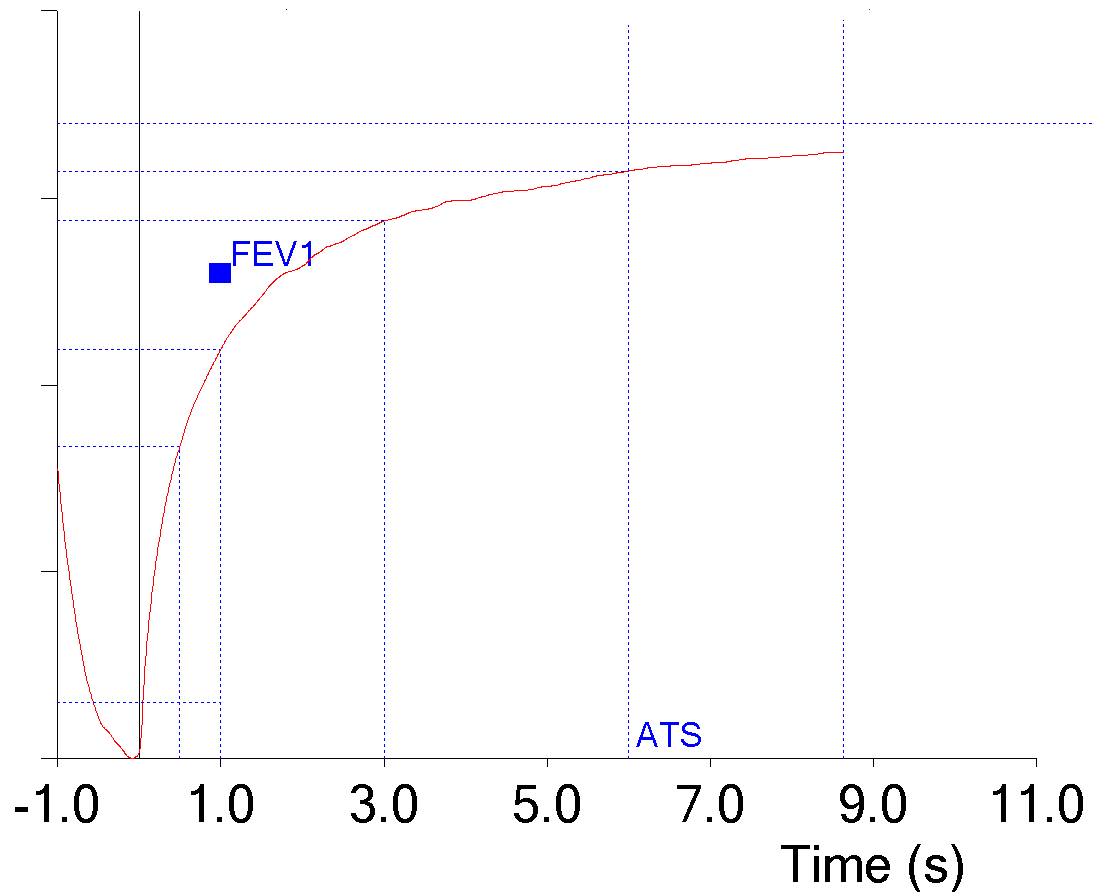
Finally, my lab has a mix of different test systems. Some are simple pneumotach spirometry systems, some are plethysmograph systems with pneumotachs and pressure-actuated valves, and some are volume displacement spirometry systems with pressure-actuated valves. For all of these systems either the patient or the system itself can leak.
The easiest way to see a leak is to notice whether or not the tidal loop is drifting but in this case the patient only had one tidal breath before starting the FVC maneuver. The patient’s FEV1 and PEF were above normal so gas trapping is unlikely. They also exhaled for a reasonable period of time.
This means that a leak is really the only possibility. Once it’s detected a leak should be fixed before any further testing is performed. Yes, this means that testing needs to be put on hold until this is done but continuing to perform tests while knowing there is a leak is just not acceptable in any way.
So, simple stuff, yes? But the reason I selected these specific examples was that in every case the technician performing the test wrote “good test quality” in the notes. This can probably be excused for the patient with gas trapping since in every other way the test effort met the criteria for acceptability. But the others? Not so much.
All of the technicians in my lab have a minimum of two years of experience, and in several cases quite a few more. So why did they miss these things? In each case the primary clue that the FVC was being underestimated was because the end of exhalation of the FVC maneuver was at a lower volume (further to the left) than the tidal loops. So I think it is largely because everybody (and I’ve seen this in other labs than my own) tends to ignore tidal loops. I suspect that the most common thought is that tidal loops are just something that happens before the FVC maneuver so of course they aren’t really important.
There is also nothing in the ATS/ERS spirometry standards that specifically addresses tidal loops. To a large extent I can understand this since the standards are primarily designed to address the actual FVC, SVC and MVV test maneuvers. Even so, the standards include several graphs that show the tidal breathing prior to the maneuver and it is evident that it is assumed to be stable and not drifting in any way. For this reason I think that the next time the ATS/ERS spirometry standards are updated it wouldn’t hurt to define the acceptable limits on any drift during tidal breathing.
Finally, I’ve seen some test system software that did not allow tidal loops to be displayed. In some cases this was just in the manufacturer’s sales literature so it may actually be possible to override this. Even so tidal breathing is part of the FVC maneuver and because it can provide important clues on expiratory time, gas trapping and leaks it should always be included when flow-volume loops are displayed.
The “simple” FVC maneuver has numerous subtleties and it’s a harder test to perform correctly than may appear at first glance. We’re not going to stop spirometry from being performed outside the pulmonary lab (nor should we even try) but if we’re going to show why pulmonary labs continue to be needed then we’re going to have to make sure that we perform spirometry better than anybody else. In particular that means we need to understand and pay attention to all of the details and for spirometry that includes the tidal loops.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License