Recently I was reading the blog of someone who teaches Pulmonary Function testing and they stated:
“…in emphysema and air trapping, the VTG (thoracic gas volume) will be higher than a FRC (functional residual capacity) measured by Helium dilution and Nitrogen washout. This is because VTG is the volume of gas contained in the thorax, whether in communication with the airways or trapped in the thorax.”
This unfortunately is not correct, but it is a common misconception and since there was a time when I believed it myself I find it difficult to fault the author too much. I think it’s time to return to the basics of plethysmographic lung volumes however, and show why this is not true.
Plethysmography relies on Boyle’s law, which is:
P1V1 = P2V2
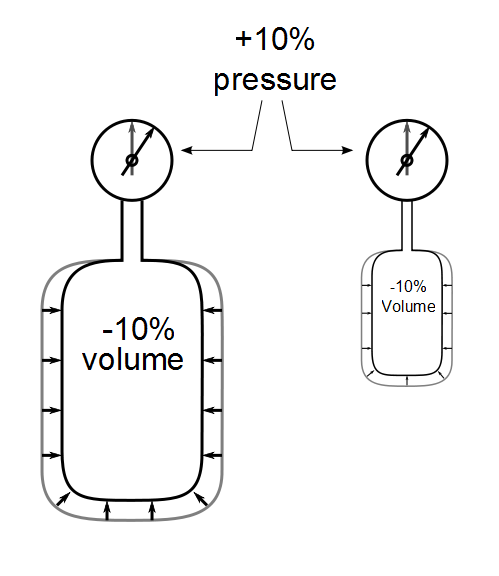
This means that in a closed system, there is a proportional relationship between pressure and volume. Decrease the volume and the pressure increases proportionally. Increase volume and the pressure decreases proportionally as well. This effect is independent of the size of the system, so both large and small systems will act in the same way.
To measure lung volume, lungs (the person is optional) are placed inside of a pressure-tight box (the plethysmograph). When the patient inhales and exhales against a closed shutter the lungs expand and compress and mouth pressure decreases and increases accordingly. This maneuvercompresses and rarifies the air in the box and the pressure in the box increases and decreases.
The volume of the lungs is small compared to the volume of the box and the change in box pressure is going to be proportional to:
[change in lung volume] / [box volume]
Plethysmographs have a volume of roughly 600 liters. Assuming the patient compresses or expands their lungs with 30 cm H2O pressure, for a 6-liter lung volume this will cause the entire lung to compress or expand by about 180 ml. This in turns will cause a pressure change of approximately +/- 0.3 cm H2O inside the plethysmograph. (Yes, that small a change, and the box‘s pressure transducer has to be exceedingly sensitive. I remember performing manual calibrations on this transducer and being able to tell when somebody opened a door at the other end of the lab which was around a corner).
The change in box pressure (which is directly related to volume of compression or expansion of the patient’s lung)and the change in mouth pressure are all of the elements that are needed to calculate lung volume using Boyle’s law (as long as you also know the barometric pressure and the volume of the box). The math is rather straightforward but it is easier to think of this graphically.
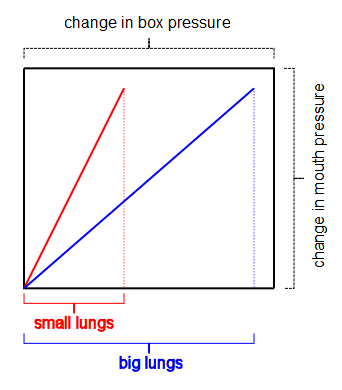
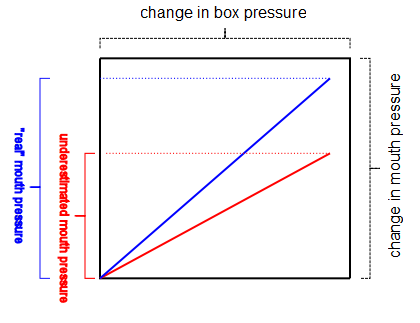
Mouth pressure and box pressure are simultaneously plotted against each other and it is the slope of this vector tracing the shows lung volume. Assuming that the same amount of pressure is used to expand or compress the lungs (and humans, regardless of size, tend to generate the same pressures) a small lung will cause a small change in box pressure and therefore a steep pressure tracing. A large lung will cause a large change in box pressure and a shallow pressure tracing. The slope of the tracing is therefore directly related to the volume of the lung.
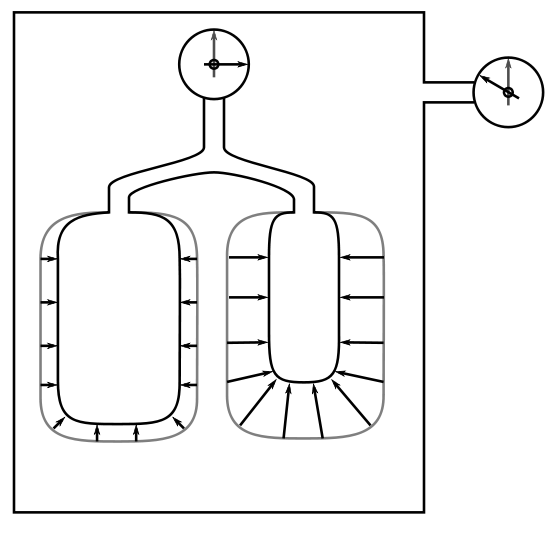
This measurement process can work well but an absolutely critical assumption is that the pressure measured at the mouth is the same as the average pressure inside the lungs. For patients with normal lungs this assumption is reasonably correct, but when lungs are diseased this is not necessarily the case at all. In obstructive lung diseases in particular the disease processes in the lung are often not homogeneous. This can cause different parts of the lung to go through different volume and pressure changes during the measurement maneuver. As long as the pressure measured at the mouth is equal to the average pressure inside the lung then the measured lung volume will be correct.
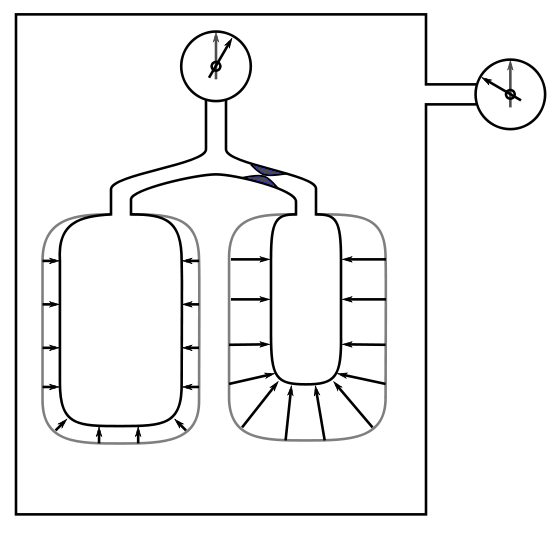
When airways are obstructed however, the pressure changes in trapped air may not be reflected at the mouth.
The pressure of trapped air cannot be less than the average pressure inside the lung and there are a number of reasons to believe it is often higher. It does not matter whether airway obstruction is localized or diffusely spread throughout the lung, the presence of trapped air usually causes mouth pressure to underestimate the average pressure inside the lung. When this underestimated pressure is compared to the actual compression volume of the lung, TGV will be overestimated.
So the misconception isn’t that a plethysmograph can measure “trapped air”, it’s that it can measure it accurately. Helium dilution and nitrogen washout lung volumes are in fact more likely to be accurate when obstruction is present.
My PFT Lab has been involved in funded research projects for close to 20 years. Almost all investigators that have come to us and asked for lung volumes to be performed have insisted that they be performed in a plethysmograph. Since more than one researcher has noted (starting over 30 years ago) that lung capacity tends to be overestimated when airway obstruction is present and that the amount of overestimation is related to the degree of airway obstruction, why has plethysmography continued to be considered the “gold standard” for lung volumes?
I think that part of the reason for this is that accurate lung volume measurement, regardless of technique, is far more difficult than is usually credited and verification of the problem has had to wait until measurements could be independently confirmed with thoracic volumes analyzed by CAT scan. I also think that for a researcher the fact that “everybody else” uses plethysmography means that using anything different would cause reviewers to needlessly question their study results. Finally, I think there is an element of time management (or laziness) involved since the fact that you can perform a half dozen plethysmography lung volume measurements in the same time it takes to measure lung volumes by helium dilution once makes it quicker and easier to use a plethymograph.
I am not going to say that obstructive hyperinflation and “trapped air” don’t exist. I’m also not going to say the helium dilution or nitrogen washout tests can’t underestimate lung volumes when obstruction is present. But instead of accepting the myth that plethysmographic lung volumes are always accurate and that helium dilution or nitrogen washout lung volumes are underestimated because of “trapped gas” it is time to start thinking the opposite may be true instead.
References:
Brown R, Ingram RH Jr, McFadden ER Jr. Problems in the plethysmographic assessment of changes in total lung capacity in asthma. Am Rev Respir Dis 1978; 118: 685-692.
Goldman MD, Smith HJ, Ulmer WT. Whole-body plethysmography. Eur Respir Mon 2005; 31: 15-43
O’Donnell CR, Bankier AA, Stiebellehner L, Reilly JJ, Brown R, Loring SH. Comparison of plethysmographic and helium dilution lung volumes: Which is better for COPD? Chest 2010; 137: 1108-1115.
Rodenstein DO, Stanescu DC, Francis C. Demonstration of failure of body plethysmography in airway obstruction. J Appl Physiol 1982: 52: 949-954.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License


Hello Richard,
If one was able to “plug off” one half of a patients lungs- would FRC Pleth not account for total volume (both the communicating and non-communicating airways whereas, FRC Nitrogen washout or Helium dilution would not, therefore underestimate the lung volumes?
Regards,
Mo RRT
Mo –
Plethysmographic lung volumes depends on the relationship between box pressure and mouth pressure. Presumably the entire lung and thorax would continue to expand and contract by the same amount after you had “plugged off” one side so the box pressure excursion would remain the same as well. The question would be whether or not the mouth pressure (which is a stand-in for alveolar pressure) in the “unplugged” lung would be the same or different than the average mouth pressure from both lungs. Depending on underlying disease processes (and even due to normal physiology) there are reasons why it could be different and if it is higher or lower the measured TGV would then be lower or higher. The assumption that mouth pressure is the same as the average alveolar pressure is the weak link in plethysmographic lung volume measurements.
– Richard