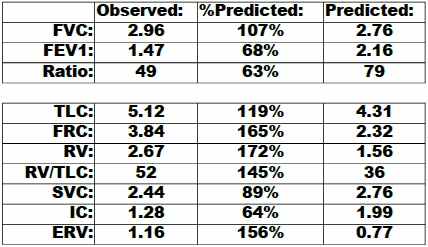
This PFT report came across my desk the other day. At first glance it looked wrong because when was the last time you saw a patient with a FRC that was 165% of predicted?
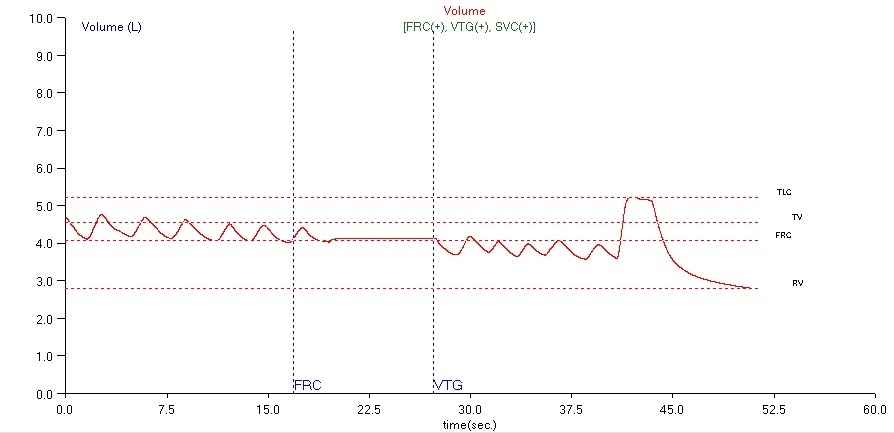
Lung volumes were done by plethysmography and I took a close look at the TGV loops (mouth pressure vs box volume) and they had excellent quality and reproducibility, about as good as you can ever expect. When I looked at the volume data however, it was apparent that the patient leaked during the panting maneuver while the shutter was closed.
As you can see there is a significant baseline shift before and after the shutter closed but this actually means it is the TLC that is underestimated not that the FRC is overestimated. In our plethysmograph system the FRC is determined from the tidal breathing before the shutter closes. When the shutter closes and the patient performs the panting maneuver TGV is measured. The system looks at where the shutter closed relative to the previously established end-of-exhalation baseline level and uses this to determine FRC. FRC is therefore based on what happened before the shutter closes not after.
After the shutter opens the patient returns to tidal breathing and then performs a slow vital capacity maneuver. ERV is measured from the original FRC level and the point of maximum exhalation from the SVC. RV is calculated from FRC minus ERV and TLC is calculated from SVC plus RV. In this case the baseline shifted downwards during the time the shutter was closed. This means that ERV is overestimated and therefore RV and TLC are underestimated.
I measured the baseline shift to be just about 0.48 liter. Add in the fact that the SVC is 0.52 liter less than the FVC this means the TLC is underestimated by at least 1.00 liter, so the “real” TLC is at least 6.12 liters or 142% of predicted. This makes about as much sense as the FRC of 165% of predicted.
In chronic, severe airway obstruction it is possible for patients to hyperinflate and over time develop barrel chests with an elevated TLC and FRC although even when this happens a TLC of 142% of predicted is on the high side. But this is with chronic, severe airway obstruction and as you can see the patient’s FEV1 is only moderately reduced. The patient also did not physically fit the picture of chronic emphysema nor did she fit it physiologically as the DLCO was 69% of predicted. Mild to moderate COPD maybe, but not chronic severe COPD.
I will mention in passing that a barrel chest is something you’re more likely to see in a textbook these days than in your PFT Lab. Severe emphysema used to be more common than it is now. Since the Surgeon General’s report in the 1960’s there are fewer smokers and COPD is recognized much sooner than it used to be. Improved medications and supplemental oxygen has made the barrel chest a much rarer creature than when I started doing pulmonary function testing forty years ago.
Do I believe the test results? Well, the TGV measurement and therefore the FRC measurement had excellent quality so they should be correct, but as a matter of fact, no, I don’t. It just doesn’t fit the picture presented by the patient herself. What I think is happening is that TGV itself is overestimated. Plethysmography used to be considered the gold standard for lung volume measurements, but it has come to be realized that TLC is usually overestimated when there is airway obstruction and the degree of overestimation tends to correlate with the degree of obstruction.
This is because a critical assumption that is made in plethysmographic lung volume measurements is that the airway pressure measured at the mouth is representative of the pressure inside the entire lung. This is a reasonable assumption in normal lungs but when airway obstruction and gas trapping is present this is no longer the case.
Could the leak while the shutter was closed cause an overestimation of TGV? All of the TGV loops were straight, narrow and without any inflections or curves. They were also highly reproducible so I have to say this is probably not the case.
Under normal circumstances I would say that the degree of obstruction indicated by a FEV1 of 68% of predicted might elevate the TGV a bit but not significantly. In this case however, there must be something about the quality of this patient’s airway obstruction that is leading to a marked overestimation of her lung volumes.
References:
O’Donnell CR, Bankier AA, Stiebellehner L, Reilly JJ, Brown R, Loring SH. Comparison of plethysmographic and helium dilution lung volumes: Which is best for COPD? Chest 2010; 137: 1108-1115.
Rodenstein DO, Stanescu DC, Francis C. Demonstration of failure of body plethysmography in airway obstruction. J Appl Physiol 1982; 52: 949-954.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.