Although we routinely use mouthpieces, noseclips and occasionally masks for our testing, all of these alter respiration in one way or another. Opto-electronic plethysmography (OEP) is a completely non-invasive technique for measuring chest wall volume that also allows for regional differences in expansion and contraction of the thorax to be detected.
The basic idea is simple and is the same as is used in cinematic motion-capture systems. Small (6-10 mm) reflective hemispheres are attached to a subject’s torso with double sided tape. A set of 4, 6 or 8 high-speed (60-120 frames/sec) CCD cameras are then used to monitor both the overall and the relative motion of the hemispheres while the subject breathes. The accuracy of these measurements is claimed to be on the order of 0.2 mm.
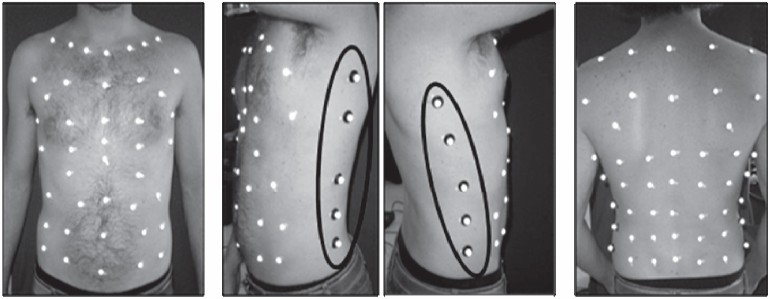
from Optoelectronic plethysmography: a review of the literature. Braz J Phys Ther 2012; 16: page 441.
The volume enclosed by the markers is analyzed geometrically by using a triangular or polyhedronal mesh. Since the triangles or polyhedrons are flat and human thoraxes are round-ish, volume tends to be underestimated to some degree. The amount of underestimation is closely related to the number of markers that are used and where they are placed. Research has shown that around 50 markers are needed for supine patients when only the anterior thorax is measured and more than 80 are needed for full coverage of upright patients. Reflectors need to cover the entire thorax, usually from the jugular notch on the upper chest to the iliac crest near the hips.

From Chest wall motion and lung volume estimation by optical reflectance motion analysis. J Appl Physiol 1996; 81: page 2683.
OEP has an accuracy that is similar to the ATS/ERS standards for spirometry. One study estimated that the coefficient of variance for static thoracic volume measurements was 2% and 3.5% for changes in thoracic volume. Another study showed a similarly small discrepancy of -2.4 +/- 3.9% when OEP was compared to volumes measured by a flow sensor during both light and heavy exercise.
OEP isn’t going to replace spirometry anytime soon however, since placing the reflectors takes up to 45 minutes. Calibration of the cameras and reflectors can take additional time as well. At least one study indicated that placement of the reflectors has to be exceptionally precise and that errors of more than 1 mm in placement made the reflector unrecognizable to the computer and required manual adjustment in the software. Subjects being measured must also be bare chested throughout the process which is something that some patients may not be comfortable with.
In addition, OEP can only measure the volume and change in volume of the external thorax, not the volume of the lung and not the actual expiratory (or inspiratory) flow at the mouth. Air inside the thorax must be compressed (or rarified) for gas flow to occur. The actual flow rate of expired (or inspired) gas will therefore be dependent on the pressure gradient between the atmosphere and the lungs, and the resistance of the airways. Although several studies have shown good correlation between tidal volumes measured by OEP and spirometers, a comparison of expiratory and inspiratory flow rates does not appear to have been made.
The greatest advantage that OEP has over conventional spirometry is that it permits separate measurement of up to six components of the thorax. These are the right and left sides of the pulmonary rib cages, abdominal rib cages and abdomen. Differences in these compartments during different breathing maneuvers are particularly useful in assessing assymetrical breathing patterns.
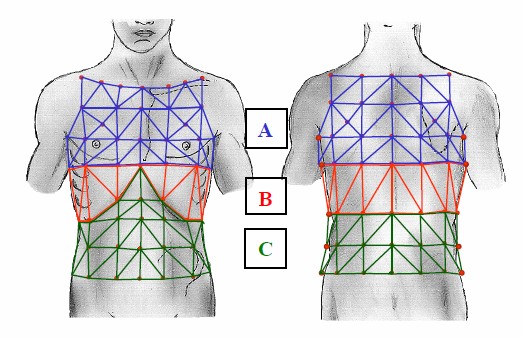
A – pulmonary rib cage, B – abdominal rib cage, C – abdomen. From Optoelectronic plethysmography has improved our knowledge of respiratory physiology and pathophysiology. Sensors 2008; 8: page 7954.
For example, a definitive diagnosis of unilateral diaphragmatic paralysis usually requires fluoroscopy, ultrasonography or phrenic nerve stimulation with diaphragmatic electromyography all of which tend to require experienced specialists and/or specialized equipment. One study has shown that when unilateral diaphragmatic paralysis is present the change in thoracic volume on the affected side during tidal breathing and inspiratory capacity maneuvers is significantly less than it is on the unaffected side. This raises the possibility that OEP could diagnose this kind of paralysis more quickly and easily than it is at present.
OEP has been used to research chest wall motion during speech; expiratory flow limitation during exercise; ventilation during hypercapnia; asymmetrical breathing from hemiplagia; hyperinflation in asthmatics during histamine-induced bronchoconstriction; thoracic motion during cough, laughter and unsupported upper arm exercise; the decrease abdominal (diaphragmatic) motion from muscular dystrophy; respiratory effort while walking; the contribution of abominal volume to dynamic hyperinflation in COPD; the contribution of abdominal volume to supine tidal volume in muscular dystrophy and diaphragmatic motion during supine breathing.
Clinically, OEP has been used to assess the respiration of newborns and ventilator patients, and has also been used to assess hyperinflation in patients with COPD during exercise. At the present time however, there is no CPT4 code for OEP and Medicare will not pay for it. In addition, OEP is a time-consuming and cumbersome process in the hospital setting and its primary value continues to be in research.
A newer technique that is similar to OEP is Structured Light Plethysmography (SLP). A grid is projected onto a patient’s chest, and like OEP the three-dimensional motion of the grid during breathing is detected by a set of cameras.
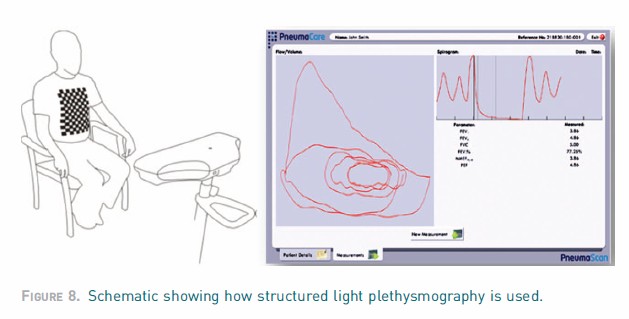
From Non-invasive assessment of lung function with reference to external light-based techniques. 2012 ERS Buyers Guide, page 67.
Despite the fact that a SLP system is commercially available it is unclear what level of accuracy SLP has versus OEP and versus conventional spirometry. On-line demonstrations of SLP have shown a projected grid that only covers the central part of the anterior chest. This may be acceptable for a supine breathing assessment but OEP researchers have emphasized the need measure motion at the margins of the thorax even for supine measurements. A number of meeting abstracts concerning SLP have been published but I have been unable to find any journal articles on the subject.
OEP is an interesting technique that at present is more suited for research than it is for a clinical PFT Lab. Having said that, a primary limitation of OEP is the ability to detect motion via reflectors that must be affixed to a subject’s thorax. Improvements in processing power and machine vision may make it possible to assess thoracic volume without the need to place reflectors. Since OEP (and SLP) can only measure changes in volume these techniques cannot replace traditional lung volume and diffusing capacity measurements. There are also reasons why OEP may have a limited ability to measure inspiratory and expiratory flow rates and this may well mean that it will be unable to replace spirometry as well.
The ability to detect asymmetrical breathing patterns however, is a relatively unique ability of OEP. It may well turn out that when measuring thoracic compartmental motion is easy to measure asymmetrical breathing may be found to be a more common problem than currently believed.
Product links:
OEP: BTS Bioengineering
SLP: Pneumacare
References:
Aliverti A, Stevenson N, Dellaca RL, Lo Mauro A, Pedotti A, Calverley PM A. Regional chest wall volumes during exercise in chronic obstructive pulmonary disease. Thorax 2004; 59: 210-216.
Aliverti A, Dellaca R, Pelosi P, Chiumello D, Pedotti A, Gattinoni L. Optoelectronic plethysmography in intensive care patients. Amer J Respir Crit Care Med 2000; 161: 1546-1552.
Boudarham J, Pradon D, Prigent H, Falaize L, Durand MC, Meric H, Petitjean M, Lofaso F. Optoelectronic plethysmography as an alternative method for the diagnosis of unilateral diaphragmatic weakness. Chest 2013; 144(3): 887-895.
Cala SJ, Kenyon CM, Ferrigno G, Carnevali P, Aliverti A, Pedotti A, MacKlem PT, Rochester DF. Chest wall motion and lung volume estimation by optical reflectance motion analysis. J Appl Physiol 1996; 81: 2680-2689.
de Boer WH, Lasenby J, Cameron J, Wareham R, Ahmad S, Roach C, Hills W, Iles R. SLP: A zero-contact non-invasive method for pulmonary function testing. Paper presented at the 2010 British Machine Vision Conference.
de Faria NS, et al. Opto-electronic plethysmography: noninvasive and accurate measurement of the volume of the chest wall and its different thoraco-abdominal compartments. Med Sci Tech 2013; 54: 147-150.
Dellaca R, Ventura ML, Zannin E, Natile M, Pedotti A, Tagliabue P. Measurement of total and compartmental lung volume changes in newborns with optoelectronic plethysmography. Pediatric Research 2010; 67(1): 11-16.
Ferrigno G, Carnevali P, Aliverti A, Molteni F, Beulcke G, Pedotti A. Three-dimensional optical analysis of chest wall motion. J Appl Physiol 1994; 77(3): 1224-1231.
Lanini B, Blanchi R, Romagnoli I, Coli C, Binazzi B, Gigliotti F, Pizzi A, Grippo A, Scano G. Chest wall kinetics in patients with hemiplagia. Amer J Respir Crit Care Med 2003; 168: 109-113.
Layton AM, Garber CE, Basner RC, Bartels, MN. An assessment of pulmonary function and ventilation kinematics by optoelectronic plethysmography. Clin Physiol Func Imaging 2011; 31: 333-336.
Layton AM, Moran SL, Garber CE, Armstrong HF, Basner RC, Thomashow BT, Bartels MN. Optoelectronic plethysmography compared to spirometry during maximal exercise. Respir Physiol & Neurobiology 2013; 185: 362-368.
Lo Mauro A, D’Angelo MG, Romei M, Motta F, Colombi D, Comi GP, Pedotti A, Marchi E, Turconi AC, Bresolin N, Aliverti A. Abdominal contribution to tidal volume as an early indicator of respiratory impairment in Duchenne muscular dystrophy. Eur Respir J 2010; 35: 1118-1125.
Parreira VF, Vieira DSR, Myrrha MAC, Oessoa IMBS, Kage SM, Britto RR. Optoelectronic plethysmography: a review of the literature. Braz J Phys Ther 2012; 16: 439-453.
Romagnoli I, Lanini B, Binazzi B, Bianchi R, Coli C, Stenardi L, Gigliotti F, Scano G. Optoelectronic plethysmography has improved our knowledge of respiratory physiology and pathophysiology. Sensors 2008; 8: 7951-7972.
Viera DSR, Hoffman M, Pereira DAG, Britto RR, Parreira VF. Optoelectronic plethysmography: intra-rate and inter-rater reliability in healthy subjects. Respir Physiol & Neurobiology 2013; 189: 473-476.
Vogiatzis I, Georgiadou O, Golemeti S, Aliverti A, Kosmas E, Kastanakis E, Geladas N, Koutsoukou A, Nanas S, Zakynthinos S, Roussous Ch. Patterns of dynamic hyperinflation during exercise and recovery in patient with severe chronic obstructive pulmonary disease. Thorax 2005; 60: 723-729.
Wang HK, Lu TW, Liing RJ, Shih TF, Chen SC, Lin KH. Relationship between chest wall motion and diaphragmatic excursion in health adults in supine position. J Formos Med Assoc 2009; 108)(7): 577-586.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
