The March 1, 2014 issue of the American Journal of Respiratory and Critical Care Medicine had an article on the use of the Lung Clearance Index (LCI) with bronchiectasis. The study showed that the LCI was as good as high-resolution computed tomography and more sensitive than FEV1 when assessing changes in airway status. This is one of the few articles I’ve seen on the LCI that was specifically about adults and wasn’t about cystic fibrosis.
So what is the LCI and how is it measured?
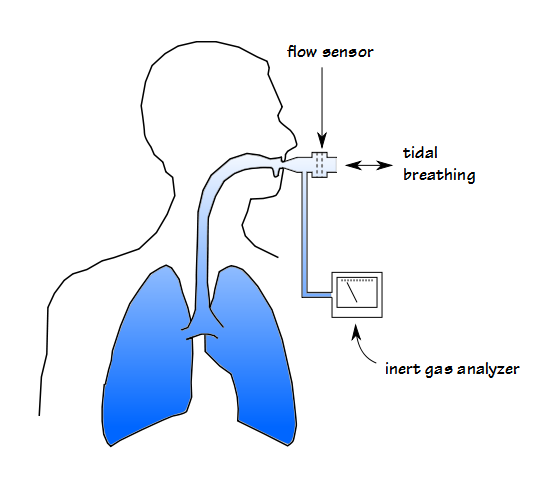
When lung tissue and airways are normal, inhaled gas is distributed evenly throughout the lung and the mixing and turnover of alveolar gas is relatively rapid. When airway obstruction is present gas distribution tends to becomes more uneven and the mixing and turnover takes longer. The Lung Clearance Index (LCI) is a way to measure these ventilation inhomogeneities and is basically a description of how much ventilation is required to completely clear the FRC. It was first described by Margaret Becklake in 1952 but has languished for many years. It has been revived in the last decade or so, particularly because it requires only tidal breathing which allows it to be measured in infants and children.
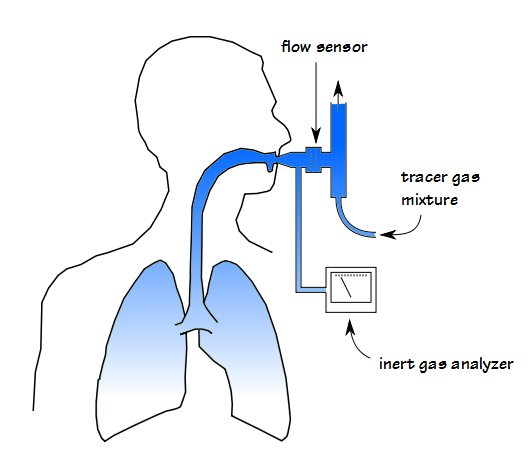
The measurement process is called an Inert Gas Multi-Breath Washout. It uses an open circuit and requires a tracer gas that is both inert and relatively insoluble and for these reasons has been primarily limited to helium, nitrogen and sulfur hexafluoride (SF6) although methane and argon could potentially be used as well.
At the start of the test, the tracer gas must be well distributed throughout the lung which means that for all gases except nitrogen there needs to be a wash-in period (although there of course needs to be a prolonged period of room air breathing between nitrogen washout tests).
The tracer gas mixture is breathed until 30 or 60 seconds after the inspiratory and expiratory concentrations have equalized (ERS/ATS statement says 5 minutes for adults and 4 minutes for children). The patient is then detached from the tracer gas source at end-exhalation and the washout period begins (mechanically, this process is reversed for N2 washout since wash-in occurs while breathing room air and the patient needs to breath 100% oxygen during the washout period).
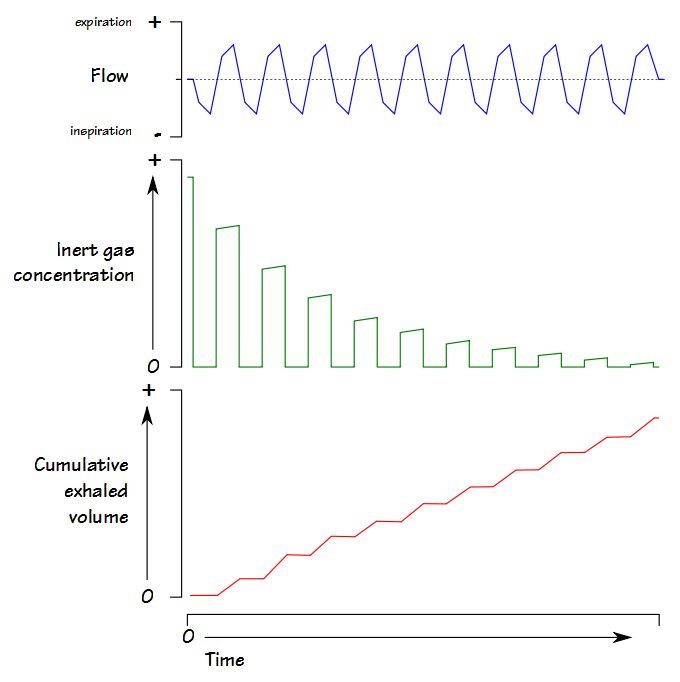
With each succeeding tidal breath, the tracer gas is leaves the lung.
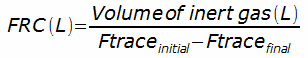
Exhaled volume is accumulated and the test continues until the exhaled gas concentration is 1/40th the initial concentration for three consecutive tidal breaths. The exhaled tracer gas volume is integrated from the flow and gas analyzer signals and FRC is calculated from:
where:
Ftrace = fractional concentration of tracer gas.
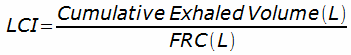
and the Lung Clearance Index is then calculated from:
The Cumulative Exhaled Volume is expressed as liters, BTPS and corrected for system deadspace.
FRC tends to be lower when measured with SF6 than with N2. This is likely due to the fact that SF6 must be washed-in before it is washed-out and it may not completely equilibrate with the poorly ventilated parts of the lung. Despite this there doesn’t seem to be a particularly significant difference in LCI values based on which gas is used.
LCI testing may take a prolonged period of time and this is partly because both the wash-in and the wash-out periods require at least 5 minutes each but also because the LCI test should be performed several times in order to ensure that repeatable results have been obtained. Given the length of time that patients are on a mouthpiece leaks are a potential problem and for this reason it is recommended that results with an FRC 10% greater than the mean should be discarded.
Most studies of LCI have presented grouped results:
LCI (SD), Children:
| Ref: | Gas: | Normal: | Cystic Fibrosis: | Asthma: |
| [A] | SF6 | 6.45 (0.49) | 11.53 (2.86) | |
| [C] | SF6 | 6.33 (0.48) | 8.33 (2.48) | |
| [E] | SF6 | 6.19 | 10.05 | |
| [E] | N2 | 6.81 | 11.29 | |
| [F] | SF6 | 7.2 (0.3) | 8.4 (1.5) | |
| [H] | SF6 | 6.24 (0.47) | 6.69 (0.91) |
LCI (SD), Adults:
| Ref: | Gas: | Normal: | Cystic Fibrosis: | Asthma: | Bronchiectasis: |
| [B] | SF6 | 7.21 (0.26) | |||
| [D] | SF6 | 6.7 (0.4) | 13.1 (3.8) | ||
| [I] | SF6 | 9.1 (2.0) | |||
| [J] | N2 | 7.19 (0.53) | |||
| [K] | N2 | 6.02 (0.31) | 6.26 (0.42) |
A recent study [G] however, has published a reference equation for LCI in healthy children (aged 2 weeks to 19 years):
Since LCI is referenced to an individual’s measured FRC there doesn’t seem to be a significant gender difference in results. It has been noted that among children LCI decreases with increasing age and height, and that among adults there seems to be a slight increase with age.
It’s not particularly clear to me why so much of the research on LCI has been done using SF6. I realize that there are additional measurements that can be made when you compare washouts with different gases (specifically it is possible to determine if the ventilation inhomogeneity is occurring at the level of the acinus or higher up in the peripheral airways), but for the LCI itself nitrogen washout seems to work as well as any of the other inert gases. This is important for the future of LCI testing since SF6 is a greenhouse gas that has not been approved for clinical applications in the United States and helium is becoming scarce and progressively more expensive.
For the last decade or so there has been a greater emphasis on early intervention for children with cystic fibrosis and a number of studies have shown that there can be significant changes in LCI without notable changes in FEV1. It’s not clear to me how the LCI measure differs from the phase III slope of the single-breath nitrogen washout, however, and these two tests have not been performed in the same patients. One major advantage of the LCI is that it only requires tidal breathing which makes it particularly suited for testing children.
Interestingly, it doesn’t appear that LCI results for individuals with asthma are substantially different from healthy controls. This is not necessarily surprising since the LCI is sensitive primarily to the peripheral airways and asthma resides in the larger airways. There are many patients with COPD however, that do not have significant changes in spirometry from visit to visit and yet report significant changes in how well they feel. Because the LCI is a measurement of ventilation inhomogeneity rather than expiratory flow rates it would interesting to see if it (or the phase III slope of the single-breath nitrogen washout) tracks patient status better than spirometry in these cases.
Theoretically the LCI could be measured by any test system that is able to perform N2 washout lung volumes. Despite the fact that both types of testing measure FRC the maneuvers are not the same however, and the software requirements are substantially different. At the present time there are no commercial test systems that are able to measure the LCI although this may change since the ERS/ATS released guidelines in 2013 that specifically addressed the technical and software requirements for LCI measurements (and if you read between the lines on their websites a couple of manufacturers are at least considering adding the LCI to their test systems).
The FEV1 and the FEV1/FVC ratio have been the primary focus for the detection and monitoring of airway obstruction for decades. This is in part understandable since the Forced Vital Capacity is a relatively simple and repeatable test that requires minimal equipment. Spirometry is not sensitive to all forms of airway obstruction and it has become evident in a variety of lung diseases that changes (or the lack of changes) in FEV1 does not match either disease progression or status. Ventilation inhomogeneity may be one of the missing pieces in this puzzle and as such, the LCI deserves more extensive research in a wider variety of lung diseases and age groups.
References:
[A] Aurora P, Gustafsson P, Bush A, Lindbla A, Oliver C, Wallis CE, Stocks J. Multiple breath inert gas washout as a measure of ventilation distribution in children with cystic fibrosis. Thorax 2004; 59: 1068-1073.
Becklake MR. A new index of the intrapulmonary mixture of inspired air. Thorax 1952; 7: 111-116.
[B] Fuchs SI, Buess C, Lum S, Kozlowska W, Stocks J, Gappa M. Multiple breath washout with a sidestream ultrasonic flow sensor and mass spectrometry. A comparative study. Pediatric Pulmonology 2006; 41: 1218-1225.
[C] Gustafsson PM, Aurora P, Lindblad A. Evaluation of ventilation maldistribution as an early indicator of lung disease in children with cystic fibrosis. Eur Respir J 2003; 22: 972-979.
Gustafsson PM, De Jong PA, Tiddens HAWN, Lindblad A. Multiple-breath inert gas washout and spirometry versus structural lung disease in cystic fibrosis. Thorax 2008; 63(2): 129-134.
[D] Horsley AR, Gustafsson PM, Macleod KA, Saunders C, Greening AP, Porteous DJ, Davies JC, Cunningham S, Alton EWFW, Innes JA. Lung clearance index is a sensitive, repeatable and practical measurement of airways disease in adults with cystic fibrosis. Thorax 2008; 63(2): 135-140.
[E] Jensen R, Stanojevic S, Gibney K, Slazar JG, Gustafsson P, Subbarjo P, Ratjen F. Multiple breath nitrogen washout: a feasibile alternative to mass spectrometry. PLOS One 2013; 8(2): e56868.
[F] Lum S et al. Early detection of cystic fibrosis lung disease: multiple-breath washout versus raised volume tests. Thorax 2007; 62: 341-347.
[G] Lum S et al. Age and height dependence of lung clearance index and functional residual capacity. Eur Respir J 2013; 41: 1371-1377.
[H] Maclead KA, Horsley AR, Bell NJ, Greening AP, Innes JA. Ventilation heterogeneity in children with well controlled asthma with normal spirometry indicates residual airways disease. Thorax 2009; 64: 33-37.
Robinson PD et al. ERS/ATS Consensus Statement: Consensus statement for inert gas washout measurement using multiple- and single-breath tests. Eur Respir J 2013; 41: 507-522.
[I] Rowan SA et al. Lung Clearance Index is a repeatable and sensitive indicator of radiological changes in bronchiectasis. Am J Resp Crit Care Med 2014; 189: 586-592.
[J] Singer F, Houltz B, Latzin P, Robinson P, Gustafsson P. A realistic validation study of a new nitrogen multiple breath washout system. Plos One 2012; 7(4): e36083.
[K] Verbanck S, Paiva M, Schuermans D, Hanon S, Vincken W, Van Muylem A. Relationship between the lung clearance index and conductive and acinar ventilation heterogeneity. J Appl Physiol 2012; 112: 782-790.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License