Recently I was reviewing a spirometry report and noticed that the FVC was below normal. A low FVC can suggest a restrictive lung disease but the reported expiratory time was only about 4 seconds. I took a look at the graphics included with the report and the volume-time curve showed the effort ended well before 6 seconds so my first thought was that the reduced FVC was more likely because of suboptimal patient effort than anything else.
I always try to review spirometry results whenever there is anything questionable so I pulled up the raw test results and immediately saw that the reported FVC was actually a composite. The ATS-ERS statements on Spirometry and Interpretation say that the highest VC regardless of which test it came from (which even includes the slow vital capacity test from lung volume measurements and the inspiratory volume from a DLCO) should be used when reporting spirometry results. In this case the FVC came from one effort, the FEV1 and everything else came from a different effort. The interesting thing was that the effort the FVC came from was about 10 seconds long which shows it actually was an adequate effort. The FEV1 effort on the other hand was only about 4 seconds long and showed an abrupt and early termination of exhalation.
The technician who performed the tests selected the correct efforts to make a composite. The patient had made five spirometry efforts and the selected FVC was significantly larger than all of the other efforts but the FEV1 from the same effort was significantly lower than several other efforts. Our criteria for selecting FEV1 does not just go by the largest FEV1, we also look at the peak flow (PEF) and whether there has been any back extrapolation and the effort the FEV1 came from had the highest peak flow and no back extrapolation. So, a good choice had been made on both efforts.
When it comes to selecting values from different spirometry efforts there are only a limited number of results that our lab software allows us to mix and match. The FVC, the FEV1 and the graphics (flow-volume loop and volume-time curve which are linked to each other) can all be selected individually, but everything else, which includes the expiratory time, PEF, FEF25-75, MEF50 etc. etc. can only be selected as a group.
Our policy when selecting the FVC from one effort and the FEV1 from another is that the flow-volume loop and all the ancillary values go along with the FEV1 which is mainly because these include the values that indicate the quality of the FEV1. This makes sense for PEF and (within limits) the flow-volume loop, but less so for all of the other values. The most obvious mismatch is that the expiratory time belongs with the FVC, not the FEV1. For many, if not most, of the other ancillary values it is not clear at all which effort they should be selected from.
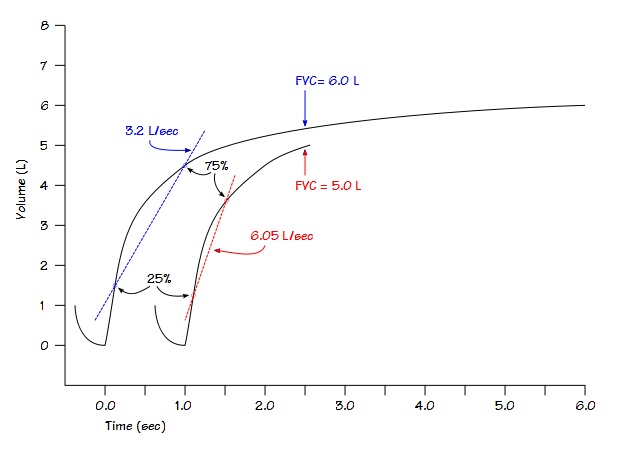
For example, the FEF25-75 will almost always be overestimated when it is taken from an effort with a short exhalation time. This is because the 25% and 75% points are based on the vital capacity, and when a spirometry is shorter than it should have been, these points will occur earlier when flow rates are higher.
The same consideration applies to MEF25, MEF50, MEF75, MIF25, MIF50 and MIF75 since these values are also determined in relation to the vital capacity. That being said, that doesn’t mean that the FEF25-75 and the other ancillary values should be taken from the effort with the largest FVC either. All of these values reflect expiratory flow rates and are presumably the highest values the patient can attain. There is nothing that says that a spirometry effort with the largest vital capacity volume was performed with maximal flow rates as well.
The ATS-ERS statement on Spirometry says the FEF25-75 should be taken from the effort with the highest combined FVC and FEV1. I understand the intent but I also think this recommendation was made without consideration of those times when when there are significant differences in FVC and FEV1 from test to test or when the VC comes from a test other than a forced vital capacity. Even so, if this guideline was followed, it would be possible to report a composite effort with the FVC from one effort, the FEV1 from another and the FEF25-75 from another. Interestingly, although the ATS-ERS statements discuss the performance of Peak Flow and Flow-Volume Loops, there are no specific guidelines for selecting them when a composite is made.
My particular quandary is that we cannot select the FEF25-75, peak flow and expiratory time separately. They come as a group and any choice is going to be a compromise. Fortunately, since we don’t routinely report FEF25-75 or any of the other ancillary flow values this simplifies the process somewhat. My lab’s decision has been that since PEF is used as part of the selection process for FEV1 and is also a reported value that is used to compared a patient’s personal peak flow readings, it trumps expiratory time and the reported value (along with everything else, like it or not) therefore comes from the FEV1 effort. For similar reasons, the flow-volume loop is associated more with FEV1 and peak flow, so it also comes from the FEV1 effort.
Our inability to select what we think are the most appropriate test results when making a composite is primarily due to limitations in our lab’s testing software, but I suspect this is a similar problem for all systems that allow the FVC and FEV1 to be selected from different spirometry efforts. The ATS-ERS statements offer no guidelines about selecting FEF25-75, peak flow and expiratory time when composite spirometry efforts are created so it’s up to each equipment manufacturer to decide what can and can’t be selected other than the FVC and the FEV1.
I think there are good reasons why PEF and flow-volume loop should go along with the FEV1. I also think that expiratory time should come from the largest FVC (ignoring of course those times when it comes from lung volume or DLCO tests). When it comes to FEF25-75 and the other ancillary flow values, I don’t think there can be a clear answer, and that in fact any selection at all is likely going to result in reporting values that are in one way or another incorrect (and is another reason for not reporting them in the first place).
One final issue I have with this whole process is that there is nothing whatsoever on our final report that indicates that the FVC and FEV1 came from different efforts. If I hadn’t decided to pull up the raw test data I wouldn’t have known. This information doesn’t necessarily need to be on a final report, but it’s not even an option for us. Since the final report (in PDF format) is the primary tool for reviewing (and eventually will also be for signing) tests for my lab, I think this is a problem.
The ATS-ERS statements on Spirometry and Interpretation say that the largest vital capacity should be used to report the FEV1/VC ratio. I am in complete agreement with this since I think it is best way to implement the intent of the forced vital capacity maneuver which is to determine the presence of airway obstruction. The devil is in the details however, since a spirometry test is not just about VC and FEV1, but also about peak flow, FEF25-75, expiratory time, the flow-volume loop, the volume-time curve and other values. The lack of guidelines and certain inconsistencies in the selection process for these other values makes it likely that incorrect or misleading results can and will be reported.
I would like to hope that these issues (as well as many others) will be addressed in the next ATS-ERS statements on Spirometry and Interpretation, but we’ll have to wait and see. In the meantime reviewers need to remember that the criteria used to select FVC and FEV1 may be inconsistent with those needed to select the other reported values; that limitations on the selection process may be imposed by testing software; that the graphics don’t necessarily match the numerical values; and finally the fact that a composite effort was created at all may be hidden from view by reporting limitations.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of Lung Function Testing: Standarisation of spirometry. Eur Respir J 2005; 26: 319-338.
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of Lung Function Testing: Interpretive strategies for lung function tests. Eur Respir J 2005; 26: 948-968.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.