During exhalation air flow occurs because of the pressure difference between the alveoli and the surrounding atmosphere. The increase in alveolar pressure acts to compress the air inside the lung and because of this compression the decrease in lung volume during exhalation is always going to be greater than the volume of exhaled air. This effect is known as Thoracic Gas Compression (TGC).
The flow rate that occurs for a given alveolar pressure depends primarily on airway resistance. When an individual has airway obstruction their airway resistance is increased and they often attempt to increase their expiratory flow by increasing the amount of force they apply during exhalation. This increased force further compresses the air inside the lung and increases TGC. Numerous researchers have shown that there is usually a substantial differences in TGC between subjects with normal lungs and those with airway obstruction.
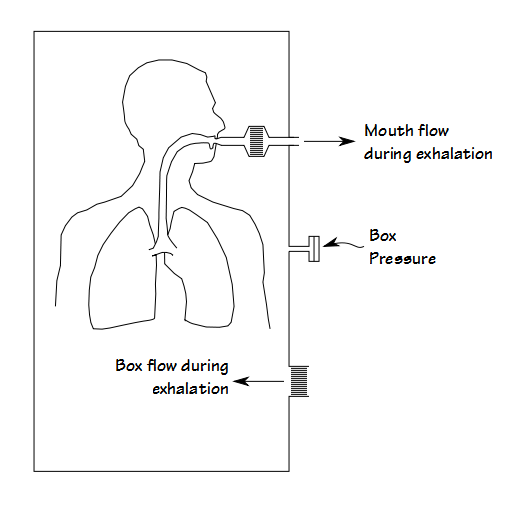
Routine spirometry and lung volume tests cannot measure thoracic gas compression. It can only be measured in a special kind of plethysmograph. Unfortunately the nomenclature for this type of plethysmograph is a bit muddy and it is variously known as a transmural, constant pressure, volume-displacement or flow plethysmograph (I prefer volume-displacement because I think this sums up its mode of operation most succinctly). In this type of plethysmograph the subject breathes in and out through an opening in the box. The expansion and contraction of their lungs causes air to flow in and out of the box through a separate opening. The pressure inside the plethysmograph is monitored and used to compensate for any delays in box flow.
Because the air in the lung is compressed during a forced exhalation this means that more air flows into the plethysmograph than flows out through the subject’s mouth. These two signals are compared to determine the difference in flow rates.
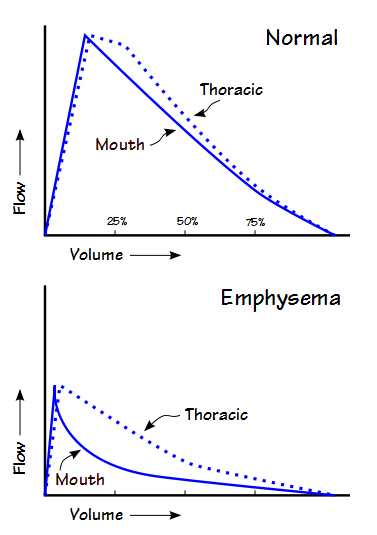
Largely because it is difficult to compare an entire curve, researchers have tended to report the difference in expiratory flow rates at specific lung volumes. One approach as been to use the flow rates at 25%, 50% and 75% of vital capacity. Another has been to correct and re-calculate FEV1 for TGC.
Regardless of how it is measured investigators have shown that the difference between mouth and thoracic flow rates increase with increasing airway obstruction and decrease when it lessens. This has been shown in patients with asthma, both during a methacholine challenge and after bronchodilation. Patients with emphysema tend to have a large difference between mouth and thoracic flow rates, particularly at high lung volumes, and not unsurprisingly, patients with interstitial lung disease tended to have the least discrepancy between the two. Although the difference between mouth and thoracic flow rates is usually highest close to TLC, obese patients tended to have significant differences even at lower lung volumes.
Of note, one group of researchers used the difference between exhaled mouth and box volumes to estimate alveolar pressure and thereby continuously calculate airway resistance during a forced exhalation. This seems to be an elegant answer to the accepted practice of measuring airway resistance but there must be a flaw to this approach that I am not aware of, either in its basic assumptions or to its clinical relevance, since this technique does not appear to have been used by any but the original researchers.
The mechanical difference between the more common constant-volume and the volume-displacement plethysmograph is relatively small and plethysmographs capable of both modes of operation have been available since at least the 1980’s. They are still available from one or more different equipment manufacturers and are equipped with software to measure mouth and thoracic flow-volume loops and to overlay them. So why isn’t this technique more commonly known and used?
Although there is a general correlation between the degree of airway obstruction and the difference in thoracic and mouth flow rates, I think the key factor for its lack of general adoption is that it is not individually predictable. This is due in part to differences in patient effort, static recoil and available muscle strength. It may also be due in part to the site and the nature of the airway resistance as well. For this reason there are no normal values and although there are statistically significant differences following bronchodilation for a study group as a whole that is different from knowing what’s the significant difference for an individual. In addition there has been no standardization in how it is measured (i.e. flow at 50% vs corrected FEV1 as well as the fact that some researchers report the volumes at which flows are measured either relative to TLC or relative to RV which means that the flow rates at 25% from one researcher can be the same those as 75% from another). A final barrier is that measurement of TGC requires specialized equipment that is unlikely to be generally available.
Thoracic gas compression occurs to one extent or another in everyone. There is a general correlation between airway obstruction and the degree of TGC. The amount of an individual’s TGC or changes in TGC following treatment or therapy may well be clinically relevant but the lack of normal values means that its use should be approached with caution.
References:
Coates AL, Peslin R, Rodenstein D, Stocks J. Measurement of lung volumes by plethysmography. Eur Respir J 1997; 10: 1415-1427.
Coates AL, Desmond KJ, Demizio D, Allen P, Beaudry PH. Sources of error in flow-volume curves. Effect of expired volume measured at the mouth vs that measured in a body plethysmograph. Chest 1988; 94: 976-982.
Pellegrino R, Confessore P, Bianco A, Brusasco V. Effects of lung volume and thoracic gas compression on maximal and partial flow-volume curves. Eur Repir J 1996; 9: 2168-2173.
Piirila PL, Hodgson U, Wuorimaa T, Smith HJ, Sovijarvi ARA. Thoracic gas compression during forced expiration in patients with emphysema, interstitial lung disease and obesity. BMC Pulmonary Medicine 2014; 14: 34.
Sharafkhaneh A, Officer TM, Goodnight-White S, Rodarte JR, Boriek AM. Novel method for measuring effects of gas compression on expiratory flows. Am J Physiol Regul Integ Comp Physiol 2004; 287: R479-R484.
Sharafkchaneh A, Babb TG, Officer TM, Hananla NA, Sharafkhaneh H, Boriek AM. Confounding effects of thoracic gas compression ob measurement of acute bronchodilator response. Am J Resp Crit Care Med 2007; 175: 330-335.
Stanescu D, Veriter C, Van Leemputten R, Brasseur L. Constancy of effort and variability of maximal expiratory flow rates. Chest 1979; 76(1): 59-63.
Walamies MA. Thoracic gas compression profie during forced expiration in health and asthmatic schoolchildren. Respir Med 1998; 92: 173-177.
Zamel N, Jones JG, Bach SM, Newburg L. Analog computation of alveolar pressure and airway resistance during maximum expiratory flow. J Appl Physiol 1974; 36(2): 240-245.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.