Over the last couple of years I’ve run across a number of test systems that do not include tidal loops along with the maximal flow-volume loop. I’ve wondered why this was done and because of this I’ve thought a lot about tidal flow-volume loops and what additional information, if any, they add to spirometry interpretation.
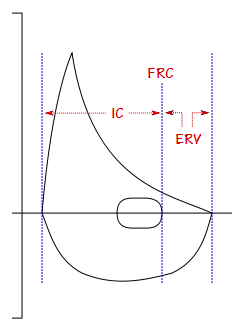
One of my thoughts has been about the relationship between obesity and the IC and ERV. FVC and TLC are often reasonably preserved even with relatively severe obesity. FRC, on the other hand, is often noticeably affected with even minor changes in BMI (and interestingly this applies to reduced as well as elevated BMI’s). When FRC decreases because of obesity the IC usually increases and the ERV decreases and for this reason the IC/ERV ratio has been suggested as a way to monitor changes in FRC without having to actually measure lung volumes.
IC and ERV are not measured as part of spirometry but the position of the tidal loops gives at least a general indication of their magnitude and I’ve noticed that there’s a moderately good correlation between BMI and the position of the tidal loop.
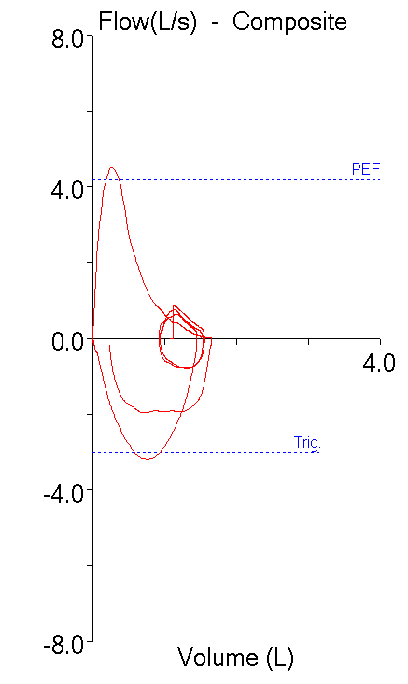
With this in mind, I see up to a dozen reports a week with restrictive-looking spirometry (i.e. symmetrically reduced FVC and FEV1 with a normal FEV1/FVC ratio) on patients with a diagnosis of asthma. This is nothing new and there have probably been at least 10 articles in the last decade about the Restrictive Spirometry Pattern (RSP). Interpreting these kinds of spirometry results is always problematic, particularly when there are no prior lung volume measurements to rule-in or rule-out restriction. I’ve noticed however, that patients with a restrictive spirometry pattern almost always have the tidal loop on the far right-hand side of the flow-volume loop (zero or near zero ERV). For example:
| Observed: | %Predicted: | |
| FVC: | 1.65 | 74 |
| FEV1: | 1.21 | 73 |
| FEV1/FVC: | 73 | 100 |
But there doesn’t seem to be any relationship between this observation and the patient’s BMI and in fact, this is seen even when BMI is normal or somewhat reduced.
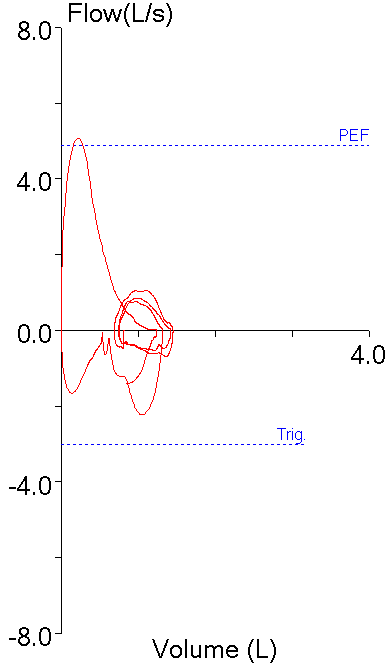
The patient in the above example however, also had a DLCO test and the Inspired Volume (IVC) was 1.95 L (87% of predicted FVC). Using the IVC to re-calculate the FEV1/VC ratio showed it to be 62.1 or 85% of predicted (LLN = 89). So, instead of possible restriction, this shows that the patient had mild airway obstruction and that the reduced FVC was due to gas trapping.
In addition, I’ve reviewed the flow-volume loops from a number of patients with known lung restriction and found that the tidal loop was almost always more centrally placed. But when I look at restrictive spirometry pattern flow-volume loops a certain fraction of them has a tidal loop that is to the right and outside the maximal flow-volume loop.
I’d be the first to admit that this flow-volume loop could be the result of the patient leaking around the mouthpiece. I’d even argue that expiratory leaks are more likely to occur than inspiratory leaks and that this could explain why the end of expiration is to the left of the beginning of the inspiration (i.e. FIVC > FVC). However, after reviewing a number of RSP loops I saw that this was occurring in somewhere around a quarter of them and that seems to be a bit too many to attribute to leaking, particularly since the same thing doesn’t seem to be happening in patients with restriction.
The alternative explanation therefore is that this is actually a more extreme form of gas trapping. Confirmation of gas trapping usually requires lung volume measurements (i.e. elevated FRC and RV) but many patients with a restrictive spirometry pattern do not get lung volume measurements, or if they did it was well in the past and there is no overwhelming need to repeat them.
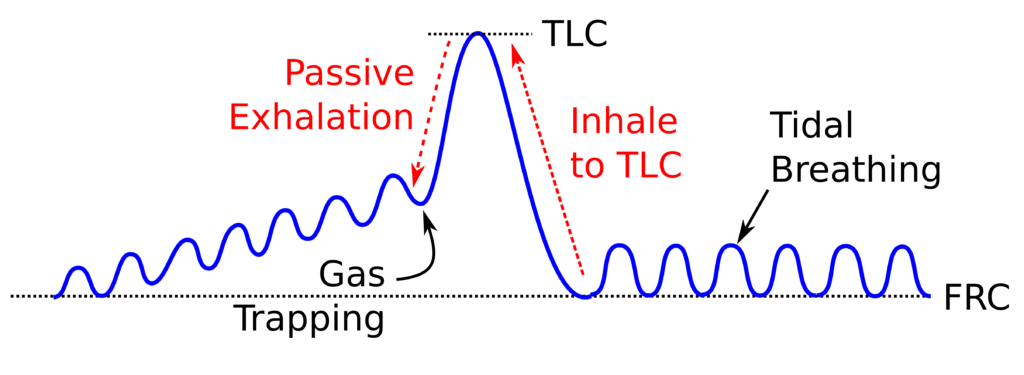
But you don’t necessarily need lung volume measurements to determine the presence of gas trapping. Back in the 1970’s and 1980’s when we had water-seal volume displacement spirometers with a kymograph there was a relatively simple test to detect gas trapping. Specifically, we’d have a patient start with tidal breathing and then have them take a deep breath in and then ask them to return to normal breathing. Patients without gas trapping would have the end-exhalation level of their tidal breathing return to FRC almost immediately, while those with gas trapping would take a number of breaths before this happened. This test wasn’t particularly qualitative but it clearly differentiated between patients with gas trapping and those without.
This kind of testing however, usually can’t be performed on current test systems, primarily due to software limitations, and the more common approach is to compare the FVC and SVC.
So I have strong suspicions that patients with a restrictive spirometry pattern and whose tidal flow-volume loops show an essentially zero ERV are likely gas trapping. These (and probably other) patients should probably perform an SVC maneuver in order to make this more evident. Although I’d like to get our techs to perform SVC maneuvers as part of routine spirometry more frequently there are at least a couple of problems that make this more difficult than it ought to be.
First, almost all of our routine spirometry is performed as part of the pulmonary physician clinics which are located several buildings away from the main PFT Lab. We have a couple screening spirometry systems there and I would like to say we can give every patient the time that they need but realistically given the number of patients seen in clinics and our resources the amount of time we can give to each patient is limited. Adding an SVC maneuver to routine spirometry could as much as double the amount of time spent with a patient and that’s time we often don’t have.
Next, even when we have the time to perform both FVC and SVC maneuvers our lab software will not calculate the FEV1/SVC ratio and will not include it in a report. The best we can do is to report the SVC and then manually calculate the FEV1/SVC ratio and put it in the notes.
Note: In addition I know that there are at least some spirometry systems do not permit an SVC to be performed. I don’t know how widespread this problem is but I have an older (~15 years) office spirometer that I use in a weekly free spirometry session in my community and it does not have an SVC test module.
And although I feel crass for having to mention this, you can perform an FVC and be reimbursed or you can perform an SVC and be reimbursed but if you perform both and FVC and an SVC you will only be reimbursed for the FVC. Since an FVC and SVC probably only need to be performed a relatively small number of patients I don’t have a problem with this (we already perform upright and supine spirometry regularly and aren’t reimbursed for the supine portion) but there are many labs where this might be an issue.
Finally, there remains a number of open questions about interpreting the FEV1/SVC ratio. In one sense it’s a no-brainer when a subject with a reduced FVC and a normal FEV1/FVC ratio can be shown to have a normal SVC with a reduced FEV1/SVC ratio. At the same time however, the FEV1/SVC ratio has not been studied in a normal population so its Mean and LLN values are at best speculative.
Gas trapping has significant clinical implications and I strongly suspect that it is far more common than is generally realized. A major reason for this is our approach to routine spirometry (i.e. FVC only) which in turn has lead to corresponding limitations in many of our test systems. We need to be more open towards performing additional testing despite problems in time management, software limitations and reimbursement in order to detect gas trapping in our patients.
It’s been over a decade since the ATS/ERS interpretation guidelines advocated the use of the FEV1/VC ratio (using the largest VC whatever the source). Although the recent ATS reporting guidelines mentions:
“Measurement of slow VC and calculation of FEV1/VC are a useful adjunct in patients with suspected airflow obstruction.”
there are no still guidelines about when an SVC should be performed as part of routine spirometry. It could be argued that an SVC should be performed in any patient with a reduced FVC but many if not most of those who meet this criteria clearly have airway obstruction and the value of an SVC is limited. More realistically it would probably be best to perform an SVC in only those patients with a reduced FVC and a normal FEV1/FVC ratio.
References:
Brusasco V, Crapo R, Viegi G et al. ATS/ERS task force: Standardisation of lung function testing. Interpretive strategies for lung function tests. Eur Respir J 2005; 26: 948-968.
Graham BL et al. Recommendations for a standardized pulmonary function reports. An American Thoracic Society technical statement. Am J Respir Crit Care Med 2017; 196(11): 1463-1472.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

Richard
We usually did tidal loop captures during exercise and overlay them on FVL done pre-ex. When there was air trapping, the tidal loop would ‘travel’ inside the FVL, sometimes without gaining much volume over the resting tidal loop. When there was no air trapping it was easy to see from the size of the tidal loop when ventilatory maximum was nearing.
Good post, as always.
Hi Richard,
In the above example, this subject does have an increased BMI?
I see this type of loop with thoes that have an elevated BMI, whereas thoes with true restriction (pulmonary and not obesity) find their tidal volume shifted to the left of centre.
In the above example the subject has a normal FEV1/FVC ratio, and that being the case, one has to ask,
How can one have air trapping without obstruction?
The only case that this may appear, would be in a neuromuscular subject. (Normal FEV1/FVC with an elevated RV.
FVL that are peoduced without the tidal breath, fail to capture possible air flow limitation (where the expiration of the FVC cuts through the tidal breath) subjects with obstruction.
In your second loop, I find the only way th is is possibly caused by a leak.
Regards,
Mo
Mo –
No, the patient’s BMI was 25.4. I agree that the tidal loop is shifted right-wards in obese patients and this is something I said in the posting.
I think you’re a bit hung up on the notion that airway obstruction always presents as a reduced FEV1/FVC ratio. That is probably true for 90% of patients with asthma, but about 10% present with restrictive-looking spirometry and this is most likely due to gas trapping. In addition, a number of patients with CHF also have restrictive spirometry with a normal TLC. I agree the tidal loop in the final flow-volume loop could be caused by a leak but why does such a large number of patients with RSP look like this and yet patients with known lung restriction rarely do. There are in fact a number of patients who cannot exhale what they inhale (i.e. FIVC > FVC) because of gas trapping and these will look just like what the final loop looks like.
Regards, Richard
Hi Richard, How do you feel about performing an FVC manoeuver & instructing the patient to reduce the force at the end of the manoeuver when flows become exceptionally low to encourage complete emptying? As this is the effort independent part of the forced expiratory manoeuver & being very careful not to do it too early when less dynamic airway collapse could influence the shape of the curve doesn’t it represent a similar result to FEV1/VC, making any airflow obstruction more obvious on simple spirometry & can be done within the FVC trial thus mitigating the issues of time & software restrictions. I have been using this modified method in some cases from a technical standpoint of patient compliance as i have found it reduces cough & pre-syncope having less force as you approach RV & in turn obtaining more repeatable & accurate data (hopefully!). I look forward to your reply as to whether i am bastardising spirometry!
Kim –
I use this approach when I perform spirometry and coach patients to blast forcibly in the beginning of the FVC maneuver but after a couple seconds change to coaching them to let their air out steadily. I agree with you that it is less stressful for the patient and that I think I get better compliance and reproducibility with this approach. Although this may not meet the exact letter of the ATS/ERS standards for spirometry I think it meets the spirit of them and realistically it gets better quality results.
However, this approach does not necessarily get better results in patients with gas trapping since you are still starting from a maximum inhalation. For these patients an SVC maneuver that starts with a maximal exhalation to RV and then maximal inhalation to TLC is more likely to get a larger VC.
Regards, Richard
Richard, you have made my day! I was quite nervous as i awaited your reply as my respect for your blog is enormous & wondered if i was indeed doing something that goes against the ATS/ERS guidelines, but you have reaffirmed my actions as legitimate. I take your point regarding the SVC from RV to TLC & again you have expanded my knowledge base & got me thinking! Cheers Kim