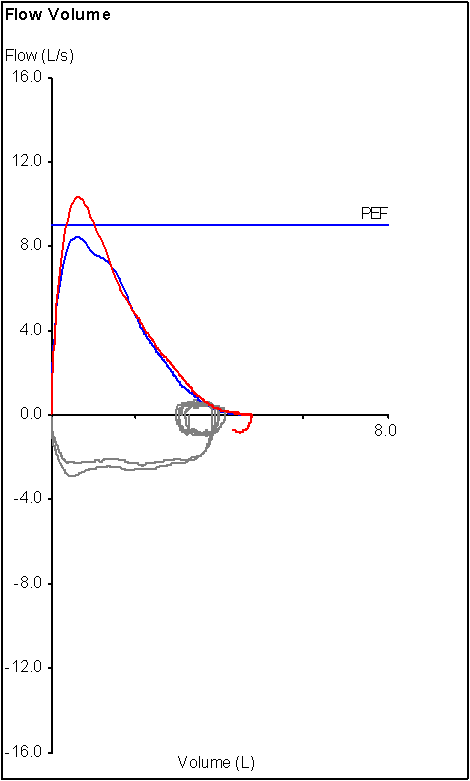
Recently I was discussing a flow-volume loop with one of our pulmonary physicians. His concern was whether the loop, which was from a patient with a cracked hyoid, was showing inspiratory obstruction or not. I had to point out that the inspiratory flows on the loop in question came from the pre-FVC inspiration that started at FRC, not RV, and that we don’t emphasize maximal inspiratory flow at that point in the test, just maximal inspiratory volume and for these reasons the flow-volume loop was not a reliable indicator of inspiratory obstruction.
When we assess flow-volume loops we usually don’t pay a lot of attention to the inspiratory loops from routine spirometry and this is because they aren’t terribly reliable. As with all routine spirometry there are going to be issues with patient performance. Many patients have difficulty performing a maximal inspiratory flow maneuver because they don’t “get it” or will come off the mouthpiece as soon as they have finished exhaling despite repeated coaching. In other instances we have enough problems getting a good expiratory maneuver without even trying to worry about any kind of an inspiratory effort.
More importantly however, is that even when we are able get a patient to perform an adequate inspiratory maneuver we have to report a given spirometry effort based on its maximal expiratory values, not the inspiratory values. Our lab software allows us to mix-and-match expiratory values like FVC, FEV1 and the flow-volume loop from different spirometry efforts but it does not allow us to take the best inspiratory values from one spirometry effort and match them with the best expiratory values from another test. This means that the only time a patient’s best inspiratory values can be reported is when they coincidentally also belong to a spirometry effort with the best expiratory values.
Note: I will mention in passing that the DOS version of our lab software that we used over 15 years ago allowed us to mix-and-match inspiratory and expiratory values from different spirometry efforts. This feature (along with several other useful features) didn’t make the transition to the Windows version of the software. Progress isn’t always progress!
What this means is that if we took the inspiratory flow-volume loops from routine spirometry at face value we would be reporting a lot of false-positives for inspiratory airway obstruction. Our work-around for this problem is to ask our pulmonary physicians to specifically request an inspiratory flow-volume loop when they suspect inspiratory airway obstruction. This allows us to focus on obtaining and selecting the best inspiratory effort without worrying about the expiratory values or at least to separate the tests where we emphasize one feature over another.
When we do attempt to obtain an inspiratory FVL it is easy to reject a clearly suboptimal maneuver but at what point is an inspiratory effort acceptable? Interestingly, although the ATS/ERS Standards for Spirometry states that the expiratory effort of an FVC maneuver should be
“followed by a rapid full inspiration with maximum effort back to TLC”
it does not indicate how to assess the quality or reproducibility of the inspiratory maneuver. In fact, other than noting that MIF mean Maximal Inspiratory Flow the ATS/ER Spirometry Standards do not discuss any of the instantaneous flow measurements (MIF25%, MIF50%, MIF75%, MEF25%, MEF50% and MEF75%). There is some discussion on the use of the inspiratory flow-volume loop in the ATS/ERS Statement on Interpretation but the only reference to quality assessment is
“It is critical that the patient’s inspiratory and expiratory efforts are near maximal and the technician should confirm this in the quality notes.”
I guess this is a “we’ll know it when we see it” type of thing since otherwise the criteria by which the maximal inspiratory flow and maximal inspiratory volume are determined remain unclear.
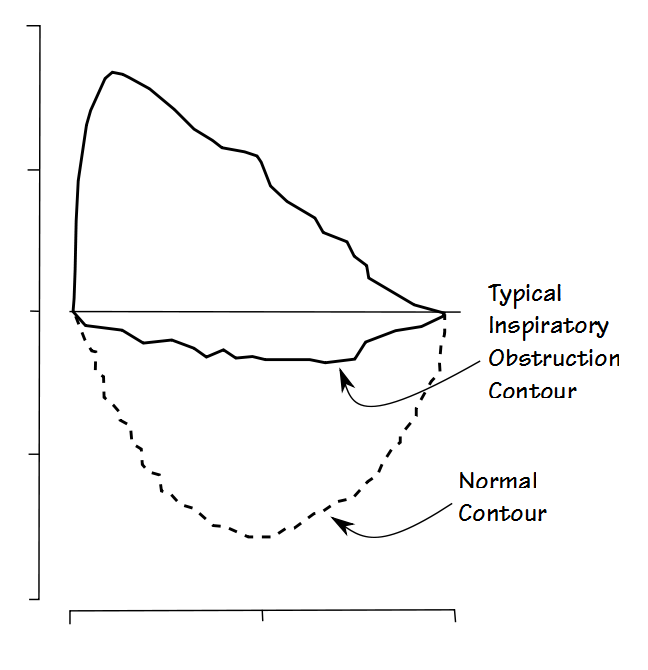
Once you have an inspiratory flow-volume loop with (presumably) good quality however, it is the contour that is usually most informative.
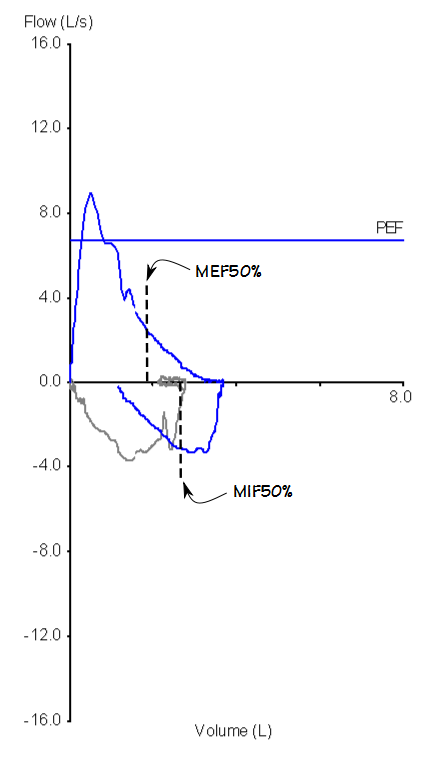
Contour is one of those things where everybody “knows” what inspiratory obstruction looks like but is difficult to describe otherwise. The measured values that have been used most often to describe inspiratory obstruction are the Maximal Inspiratory Flow rate at 50% of the vital capacity (MIF50%) and the ratio between the Maximal Expiratory and Inspiratory Flow rates at 50% of the vital capacity (MEF50%/MIF50% ratio).
Note: The average flow between 25% and 75% of the FIVC (the FIF25%-75%) and the Forced Inspired Volume in 1 second (FIV1) have also been suggested as also being sensitive to inspiratory obstruction but no thresholds or LLN’s have been proposed for them.
There is a general consensus that inspiratory obstruction is present when:
MIF50% < 100 LPM (1.67 L/sec)
MEF50%/MIF50% > 1.0
but other than the fact that these values come from a single study performed in 1975 and have been copied verbatim by most subsequent studies there are at least a couple problems with these values.
As already mentioned the best MIF50% and MEF50% may come from different spirometry efforts. One study showed that almost two-thirds of the time the highest PIF and MIF50% occurred in a different spirometry effort than the one selected for best expiratory values. Another study showed that in a population of patients with inspiratory obstruction the MEF50%/MIF50% ratio decreased from 3.07 to 1.77 when the spirometry effort with the best combined MIF50% and MEF50% was selected rather than the best FVC and FEV1. For this reason when inspiratory obstruction is being evaluated it is apparent that the spirometry selection criteria needs to be different than that used for normal spirometry. One study proposed that the inspiratory effort with the best FIVC + MIF50% + PIF should be selected for reporting and in the absence of an official ATS/ERS statement this appears to be a useful set of criteria.
The usefulness of the MEF50%/MIF50% ratio however, also presumes that the MEF50% is relatively normal but the MEF50% will be reduced when airway obstruction (i.e. Asthma, COPD) is present. MIF50% also tends to decreases when airway obstruction is present but even so the MEF50%/MIF50% ratio will be tend to be lower than it “should be” even when inspiratory obstruction is also present.
Next, MIF50% and MEF50% should be measured at 50% of the vital capacity, but which vital capacity? Exhaled or inhaled? Relating inspiratory flow to the exhaled vital capacity probably makes the most sense and a review of the literature indicates that this is the most common (but interestingly not completely universal) approach but when I checked our lab software I found that it was measuring the MIF50% using the inspired vital capacity and the MEF50% using the exhaled vital capacity. As well as making the MIF50% questionable this also calls into question the validity of the reported MEF50%/MIF50% ratio in our and possibly other test systems.
An additional point to this is that as already mentioned the ATS/ERS Standard for Spirometry states that the inspiratory effort should follow the expiratory effort. At least one study showed that FIVC, MIF50% and PIF were larger when the inspiratory effort preceded the expiratory effort or was performed separately. This is not an option for us since my lab’s software will only calculate the MIF, PIF and FIVC values when the inspiratory effort follows the FVC maneuver.
Despite their importance, inspiratory flow rate have been studied almost exclusively by comparing different groups of patients with each other. There are very few reference equations to aid in determining normal ranges.
| Reference: | Value: | Gender: | Age: | Equation: |
| [A] | MIF50% | Male | 21-75 | (1.07 x BSA) – (0.20 x age) + 2.78 |
| [A] | PIF | Male | 21-75 | (1.15 x BSA) – (0.14 x age) + 2.73 |
| [B] | FIV1/FIVC | Male | 18-34 | 77.4 + (7.7 x Ht(M)) – (0.04 x age) |
| [B] | FIV1/FIVC | Male | 35-73 | 107.9 – (3.4 x Ht(M)) – (0.26 x age) |
| [B] | FIV1/FIVC | Female | 18-34 | 60.8 + (20.6 x Ht(M)) – (0.28 x age) |
| [B] | FIV1/FIVC | Female | 35-73 | 121.6 – (14.1 x Ht(M)) – (0.29 x age) |
Probably the biggest problem with using numerical values to assess inspiratory obstruction is that only a small number of patients that meet these criteria actually have upper airway obstruction. One study that evaluated these criteria showed that of 40 patient with a MIF50% < 100 LPM only 3 (7.5%) actually had upper airway obstruction and that of 207 patient with a MEF50%/MIF50% ratio > 1.0 (and <0.3) only 17 (8.2%) had upper airway obstruction.
On the other hand the same study showed that 100% of the patients with a visually abnormal inspiratory flow-volume loop had upper airway obstruction. For this reason, it seems that we really do know upper airway obstruction when we see it and that the contour of the inspiratory flow-volume loop remains the best tool for determining its presence.
The inspiratory flow-volume loop is an important tool for determining the presence of both fixed and variable upper airway obstruction during inspiration. This kind of obstruction can be a result of subglottic stenosis, goiter, Parkinson’s disease, Sarcoidosis, Wegener’s granulamatosis, vocal cord dysfunction, tumors and obstructive sleep apnea. Although numerical analysis of inspiratory flow rates can raise the suspicion of upper airway obstruction visual inspection of the flow-volume loop remains the most accurate approach to assessing test results.
Although inspiratory obstruction is admittedly far less common than expiratory obstruction I’d like to see some acknowledgment from equipment manufacturers that the criteria for selecting an inspiratory flow-volume loop are quite different and possibly in conflict with the selection criteria and possibly even the test procedure for the FVC and FEV1. The ability to mix-and-match inspiratory and expiratory efforts would go a long way towards correcting this problem. I’d like to see the ATS/ERS publish standards for the performance of an FIVC maneuver and indications on how to assess quality and repeatability. I’d also like to see further work on characterizing normal inspiratory flow rates (the FIF25-75 in particular looks interesting and deserves further study) and their LLN because otherwise we are mostly flying by the seat of our pants when we use just the contour of the inspiratory flow-volume loop to diagnose inspiratory airway obstruction.
References:
[A] Bass H. The flow volume loop: Normal standards and abnormalities in Chronic Obstructive Pulmonary Disease. Chest 1973; 63: 171-176.
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of Lung Function Testing. Standarisatio of spirometry. Eur Respir J 2005; 26: 319-338.
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of Lung Function Testing. Interpretive strategies for lung function tests. Eur Respir J 2005; 26: 948-968.
Ewald FW, Tenholder MF, Waller RF. Analysis of the inspiratory flow-volume curve. Should it always preced the forced expiratory maneuver. Chest 1994; 106: 814-818.
[B] Gulsvik A, Tosteson T, Bakke P, Humerfelt S, Weiss ST, Speizer FE. Expiratory and inspiratory forced vital capacity and one-second forced volume in asymptomatic never-smokers in Norway. Clin Physiology 2001; 21(6): 648-660.
Hnafiuk OW, Slade AR. Characterization of the inspiratory flow-volume curve in asymptomatic patients with no known pulmonary disease and normal expiratory spirometry. Chest 1995; 108(3): S187.
Jordanoglou J, Pride NB. A comparison of maximum inspiratory and expiratory flow in health and in lung disease. Thorax 1968; 23: 38-45.
Masumi S, Nishigawa K, Williams AJ, Yan-Go FL, Clark GT. Effect of jaw position and posture on forced inspiratory airflow in normal subjects and patients with obstructive sleep apnea. Chest 1996; 109: 1484-1489.
Modrykamien AM, Gudavalli R, McCarthy K, Liu X, Stoller JK. Detection of upper airway obstruction with spirometry results and the flow-volume loop: A comparison of quantitative and visual inspection criteria. Resp Care 2009; 54(4): 474-479.
Reddy R, Cook T, Tenholder MF. Bronchodilation and the inspiratory flow-volume curve. Chest 1996; 110: 1226-1228.
Rotman HH, Liss HP, Weg JG. Diagnosis of upper airway obstruction by pulmonary function testing. Chest 1975; 68: 796-799.
Sterner JB, Morris MJ, Sill JM, Hayes JA. Inspiratory flow-volume curve exaluation for detecting upper airway disease. Resp Care 2009; 54(4): 461-466.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

Hi Richard,
I’ve been in the field about 45 years and I found the best solution for this problem is to have the patient perform an MVV maneuver as one of the F/V loop trials. If the flattening on the loop is real, the flow rates from the MVV maneuver will not exceed what your saw during normal spirometry. If the flow rates do exceed those flow rates, you know it’s just patient effort. The picture is worth a thousand words. All you have to do is superimpose the trial efforts and you’ll get your answer.
I find the the mid-flow measurements to be useless. It’s the shape of the curve that matters.
Hope this helps,
Very Best,
Ira Bauer RPFT
P.S. Love the blog! Keepup the good work.
Ira –
I hadn’t heard of this technique before but it makes sense. I assume you do this only when you see a suspicious inspiratory loop or are specifically trying to look at inspiratory loops. I can think of one or two test systems where this wouldn’t work since they “automatically” detect the beginning of the inspiratory effort for an FVC maneuver and would stop collecting data at the end of the following inspiratory maneuver so the most you could get in would be two inspiratory loops. Good idea though, and a good way to check the quality of a patient’s effort.
Thanks,
– Richard