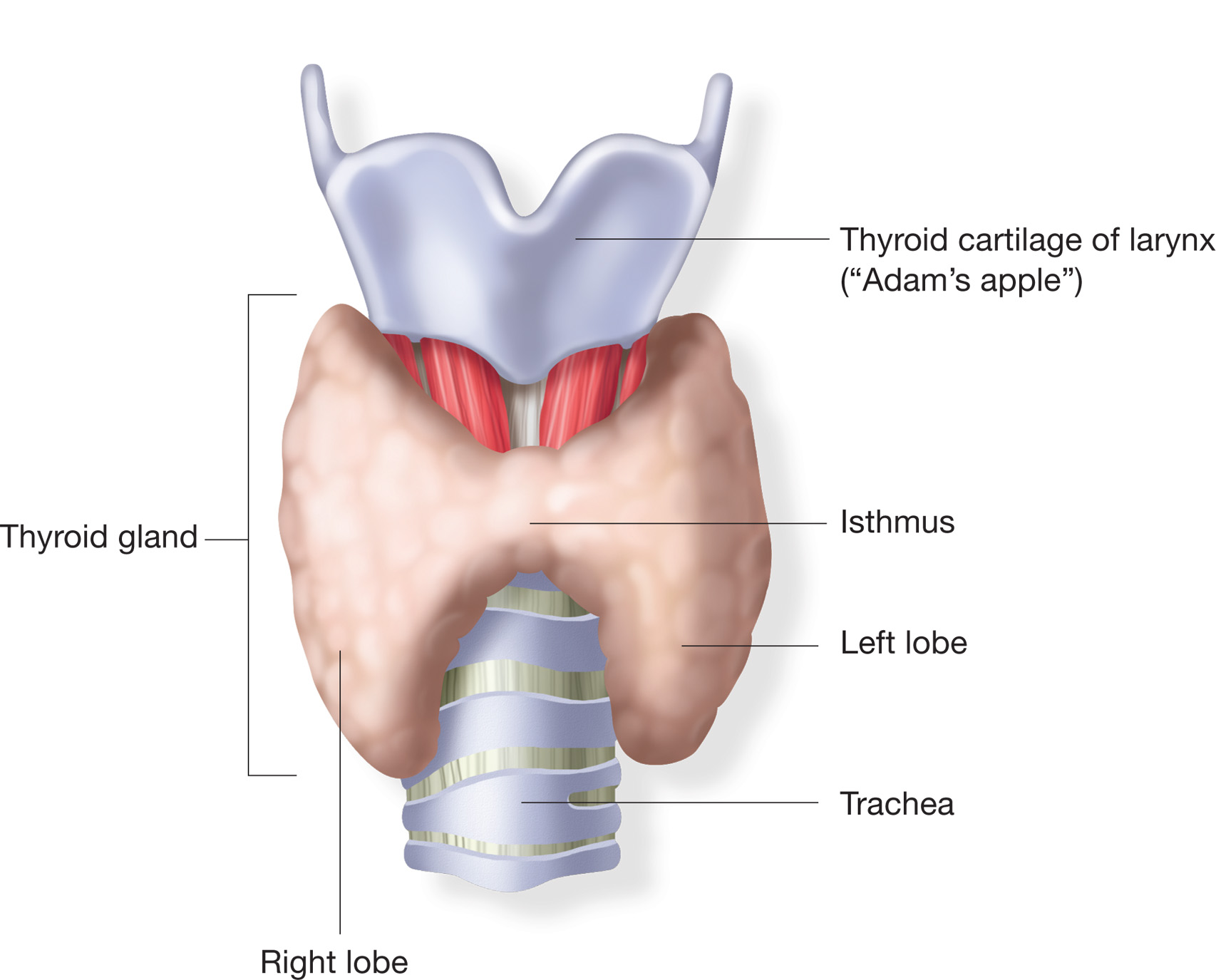
The thyroid gland is located across the front of the upper airway a short distance below the larynx. An enlarged thyroid gland is known as a goiter. The most common worldwide cause of goiter is an iodine deficiency. This is much less common in the western nations where factors such as Hashimoto’s thyroiditis, Graves’ disease, multi-nodular thyroid disease, thyroid cancer, pregnancy and the side effects of some medications are the its primary causes. Common respiratory complaints associated with goiter include cough, hoarseness, shortness of breath and stridor.
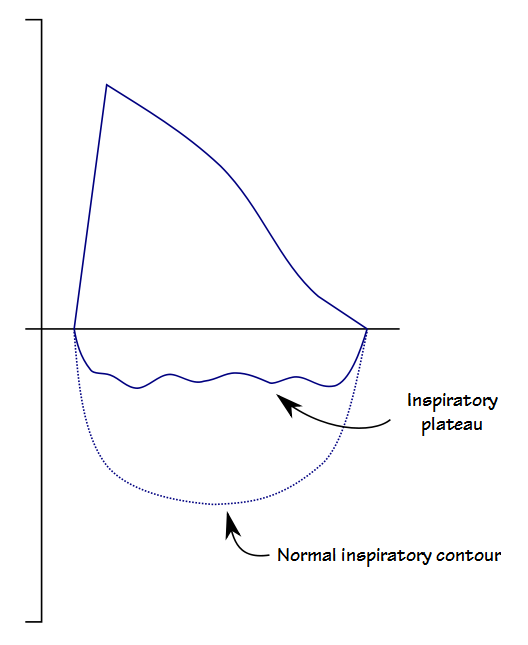
When a goiter is large enough it can press against the trachea and cause a narrowing or deviation of the upper airway. My lab usually gets at least a couple of patients referred to us every year with a diagnosis of goiter and a request that we assess whether it is causing any significant airway obstruction. Decades ago I was taught by my medical director that when this occurs it shows up as an expiratory plateau on a flow-volume loop.
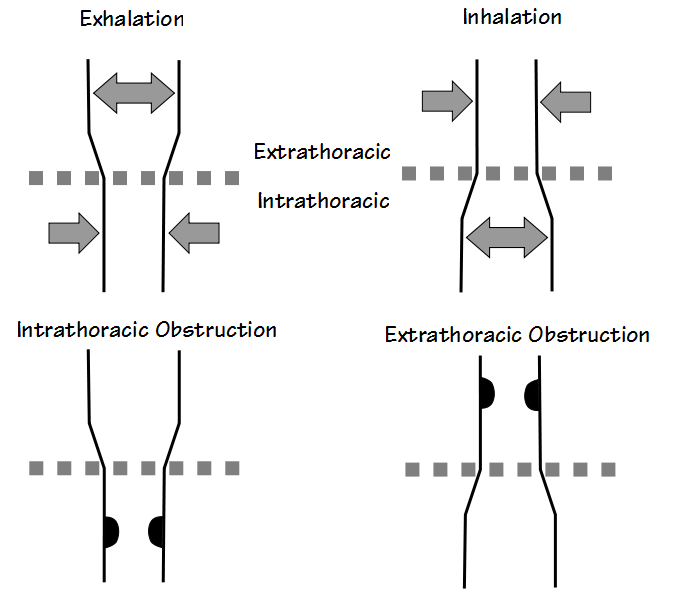
The reality (as usual) is more complex and this is mostly because the thyroid gland lies close to the boundary between the extrathoracic and intrathoracic sections of the trachea. Depending on its size and the which direction the thyroid expands towards, goiter can show up as an extrathoracic or intrathoracic airway obstruction. Even more importantly, as a recent article in Chest showed, the airway obstruction from goiter can be dependent on body position as well.
Note: Interestingly, most of the published studies of goiter and airway obstruction goiter are fairly evenly divided between researchers that detected primarily extrathoracic obstruction and those that detected primarily intrathoracic obstruction. To some extent this appears to be a case of finding what you’re looking for since in many cases only expiratory or only inspiratory parameters are reported.
If the obstruction is intrathoracic, flow limitation will show up as a plateau in flow during exhalation. If it is extrathoracic, flow limitation and a plateau will occur during inhalation. Given the position of the thyroid gland it is also possible for both intrathoracic and extrathoracic flow limitations to be present at the same time.
The effects that extrathoracic and intrathoracic airway obstructions have on flow-volume loops were extensively described by Miller and Hyatt decades ago and the flow-volume loops in their article have been reproduced numerous times since then. The reason for the different flow-volume loop contours is relatively simple however, and has mostly to do with the differences in pressure between the interior of the airway and the surrounding tissue.
During exhalation, the pressure surrounding the airways inside the thorax (intrathoracic) is higher than what is inside the airways and this causes these airways to be narrowed. At the same time, the pressure around the airways outside the thorax (extrathoracic) is lower than what is inside the airways and this causes the airways to widen.
During inhalation, the pressure differences are reversed and this causes the extrathoracic airway to narrow and the intrathoracic airway to widen. Forced inspiratory and expiratory efforts exaggerate this effect. Because a goiter (or tumor or other mass) can press against the airway, this can cause a narrowing that is greater than what is normally expected to occur. Depending on its location this will then show up as a flattening or plateau in either the expiratory or inspiratory portion of the flow-volume loop.
Note: Some goiters extend well into the thorax and sub-sternal goiters have been described in more than one study. These goiters can decrease lung capacity but they are usually detected by imaging (MRI, nuclear medicine uptake scans) and not by lung volume measurements. Changes in FVC, TLC and FRC pre- and post-treatment have occasionally been noted, however.
Flow-volume loops from individuals with goiter are often reasonably normal however but spirometry is also usually performed while sitting upright and a goiter may not narrow the airway enough to affect flow rates in this position. Several studies have shown that some individuals with goiter that had normal flow-volume loops in the upright position showed flattening when they were performed in the supine or lateral positions. Another recent study showed that an individual with goiter that had the Pemberton sign (a somewhat unusual condition where elevating both arms causes venous congestion and cyanosis) also had an expiratory plateau on their flow-volume loop only when their arms were raised.
Interestingly, research has shown that radiological imaging is an unreliable indicator for determining the presence of airway obstruction and flow-volume loops remain the best tool for this purpose. Researchers have used a variety of numerical results such as the MIFR (PIF), the FEV1/PEF ratio and MEF50/MIF50 ratio to assess inspiratory and expiratory flattening. The usefulness of these values is limited however, particularly because their normal variability is high. Visual inspection of the flow-volume loops still seems to be the most accurate way to assess for inspiratory or expiratory flow limitations.
Goiter continues to occur throughout the world for a variety of reasons and upper airway obstruction can be associated with it. One study of a relatively large number of patients referred for thyroid surgery showed that 33% had upper airway obstruction but the actual prevalence amongst all patients with goiter is unknown. For this reasons any individual with goiter, and most particularly those with any respiratory symptoms, should probably be assessed for upper airway obstruction and this should consist of a careful examination of the maximal expiratory and inspiratory flow-volume loops. Individuals with normal flow-volume loops in the upright position should probably also perform supine (and possibly right or left lateral depending on the position of the goiter) spirometry as well, particularly if they complain of orthopnea.
References:
Albareda M, Viguera J, Santiveri C, Lozano P, Mestron A, Bengoa N, Calvet R, Roger A, Pardillo D, Delgado E, Vila LI. Upper airway obstruction in patients with endothoracic goiter enlargement: no relationship between flow-volume loop and radiological tests. Eur J Endocrin 2010; 163: 665-669.
Bright P, Miller MR, Franklyn JA, Sheppard MC. The use of a neural network to detect upper airway obstruction caused by goiter. Am J Respir Crit Care Med 1998; 157: 1885-1891.
Geraghty JG, Coveney EC, Kiernan M, O’Higgins NJ. Flow volume loops in patients with goiters. Ann Surg 1992; 215(1): 83-86.
Gittoes NJL, Miller MR, Daykin J, Sheppard MC. Upper airways obstruction in 153 consecutive patients presenting with thyroid enlargement. BMJ 1996; 312: 484-485.
Karbowitz ST, Edelman LB, Nath S, Dwek JH, Rammohan G. Spectrum of advanced upper airway obstruction due to goiters. Chest 1985; 87(1): 18-21.
Meysman M, Noppen M, Vincken W. Effect of posture on the flow-volume loop in two patients with Euthyroid goiter. Chest 1996; 110: 1615-1618.
Miller RD, Hyatt RE. Evaluation of obstructing lesions of the trachea and larynx by flow-volume loops. Am Rev Respir Dis 1973; 108: 475-481.
Resende PN, Menezes MB, Silva GA, Vianna EO. Pemberton sign. A recommendation to perform arm elevation spirometry with flow-volume loops. Chest 2015; 148(6): e168-e170.
Rios A, Rodriguez JM, Galindo PJ, Cascales PA, Balsalobre M, Parilla P. Spirometric evaluation of respiratory involvement in asymptomatic multinodular goiter with an intrathoracic involvement. Arch Bronconeumol 2008; 44(9): 504-506.
Sterner JB, Morris MJ, Sill JM, Hayes JA. Inspiratory flow-volume curve evaluation for detecting upper airway disease. Resp Care 2009; 54(4): 461-466.
Sugapriya G. Pulmonary function studies in hyperthyroid females with goiter – before and after thyroid surgery. Int J Biol Med Res 2011; 2(3): 661-663.
Torchio R, Gulotta C, Perboni A, Ciacco C, Guglielmo M, Orlandi F, Milic-Emili J. Orthopnea and tidal flow limitation in patients with Euthyroid goiter. Chest 2003; 124(1): 133-140.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License