Oxygen transport between the lungs and the body depends on numerous complex factors. Ventilation and the alveolar-capillary surface area are of course important but a critical component is hemoglobin. Oxygen is poorly soluble in water (which is what blood is mostly made of) and the transportation of oxygen throughout the body would not happen without hemoglobin’s ability to absorb and release oxygen on demand. Although it is possible to measure the diffusing capacity of oxygen (DLO2) the process is technically difficult and not at all suited to routine clinical testing.
There are a number of gases that are able to diffuse across the alveolar-capillary membrane and can be used in a variety of physiological measurements but in order for a particular gas to act as a substitute for oxygen it must be able to interact with hemoglobin. Carbon monoxide (CO) has an affinity for hemoglobin approximately 220 times greater than oxygen and was the first gas used to measure diffusing capacity (DLCO). DLCO has been a routine test for well over 50 years and has been measured by single-breath, steady-state and rebreathing techniques.
Nitric Oxide (NO) has an affinity for hemoglobin about 400 times greater than carbon monoxide (it is generally an irreversible process since the end product is methemoglobin whereas hemoglobin’s binding with CO is more reversible) and for this reason it can also be used to measure diffusing capacity. DLNO can also be measured by single-breath, steady-state and rebreathing techniques. Because of its high affinity and the speed at which the binding of NO to hemoglobin occurs numerous researchers have assumed that DLNO is equivalent to DMNO (the membrane component of diffusing capacity). This is not really true, but it can be a useful fiction and in order to understand why it’s necessary to look at the basic physiology of diffusing capacity tests.
Roughton and Forster’s seminal 1957 paper showed that diffusion is the sum of two resistances. I’ve discussed this previously but specifically:
Where:
DMCO = membrane component
θCO = the rate at which CO binds to hemoglobin
Vc = pulmonary capillary blood volume
The first resistance (1/DMCO) is the resistance to the diffusion of CO through the alveolar-capillary membrane and blood plasma to the surface of the stagnant plasma boundary layer around a red blood cell. The second resistance refers to the diffusion rate of CO through the plasma boundary layer, then the wall and interior of the red blood cell and finally the rate of reaction with hemoglobin.
The same formula applies to DLNO:
θNO however, is relatively large and in fact when its value was initially calculated it came out close to infinity. For this reason, it has been assumed that the value on the right side of the equation [1/θNO x Vc] is exceedingly small and as a shortcut can be assumed to be zero. For this reason many researchers have assumed that DLNO is essentially equal to DMNO.
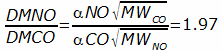
The diffusion rate of gases across the alveolar-capillary membrane is directly proportional to their solubility and inversely proportional to their molecular weight. For this reason, the difference in the membrane component of diffusion for CO and NO is:
Where:
α = solubility coefficient
MW = molecular weight
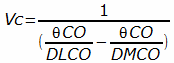
Which means that DMCO can be calculated by multiplying DMNO by 1.97. The reason this is important is that DMCO (and the pulmonary capillary blood volume) are usually calculated using a somewhat time-consuming multi-step process that requires that DLCO be at least measured at two different oxygen concentrations. By measuring DLCO and DLNO simultaneously, it is possible to calculate DMCO and then Vc:
with a single maneuver.
As usual however, things are never that simple. In particular, the assumption that any physiological process occurs infinitely fast is not something that correlates well with reality. Careful followup lab research has shown that θNO is actually much lower than expected, with a value of around 4.5. So why is there such a discrepancy?
First, the original researchers verified their DLNO findings by measuring DMCO via the traditional multi-step technique. The calculation of DMCO is quite sensitive to the value of 1/θCO that is used to calculate it (a well known and continuing problem). The DLNO researchers used Roughton and Forster’s original 1957 value which is known to be flawed (and was re-calculated by Forster in 1987). When DLNO is compared to DMCO using Forster’s updated 1/θCO value, a non-infinite θNO is found and is actually close to the 4.5 value derived from benchtop measurements.
Second, DLNO is essentially insensitive to the arterial oxygen concentration. NO binds directly with oxygenated hemoglobin to form methemoglobin. CO on the other hand competes with oxygen for binding sites on hemoglobin and its binding rate is therefore inversely proportional to arterial PO2.
Third, DLNO is relatively insensitive to pulmonary capillary blood volume which is partly because of how it binds to hemoglobin but also due to the details of the DLNO test. NO at high concentrations is toxic because of its rapid conversion to NO2. For this reason, an NO concentration of 40-45 ppm is usually used for the inspired gas mixture (and is considered reasonably safe because smokers inhale higher NO concentrations from cigarettes). This very small concentration of NO means that only tiny amounts of hemoglobin are involved in the uptake of NO and for this reason NO uptake is unchanged over a very broad range of hemoglobin concentrations and pulmonary capillary blood volumes.
Finally, even though NO’s reaction rate with hemoglobin is not infinitely fast, it is still substantially faster than that for CO. This means that the DMNO/DLNO ratio is substantially larger than the DMCO/DLCO ratio and that DLNO can in some circumstances be considered to be a reasonable substitute for DMNO (and DMCO). But reasonable substitute in this case means conceptually more than as a measurable property. The mathematical relationship between DMNO and DMCO depends greatly on which θCO and θNO constants are used, and there are at least seven different sets of constants for CO as well as several sets for NO. Unfortunately, this problem calls into question the results and conclusions of many research studies.
The value of DLNO is that it is primarily sensitive to the lung’s functional surface area and relatively insensitive to PaO2, hemoglobin concentration and pulmonary capillary blood volume. For this reason, a number of researchers have proposed using the DLNO/DLCO ratio rather than trying to use DLNO to estimate DMCO and Vc.
Since the DLNO/DLCO ratio combines diffusing capacity for two different gases with different physiological properties, it has the potential to be more informative than just DLCO or DLNO alone. DLNO, Vc and the DLNO/DLCO ratio have been studied and have provided insights into emphysema, pulmonary hypertension, diffuse interstitial disease, cystic fibrosis, obesity, systemic sclerosis, hepatopulmonary syndrome and the effects of methotrexate, bleomycin, exercise, and high altitude. Notably, the DLNO/DLCO ratio tends to rise when lung disease is present primarily because DLCO usually decreases more than DLNO. Interestingly DLNO/DLCO decreases during exercise and in some patients with sarcoid, and it’s predicted to decrease in the early stages of CHF (a confounding problem however, is that the DLNO/DLCO ratio decreases when DLCO and DLNO are measured below TLC so test quality is an important factor).
A key question however, has to be whether DLNO and the DLNO/DLCO ratio are clinically relevant. The answer is that although they can provide useful physiological information, it isn’t at all clear that DLNO significantly improves either the diagnosis or the monitoring of lung diseases at this time. There is a great deal of overlap in DLNO/DLCO ratios between dissimilar lung diseases and there are no longitudinal studies that would show changes in DLNO and the DLNO/DLCO ratio over time. The potential is certainly there but DLNO measurement techniques, normal ranges and derived values need to be standardized and there needs to be clear clinical guidelines in its use.
Note: For those who are feeling clinically adventurous Medisoft has two PFT systems (Hypair Compact, BodyBox 5500) that offer DLNO testing as an option.
The nitric oxide diffusing capacity (DLNO) can be measured using much the same techniques, equipment and mathematics that are used for DLCO testing. Initial research appeared to show that DLNO could be used to quickly and easily derive DMCO and Vc. Many researchers still follow this convention despite the fact that this has since been shown to be incorrect. The DLNO measurement however, is dominated by the membrane component of conductance and for this reason is more sensitive to the lung’s functional surface area than is DLCO, while DLCO is more sensitive to hemoglobin and the pulmonary capillary blood volume. These characteristics suggest that differences in DLCO and DLNO have the potential to provide useful diagnostic information.
UPDATE: Standards for DLNO testing were released in the February 2017 issue of the European Respiratory Journal. This is discussed in 2017 ERS DLNO Standards.
References:
Borland CRR, Higenbottam TW. A simultaneous single breath measurement of pulmonary diffusing capacity with nitric oxide and carbon monoxide. Eur Respir J 1989; 2: 56-63.
Borland C, Mist B, Zammit M, Vuylsteke A. Steady-state measurement of NO and CO lung diffusing capacity on moderate exercise in men. J Appl Physiol 2001; 90: 538-544.
Borland CDR, Dunningham H, Bottrill F, Vuylsteke A, Yilmaz C, Dane DM, Hsia CCW. Significant blood resistance to nitric oxide transfer in the lung. J Appl Physiol 2010; 108: 1052-1060.
Degano B, Mittaine M, Guenard H, Rami J, Garcia G, Kamar N, Bureau C, Peron JM, Rostaing L, Riviere D. Nitric oxide and carbon monoxide lung transfer in patients with advanced liver cirrhosis. J Appl Physiol 2009; 107: 139-143.
Farha S, Laskowski D, George D, Park MM, Tang WHW, Dweik RA, Erzurum SC. Loss of alveolar membrane diffusing capacity and pulmonary capillary blood volume in pulmonary arterial hypertension. Resp Research 2013; 4:6
Glenet SN, De Bisschop C, Vargas F, Guenard HJP. Deciphering the nitric oxide to carbon monoxide lung transfer ratio: physiological implications. J Physiol 2007 582.2: 767-775.
Hughes JMB, van der Lee I. The TL,NO/TL,CO ration in pulmonary test interpretation. Eur Respir J 2013; 41: 453-461.
Martinot JB, Mule M, de Bisschop C, Overbeek MJ, Le-Dong NN, Naeije R, Guenard H. Lung membrane conductance and capillary volume derived from the NO and CO transfer in high-altitude newcomers. J Appl Physiol 2013; 115: 157-166.
Meyer M, Piiper J. Nitric oxide (NO), a new test gas for study of alveolar-capillary diffusion. Eur Respir J 1989; 2: 494-496.
Meyer M, Schuster KD, Schulz H, Mohr M, Piiper J. Pulmonary diffusing capacities for nitric oxide and carbon monoxide determined by rebreathing in dogs. J Appl Physiol 1990; 68(6): 2344-2357.
Perillo IB, Hyde RW, Olszowka AJ, Pietropaoli AP, Frasier LM, Torres, A, Perkins PT, Forster RE, Utell MJ, Frmpton MW. Chemiluminescent measurements of nitric oxide pulmonary diffusing capacity and alveolar production in humans. J Appl Physiol 2001; 91: 1931-1940.
Roughton FJW, Forster RE. Relative importance of diffusion and chemical reaction rates in determining the rate of exchange of gases in the human lung, with special reference to true diffusing capacity of the pulmonary membrane and volume of blood in lung capillaries. J Appl
Physiol 1957; 11: 290 –302.
Sivova N, et al. Relevance of partitioning DLCO to detect pulmonary hypertension in systemic sclerosis. PLOS ONE 2013; 8(10): e78001.
Tamhane RM, Johnson RL, Hsia CCW. Pulmonary membrane diffusing capacity and capillary blood volume measured during exercise from nitric oxide uptake. Chest 2001; 120: 1850-1856.
van der Lee O, Zanen P, Grutters JC, Snijder RJ, van den Bosch JMM. Diffusing capacity for nitric oxide and carbon monoxide in patients with diffuse parenchymal lung disease and pulmonary arterial hypertension. Chest 2006; 129: 378-383.
van der Lee I, Zanen P, Stigter N, van der Bosch J, Lammers JWJ. Diffusing capacity for nitric oxide: reference values and dependence of alveolar volume. Respiratory Medicine 2007; 10: 1579-1584.
van der Lee I, Gietema HA, Zanen P, van Klaveren RJ, Prokop M, Lammers JWJ, van den Bosch JMM. Nitric oxide diffusing capacity versus spirometry in the early diagnosis of emphysema in smokers. Respiratory Medicine 2009; 103: 1892-1897.
Viart-Ferber C, Couraud S, Gormand F, Pacheco Y. Combined lung transfer of NO and CO in patients reveicing methotrexate or bleomycin therapy compared to normal subjects. Physiol J 2013; Article ID 539076.
Wheatley CM, Foxx-Lupo WT, Cassuto NA, Wong EC, Daines CL, Morgan WJ, Snyder EM. Impaired lung diffusing capacity for nitric oxide and alveolar-capillary membrane conductance results in oxygen desaturation during exercise patients with cystic fibrosis. J Cystic Fibrosi 2011; 10: 45-53.
Zavorsky GS, Quiron KB, Massarelli PS, Lands LC. The relationship between single-breath diffusion capacity of the lung for nitric oxide and carbon monoxide during various exercise intensities. Chest 2004; 125: 1019-1027.
Zavorsky GS, Kim DJ, McGregor ER, Starling JM, Gavard JA. Pulmonary diffusing capacity during exercise in morbid obesity. Obesity 2008; 16: 2431-2438.
Zavorsky GS. No red cell resistance to NO? I think not! J Appl Physiol 2010; 108: 1027-1029.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License


Hi Richard,
Excellent blog, as usual, and very important to understand. As you know, there are some companies selling equipment that does DLNO, claiming it can separate DM from VC. Forester himself wrote about this many years later and questioned the importance of his own equation. Simply put, you can’t measure DM and VC separately because they are interdependent — they are like Siamese Twins, or row houses with a common wall. However, you can’t calculate DM without Hb. Therefore, the clinical usefulness comes into question.
Very Best,
Ira
Ira –
Given the problems with 1/theta constants for CO and NO I won’t say I ignore research findings on DM and Vc but I do take them with a big grain of salt. Since DLNO and DLCO highlight different aspects of the diffusion process I’d have thought that the differences across the spectrum of lung diseases and conditions would be more distinct, but as of yet this does not seem to be the case. Still hopeful however, that somebody will notice something about DLNO/DLCO that isn’t apparent right now.
Regards, Richard